Abstract
Purpose
To investigate the effectiveness and risks of different surgical therapies for isthmocele in symptomatic women with abnormal uterine bleeding, infertility, or for the prevention of obstetric complications, considering safety and surgical complications.
Methods
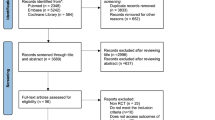
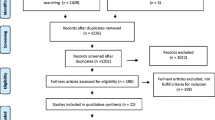
PubMed/MEDLINE, Scopus, Embase, Science Direct, and Cochrane Library were systematically searched (n° CRD4201912035) for original articles on the surgical treatment of isthmocele published between 1950 and 2018. Data synthesis was completed using MedCalc 16.4.3. The body of evidence was assessed using the GRADE methodology.
Results
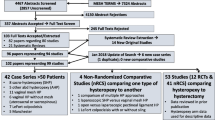
We retrieved 33 publications: 28 focused on a single surgical technique, and five comparing different techniques. Meta-analysis showed an improvement of symptoms in 85.00% (75.05–92.76%) of women after hysteroscopic correction, 92.77% (85.53–97.64%) after laparoscopic/robotic correction, and 82.52% (67.53–93.57%) after vaginal correction. Hysteroscopic surgery was associated with the lowest risk of complications (0.76%, 0.20–1.66%).
Conclusions
We found adequate evidence supporting the use of surgery for the treatment of symptomatic isthmocele, as it was found to improve the bleeding symptoms in more than 80% of patients. Differently, we found a lack of evidence regarding the role of surgery with the purpose of improving fertility or reducing the risk of obstetric complications in women with asymptomatic isthmocele. The hysteroscopic correction of isthmocele may be the safest and most effective strategy in those patients with adequate residual myometrial thickness overlying the isthmocele. Laparoscopic and vaginal surgeries may be the preferred options for patients with a thinner residual myometrium over the defect (< 2.5 mm) and when hysteroscopic treatment is inconclusive.


Adapted from Gubbini et al. [31]


Retrieved from Donnez et al. [28]


Adapted from Chen et al. [50]



Similar content being viewed by others
References
Menacker F, Declercq E, Macdorman MF (2006) Cesarean delivery: background, trends, and epidemiology. Semin Perinatol 30:235–241
Clark SL, Koonings PP, Phelan JP (1985) Placenta previa/accreta and prior cesarean section. Obs Gynecol 66:89–92
Monteagudo A, Carreno C, Timor-Tritsch IE (2001) Saline infusion sonohysterography in nonpregnant women with previous cesarean delivery: the “niche” in the scar. J Ultrasound Med 20:1105–1115
Fabres C, Aviles G, De la Jara C et al (2003) The cesarean delivery scar pouch: clinical implications and diagnostic correlation between transvaginal sonography and hysteroscopy. J Ultrasound Med 22:695–700. https://doi.org/10.7863/jum.2003.22.7.695
Morris H (1995) Surgical pathology of the lower uterine segment caesarean section scar: Is the scar a source of clinical symptoms? Int J Gynecol Pathol 14:16–20. https://doi.org/10.1097/00004347-199501000-00004
Florio P, Filippeschi M, Moncini I et al (2012) Hysteroscopic treatment of the cesarean-induced isthmocele in restoring infertility. Curr Opin Obstet Gynecol 24:180–186
Borges LM, Scapinelli A, de Baptista DD et al (2010) Findings in patients with postmenstrual spotting with prior cesarean section. J Minim Invasive Gynecol 17:361–364. https://doi.org/10.1016/j.jmig.2010.02.007
Wang CB, Chiu WWC, Lee CY et al (2009) Cesarean scar defect: correlation between Cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet Gynecol 34:85–89. https://doi.org/10.1002/uog.6405
Uppal T, Lanzarone V, Mongelli M (2011) Sonographically detected caesarean section scar defects and menstrual irregularity. J Obstet Gynaecol (Lahore) 31:413–416. https://doi.org/10.3109/01443615.2011.577252
Thurmond AS, Harvey WJ, Smith SA (1999) Cesarean section scar as a cause of abnormal vaginal bleeding: diagnosis by sonohysterography. J Ultrasound Med 18:13–16. https://doi.org/10.7863/jum.1999.18.1.13
Bij De Vaate AJM, Van Der Voet LF, Naji O et al (2014) Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound Obstet Gynecol 43:372–382. https://doi.org/10.1002/uog.13199
Fabres C, Arriagada P, Fernández C et al (2005) Surgical treatment and follow-up of women with intermenstrual bleeding due to cesarean section scar defect. J Minim Invasive Gynecol 12:25–28. https://doi.org/10.1016/j.jmig.2004.12.023
Başbuğ A, Doğan O, Ellibeş Kaya A et al (2018) Does suture material affect uterine scar healing after Cesarean section? Results from a randomized controlled trial. J Invest Surg. https://doi.org/10.1080/08941939.2018.1458926
Stegwee SI, Jordans I, van der Voet LF et al (2018) Uterine caesarean closure techniques affect ultrasound findings and maternal outcomes: a systematic review and meta-analysis. BJOG 125:1097–1108. https://doi.org/10.1111/1471-0528.15048
Fischer RJ (2006) Symptomatic cesarean scar diverticulum. J Reprod Med 51:742–744
Vikhareva Osser O, Jokubkiene L, Valentin L (2010) Cesarean section scar defects: agreement between transvaginal sonographic findings with and without saline contrast enhancement. Ultrasound Obstet Gynecol 35:75–83. https://doi.org/10.1002/uog.7496
Antila-Långsjö R, Mäenpää JU, Huhtala H et al (2018) Comparison of transvaginal ultrasound and saline contrast sonohysterography in evaluation of cesarean scar defect: a prospective cohort study. Acta Obstet Gynecol Scand 97:1130–1136. https://doi.org/10.1111/aogs.13367
Ludwin A, Martins WP, Ludwin I (2019) Evaluation of uterine niche by three-dimensional sonohysterography and volumetric quantification: techniques and scoring classification system. Ultrasound Obstet Gynecol 53:139–143. https://doi.org/10.1002/uog.19181
Jordans IPM, de Leeuw RA, Stegwee SI et al (2019) Sonographic examination of uterine niche in non-pregnant women: a modified Delphi procedure. Ultrasound Obstet Gynecol 53:107–115. https://doi.org/10.1002/uog.19049
Gubbini G, Centini G, Nascetti D et al (2011) Surgical hysteroscopic treatment of Cesarean-induced isthmocele in restoring fertility: prospective study. J Minim Invasive Gynecol 18:234–237. https://doi.org/10.1016/j.jmig.2010.10.011
Laganà AS, Palmara V, Granese R et al (2014) Desogestrel versus danazol as preoperative treatment for hysteroscopic surgery: a prospective, randomized evaluation. Gynecol Endocrinol 30:794–797. https://doi.org/10.3109/09513590.2014.929658
Laganà AS, Vitale SG, Muscia V et al (2017) Endometrial preparation with Dienogest before hysteroscopic surgery: a systematic review. Arch Gynecol Obstet 295:661–667. https://doi.org/10.1007/s00404-016-4244-1
Florio P, Imperatore A, Litta P et al (2010) The use of nomegestrol acetate in rapid preparation of endometrium before operative hysteroscopy in pre-menopausal women. Steroids 75:912–917. https://doi.org/10.1016/j.steroids.2010.05.009
Tahara M, Shimizu T, Shimoura H (2006) Preliminary report of treatment with oral contraceptive pills for intermenstrual vaginal bleeding secondary to a cesarean section scar. Fertil Steril 86:477–479. https://doi.org/10.1016/j.fertnstert.2006.01.020
Florio P, Gubbini G, Marra E et al (2011) A retrospective case–control study comparing hysteroscopic resection versus hormonal modulation in treating menstrual disorders due to isthmocele. Gynecol Endocrinol 27:434–438. https://doi.org/10.3109/09513590.2010.495431
Vervoort A, van der Voet LF, Hehenkamp W et al (2018) Hysteroscopic resection of a uterine caesarean scar defect (niche) in women with postmenstrual spotting: a randomised controlled trial. BJOG 125:326–334. https://doi.org/10.1111/1471-0528.14733
Zhang X, Yang M, Wang Q et al (2016) Prospective evaluation of five methods used to treat cesarean scar defects. Int J Gynecol Obstet 134:336–339. https://doi.org/10.1016/j.ijgo.2016.04.011
Donnez O, Jadoul P, Squifflet J, Donnez J (2008) Laparoscopic repair of wide and deep uterine scar dehiscence after cesarean section. Fertil Steril 89:974–980. https://doi.org/10.1016/j.fertnstert.2007.04.024
Chang Y, Tsai EM, Long CY et al (2009) Resectoscopic treatment combined with sonohysterographic evaluation of women with postmenstrual bleeding as a result of previous cesarean delivery scar defects. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2008.11.038
Raimondo G, Grifone G, Raimondo D et al (2015) Hysteroscopic treatment of symptomatic cesarean-induced isthmocele: a prospective study. J Minim Invasive Gynecol 22:297–301. https://doi.org/10.1016/j.jmig.2014.09.011
Gubbini G, Casadio P, Marra E (2008) Resectoscopic correction of the “isthmocele” in women with postmenstrual abnormal uterine bleeding and secondary infertility. J Minim Invasive Gynecol 15:172–175. https://doi.org/10.1016/j.jmig.2007.10.004
Tanimura S, Funamoto H, Hosono T et al (2015) New diagnostic criteria and operative strategy for cesarean scar syndrome: endoscopic repair for secondary infertility caused by cesarean scar defect. J Obstet Gynaecol Res 41:1363–1369. https://doi.org/10.1111/jog.12738
Marotta ML, Donnez J, Squifflet J et al (2013) Laparoscopic repair of post-cesarean section uterine scar defects diagnosed in nonpregnant women. J Minim Invasive Gynecol 20:386–391. https://doi.org/10.1016/j.jmig.2012.12.006
Donnez O, Donnez J, Orellana R, Dolmans M-M (2017) Gynecological and obstetrical outcomes after laparoscopic repair of a cesarean scar defect in a series of 38 women. Fertil Steril 107:289–296.e2. https://doi.org/10.1016/j.fertnstert.2016.09.033
Vervoort A, Vissers J, Hehenkamp W et al (2018) The effect of laparoscopic resection of large niches in the uterine caesarean scar on symptoms, ultrasound findings and quality of life: a prospective cohort study. BJOG 125:317–325. https://doi.org/10.1111/1471-0528.14822
Lin YH, Hwang JL, Seow KM (2010) Endometrial ablation as a treatment for postmenstrual bleeding due to cesarean scar defect. Int J Gynecol Obstet 111:88–89. https://doi.org/10.1016/j.ijgo.2010.05.013
Urman B, Arslan T, Aksu S, Taskiran C (2016) Laparoscopic repair of cesarean scar defect “isthmocele”. J Minim Invasive Gynecol 23:857–858. https://doi.org/10.1016/j.jmig.2016.03.012
Akdemir A, Sahin C, Ari SA et al (2018) Determination of isthmocele using a foley catheter during laparoscopic repair of Cesarean scar defect. J Minim Invasive Gynecol 25:21–22. https://doi.org/10.1016/j.jmig.2017.05.017
Yalcinkaya TM, Akar ME, Kammire LD et al (2011) Robotic-assisted laparoscopic repair of symptomatic cesarean scar defect: a report of two cases. J Reprod Med 56:265–270
Feng YL, Li MX, Liang X, Li XM (2012) Hysteroscopic treatment of postcesarean scar defect. J Minim Invasive Gynecol 19:498–502. https://doi.org/10.1016/j.jmig.2012.03.010
Pérez-Medina T, Sancho-Saúco J, Ríos M et al (2014) Hysteroscopy in pregnancy-related conditions: descriptive analysis in 273 patients. J Minim Invasive Gynecol 21:417–425. https://doi.org/10.1016/j.jmig.2013.11.004
Xie H, Wu Y, Yu F et al (2014) A comparison of vaginal surgery and operative hysteroscopy for the treatment of cesarean-induced isthmocele: a retrospective review. Gynecol Obstet Invest 77:78–83
Li C, Guo Y, Liu Y et al (2014) Hysteroscopic and laparoscopic management of uterine defects on previous cesarean delivery scars. J Perinat Med 42:363–370. https://doi.org/10.1515/jpm-2013-0081
Wang CJ, Huang HJ, Chao A et al (2011) Challenges in the transvaginal management of abnormal uterine bleeding secondary to cesarean section scar defect. Eur J Obstet Gynecol Reprod Biol 154:218–222. https://doi.org/10.1016/j.ejogrb.2010.10.016
Jeremy B, Bonneau C, Guillo E et al (2013) Uterine ishtmique transmural hernia: results of its repair on symptoms and fertility. Gynecol Obstet Fertil 41:588–596. https://doi.org/10.1016/j.gyobfe.2013.08.005
Nirgianakis K, Oehler R, Mueller M (2016) The Rendez–vous technique for treatment of caesarean scar defects: a novel combined endoscopic approach. Surg Endosc 30:770–771. https://doi.org/10.1007/s00464-015-4226-6
Liu S-J, Lv W, Li W (2016) Laparoscopic repair with hysteroscopy of cesarean scar diverticulum. J Obstet Gynaecol Res 42:1719–1723. https://doi.org/10.1111/jog.13146
Luo L, Niu G, Wang Q et al (2012) Vaginal repair of Cesarean section scar diverticula. J Minim Invasive Gynecol 19:454–458. https://doi.org/10.1016/j.jmig.2012.03.012
Klemm P, Koehler C, Mangler M et al (2005) Laparoscopic and vaginal repair of uterine scar dehiscence following cesarean section as detected by ultrasound. J Perinat Med 33:324–331. https://doi.org/10.1515/JPM.2005.058
Chen Y, Chang Y, Yao S (2014) Transvaginal management of cesarean scar section diverticulum: a novel surgical treatment. Med Sci Monit 20:1395–1399. https://doi.org/10.12659/MSM.890642
Zhou X, Yao M, Zhou J et al (2017) Defect width: the prognostic index for vaginal repair of cesarean section diverticula. Arch Gynecol Obstet 295:623–630. https://doi.org/10.1007/s00404-016-4245-0
Chen H, Wang H, Zhou J et al (2019) Vaginal repair of Cesarean section scar diverticula diagnosed in non-pregnant women. J Minim Invasive Gynecol 26:526–534. https://doi.org/10.1016/j.jmig.2018.06.012
Zhou J, Yao M, Wang H et al (2016) Vaginal repair of cesarean section scar diverticula that resulted in improved postoperative menstruation. J Minim Invasive Gynecol 23:969–978. https://doi.org/10.1016/j.jmig.2016.06.013
Schepker N, Garcia-Rocha G-J, von Versen-Höynck F et al (2015) Clinical diagnosis and therapy of uterine scar defects after caesarean section in non-pregnant women. Arch Gynecol Obstet 291:1417–1423. https://doi.org/10.1007/s00404-014-3582-0
Pomorski M, Fuchs T, Rosner-Tenerowicz A, Zimmer M (2017) Sonographic evaluation of surgical repair of uterine cesarean scar defects. J Clin Ultrasound 45:455–460. https://doi.org/10.1002/jcu.22449
Di Spiezio Sardo A, Vieira MDC, Laganà AS et al (2017) Combined systemic and hysteroscopic intra-amniotic injection of methotrexate associated with hysteroscopic resection for cervical pregnancy: a cutting-edge approach for an uncommon condition. Eurasian J Med 49:66–68. https://doi.org/10.5152/eurasianjmed.2017.16215
Bakavičiūtė G, Špiliauskaitė S, Meškauskienė A, Ramašauskaitė D (2016) Laparoscopic repair of the uterine scar defect—successful treatment of secondary infertility: a case report and literature review. Acta Med Litu 23:227–231. https://doi.org/10.6001/actamedica.v23i4.3424
Vitale SG, Sapia F, Rapisarda AMC et al (2017) Hysteroscopic morcellation of submucous myomas: a systematic review. Biomed Res Int 2017:6848250. https://doi.org/10.1155/2017/6848250
Amer-Cuenca JJ, Marín-Buck A, Vitale SG et al (2019) Non-pharmacological pain control in outpatient hysteroscopies. Minim Invasive Ther Allied Technol. https://doi.org/10.1080/13645706.2019.1576054
Laganà AS, Pacheco LA, Tinelli A et al (2018) Optimal timing and recommended route of delivery after hysteroscopic management of isthmocele? A consensus statement from the global congress on hysteroscopy scientific committee. J Minim Invasive Gynecol 25:558. https://doi.org/10.1016/j.jmig.2018.01.018
D’Antonio F, Timor-Tritsch IE, Palacios-Jaraquemada J et al (2018) First-trimester detection of abnormally invasive placenta in high-risk women: systematic review and meta-analysis. Ultrasound Obstet Gynecol 51:176–183. https://doi.org/10.1002/uog.18840
Calì G, Timor-Tritsch IE, Palacios-Jaraquemada J et al (2018) Outcome of Cesarean scar pregnancy managed expectantly: systematic review and meta-analysis. Ultrasound Obstet Gynecol 51:169–175. https://doi.org/10.1002/uog.17568
Funding
Any fund/grant did not support the work.
Author information
Authors and Affiliations
Contributions
SGV: project development and manuscript writing. AL: manuscript writing. GAV: manuscript editing. PT: data collection and management. JT: manuscript editing. AV: manuscript editing, and data collection and management. RBL: data collection and management, and manuscript editing. BC: manuscript writing, project supervision, and final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent is not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vitale, S.G., Ludwin, A., Vilos, G. et al. From hysteroscopy to laparoendoscopic surgery: what is the best surgical approach for symptomatic isthmocele? A systematic review and meta-analysis. Arch Gynecol Obstet 301, 33–52 (2020). https://doi.org/10.1007/s00404-020-05438-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05438-0