Abstract
Purpose
Ovarian cancer (OC) is first gynaecologic cancer that causes women death and epithelial ovarian cancer (EOC) is the most lethal ovarian cancer type. While treatment is commonly successful, some cases (10–20%) show resistance to chemotherapy which is followed by recurrence. MicroRNA (miRNA) based diagnosis methods are slightly important for recurrent ovarian cancer diagnosis. We aimed to detect novel circulating miRNAs to be used as an early diagnosis and prediction tools for recurrent EOC.
Methods
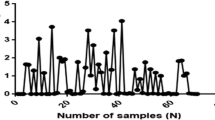
In this study, recurrent EOC serum samples and healthy control serum samples were compared for miRNA expression analysis by microarray. Microarray results were analyzed by bioinformatics tools and differentially expressed hsa-miR-1273g-3p was obtained. After microarray analysis, differentially expressed hsa-miR-1273g-3p was validated by Real-Time PCR (RT-qPCR). The relation between target genes of hsa-miR-1273g-3p and ovarian cancer were examined by Pathway Studio® (v.11.4.0.8).
Results
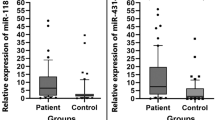
The expression of hsa-miR-1273g-3p was found to be significantly down-regulated by t test Bonferroni FWER corrected p < 0.05 and fold change > 2, in recurrence EOC compare with healthy controls groups. The RT-qPCR results confirmed that relative expressions of the serum hsa-miR-1273g-3p were significantly down-regulated in patients with recurrent EOC (p = 0.0275). Serum hsa-miR-1273g-3p levels could discriminate patients with recurrent EOC from healthy controls, with a power area under the curve (AUC) of 0.7.
Conclusion
This study suggested that hsa-miR-1273g-3p plays a significant role in regulation of related genes, which are TNF-alfa, COL1A1, MMP-2, MMP-9, with recurrent EOC outcome. hsa-miR-1273g-3p may be used as a prognostic marker for recurrent EOC after chemotherapy.




Similar content being viewed by others
References
Nakamura K, Sawada K, Yoshimura A, Kinose Y, Nakatsuka E, Kimura T (2016) Clinical relevance of circulating cell-free microRNAs in ovarian cancer. Mol Cancer 15(1):48. https://doi.org/10.1186/s12943-016-0536-0
Chong GO, Jeon HS, Han HS, Son JW, Lee YH, Hong DG, Lee YS, Cho YL (2015) Differential microRNA expression profiles in primary and recurrent epithelial ovarian cancer. Anticancer Res 35(5):2611–2617
Laios A, O’Toole S, Flavin R, Martin C, Kelly L, Ring M, Finn SP, Barrett C, Loda M, Gleeson N, D’Arcy T, McGuinness E, Sheils O, Sheppard B, Ol J (2008) Potential role of miR-9 and miR-223 in recurrent ovarian cancer. Mol Cancer 7:35. https://doi.org/10.1186/1476-4598-7-35
Retamales-Ortega R, Oróstica L, Vera C, Cuevas P, Hernández A, Hurtado I, Vega M, Romero C (2017) Role of nerve growth factor (NGF) and miRNAs in epithelial ovarian cancer. Int J Mol Sci 18:507. https://doi.org/10.3390/ijms18030507
Molasy M, Walczak A, Szaflik J, Szaflik JP, Majsterek I (2017) MicroRNAs in glaucoma and neurodegenerative diseases. J Hum Genet 62(1):105–112. https://doi.org/10.1038/jhg.2016.91
Barwari T, Joshi A, Mayr M (2016) MicroRNAs in cardiovascular disease. J Am Coll Cardiol 68(23):2577–2584. https://doi.org/10.1016/j.jacc.2016.09.945
Vienberg S, Geiger J, Madsen S, Dalgaard LT (2017) MicroRNAs in metabolism. Acta Physiol (Oxf) 219(2):346–361. https://doi.org/10.1111/apha.12681
Reddy KB (2015) MicroRNA (miRNA) in cancer. Cancer Cell Int 15:38. https://doi.org/10.1186/s12935-015-0185-1
Ruan K, Fang X, Ouyang G (2009) MicroRNAs: novel regulators in the hallmarks of human cancer. Cancer Lett 285(2):116–126. https://doi.org/10.1016/j.canlet.2009.04.031
Cochrane DR, Spoelstra NS, Howe EN, Nordeen SK, Richer JK (2009) MicroRNA-200c mitigates invasiveness and restores sensitivity to microtubule-targeting chemotherapeutic agents. Mol Cancer Ther 8(5):1055–1066. https://doi.org/10.1158/1535-7163.MCT-08-1046
James A, Daley CM, Greiner KA (2011) “Cutting” on cancer: attitudes about cancer spread and surgery among primary care patients in the USA. Soc Sci Med 73(11):1669–1673. https://doi.org/10.1016/j.socscimed.2011.09.017
Gumusoglu E, Gunel T (2018) The role of circulating biomarkers in the early diagnosis of ovarian cancer. Ovarian Cancer (in press)
Chang B, Liu G, Xue F, Rosen DG, Xiao L, Wang X, Liu J (2009) ALDH1 expression correlates with favorable prognosis in ovarian cancers. Mod Pathol 22(6):817–823. https://doi.org/10.1038/modpathol.2009.35
Yang H, Kong W, He L, Zhao JJ, O’Donnell JD, Wang J, Wenham RM, Coppola D, Kruk PA, Nicosia SV, Cheng JQ (2008) MicroRNA expression profiling in human ovarian cancer: miR-214 induces cell survival and cisplatin resistance by targeting PTEN. Cancer Res 68(2):425–433. https://doi.org/10.1158/0008-5472.CAN-07-2488
Ivashchenko A, Berillo O, Pyrkova A, Niyazova R (2014) Binding sites of miR-1273 family on the mRNA of target genes. Biomed Res Int 2014:620530. https://doi.org/10.1155/2014/620530
Cha SY, Choi YH, Hwang S, Jeong JY, An HJ (2017) Clinical impact of microRNAs associated with cancer stem cells as a prognostic factor in ovarian carcinoma. J Cancer 8(17):3538–3547. https://doi.org/10.7150/jca.20348
Ye Z, Li ZH, He SZ (2017) miRNA-1273g-3p involvement in development of diabetic retinopathy by modulating the autophagy-lysosome pathway. Med Sci Monit 23:5744–5751
Balkwill F (2002) Tumor necrosis factor or tumor promoting factor? Cytokine Growth Factor Rev 13(2):135–141
Kwong J, Chan FL, Wong KK, Birrer MJ, Archibald KM, Balkwill FR, Berkowitz RS, Mok SC (2009) Inflammatory cytokine tumor necrosis factor alpha confers precancerous phenotype in an organoid model of normal human ovarian surface epithelial cells. Neoplasia 11(6):529–541
Naylor MS, Stamp GW, Foulkes WD, Eccles D, Balkwill FR (1993) Tumor necrosis factor and its receptors in human ovarian cancer. Potential role in disease progression. J Clin Invest 91(5):2194–2206. https://doi.org/10.1172/JCI116446
Mori K, Hatamochi A, Ueki H, Olsen A, Jimenez SA (1996) The transcription of human alpha 1(I) procollagen gene (COL1A1) is suppressed by tumour necrosis factor-alpha through proximal short promoter elements: evidence for suppression mechanisms mediated by two nuclear-factor binding sites. Biochem J 319(Pt 3):811–816
Li AQ, Si JM, Shang Y, Gan LH, Guo L, Zhou TH (2010) Construction of COL1A1 short hairpin RNA vector and its effect on cell proliferation and migration of gastric cancer cells. Zhejiang Da Xue Xue Bao Yi Xue Ban 39(3):257–263
Zeller C, Dai W, Steele NL, Siddiq A, Walley AJ, Wilhelm-Benartzi CS, Rizzo S, van der Zee A, Plumb JA, Brown R (2012) Candidate DNA methylation drivers of acquired cisplatin resistance in ovarian cancer identified by methylome and expression profiling. Oncogene 31(42):4567–4576. https://doi.org/10.1038/onc.2011.611
Gifford G, Paul J, Vasey PA, Kaye SB, Brown R (2004) The acquisition of hMLH1 methylation in plasma DNA after chemotherapy predicts poor survival for ovarian cancer patients. Clin Cancer Res 10(13):4420–4426. https://doi.org/10.1158/1078-0432.CCR-03-0732
Roy R, Yang J, Moses MA (2009) Matrix metalloproteinases as novel biomarkers and potential therapeutic targets in human cancer. J Clin Oncol 27(31):5287–5297. https://doi.org/10.1200/JCO.2009.23.5556
Zhang Y, Chen Q (2017) Relationship between matrix metalloproteinases and the occurrence and development of ovarian cancer. Braz J Med Biol Res 50(6):e6104. https://doi.org/10.1590/1414-431X20176104
Tholen S, Biniossek ML, Gansz M, Ahrens TD, Schlimpert M, Kizhakkedathu JN, Reinheckel T, Schilling O (2014) Double deficiency of cathepsins B and L results in massive secretome alterations and suggests a degradative cathepsin-MMP axis. Cell Mol Life Sci 71(5):899–916. https://doi.org/10.1007/s00018-013-1406-1
Hijova E (2005) Matrix metalloproteinases: their biological functions and clinical implications. Bratisl Lek Listy 106(3):127–132
Poon SL, Klausen C, Hammond GL, Leung PC (2011) 37-kDa laminin receptor precursor mediates GnRH-II-induced MMP-2 expression and invasiveness in ovarian cancer cells. Mol Endocrinol 25(2):327–338. https://doi.org/10.1210/me.2010-0334
Laios A, Mohamed BM, Kelly L, Flavin R, Finn S, McEvoy L, Gallagher M, Martin C, Sheils O, Ring M, Davies A, Lawson M, Gleeson N, D’Arcy T, d’Adhemar C, Norris L, Langhe R, Saadeh FA, O’Leary JJ, O’Toole SA (2013) Pre-Treatment of platinum resistant ovarian cancer cells with an MMP-9/MMP-2 inhibitor prior to cisplatin enhances cytotoxicity as determined by high content screening. Int J Mol Sci 14(1):2085–2103. https://doi.org/10.3390/ijms14012085
Acknowledgements
This study was supported by Research Foundation of the University of Istanbul (Project no: 51472/2014).
Author information
Authors and Affiliations
Contributions
TG: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration supervision validation writing—original draft writing—review and editing. EG: formal analysis, methodology, software, validation, visualization, writing—original draft, writing—review and editing. BD: data curation, methodology, validation, visualization, writing—original draft, writing—review and editing. FBE: formal analysis, methodology, validation, writing—original draft, writing—review and editing. MKH: data curation, methodology, validation, formal analysis. NC: data curation, formal analysis, software. TS: data curation, resources. ST: data curation, project administration, resources, supervision. KA: data curation, resources.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
All patients and volunteers have been asked to sign and confirm the informed consent, whole sample collection and analysis processes are ethically approved by Istanbul University Faculty of Medicine Clinical Researches Ethics Committee (Permission no: 2014/1175) on 08/08/2014.
Rights and permissions
About this article
Cite this article
Günel, T., Gumusoglu, E., Dogan, B. et al. Potential biomarker of circulating hsa-miR-1273g-3p level for detection of recurrent epithelial ovarian cancer. Arch Gynecol Obstet 298, 1173–1180 (2018). https://doi.org/10.1007/s00404-018-4913-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4913-3