Abstract
Purpose
To evaluate how physicians in the United States (US) screen for, define, and treat a short cervix to prevent preterm birth.
Methods
This was a cross-sectional, web-based survey of 500 physicians treating pregnant patients with a short cervix in the US. Respondents’ geographic region was monitored to ensure balance across the nine US Census divisions.
Results
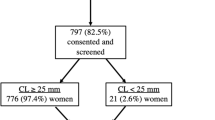
Respondents were predominantly obstetrician/gynecologists (86%, 429/500; mean age 49 years). Physicians reported that a median of 90% of their pregnant patients undergo cervical length screening; 81% (407/500) use transvaginal ultrasound. Physicians consult multiple evidence sources to inform their patient care, most commonly clinical guidelines (83%; 413/500) and published research (70%; 349/500). Most physicians (98%; 490/500) reported treating pregnant patients with a short cervix; 95% (474/500) use synthetic and/or natural progestogen, alone or in combination with other treatment modalities. If reimbursement was not a concern, 47% of physicians (230/500) would choose vaginal progesterone as their preferred treatment to prevent preterm birth in all patients with a short cervix, and 45% (218/500) would choose a synthetic progestogen.
Conclusion
US guidelines recommend transvaginal ultrasound for cervical length screening; 81% of physicians in this study reported using this method. Most physicians surveyed use progestogens to treat a short cervix, with approximately half choosing a synthetic progestin (45%) and half choosing natural progesterone (47%) as their preferred treatment, despite national guidelines recommending only vaginal natural progesterone for this indication. Additional physician education is required to implement current and best practices.


Similar content being viewed by others
References
To MS, Skentou CA, Royston P, Yu CK, Nicolaides KH (2006) Prediction of patient-specific risk of early preterm delivery using maternal history and sonographic measurement of cervical length: a population-based prospective study. Ultrasound Obstet Gynecol 27:362–367
Iams JD, Goldenberg RL, Meis PJ et al (1996) National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med 334:567–572
Berghella V, Tolosa JE, Kuhlman K, Weiner S, Bolognese RJ, Wapner RJ (1997) Cervical ultrasonography compared with manual examination as a predictor of preterm delivery. Am J Obstet Gynecol 177:723–730
Hassan SS, Romero R, Berry SM et al (2000) Patients with an ultrasonographic cervical length < or = 15 mm have nearly a 50% risk of early spontaneous preterm delivery. Am J Obstet Gynecol 182:1458–1467
World Health Organization (WHO) (2016) Born too soon: the global action report on preterm birth. http://www.who.int/pmnch/media/news/2012/preterm_birth_report/en/. Accessed 10 Jan 2017
March of Dimes (2015) 2015 premature birth report card: United States. http://www.marchofdimes.org/materials/premature-birth-report-card-united-states.pdf. Accessed 10 Oct 2016
Institute of Medicine, Committee on Understanding Premature Birth and Assuring Healthy Outcomes (2007) Societal costs of preterm birth. In: Behrman RE, Butler AS (eds) Preterm birth: causes, consequences, and prevention. National Academies Press (US), Washington (DC). https://www.ncbi.nlm.nih.gov/books/NBK11358/. Accessed 10 Jan 2017
Fonseca EB, Celik E, Parra M, Singh M, Nicolaides KH; Fetal Medicine Foundation Second Trimester Screening Group (2007) Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med 357:462–469
DeFranco EA, O’Brien JM, Adair CD et al (2007) Vaginal progesterone is associated with a decrease in risk for early preterm birth and improved neonatal outcome in women with a short cervix: a secondary analysis from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 30:697–705
Majhi P, Bagga R, Kalra J, Sharma M (2009) Intravaginal use of natural micronised progesterone to prevent pre-term birth: a randomised trial in India. J Obstet Gynaecol 29:493–498
Cetingoz E, Cam C, Sakallı M, Karateke A, Celik C, Sancak A (2011) Progesterone effects on preterm birth in high-risk pregnancies: a randomized placebo-controlled trial. Arch Gynecol Obstet 283:423–429
Norwitz ER, Caughey AB (2011) Progesterone supplementation and the prevention of preterm birth. Rev Obstet Gynecol 4:60–72
El-refaie W, Abdelhafez MS, Badawy A (2016) Vaginal progesterone for prevention of preterm labor in asymptomatic twin pregnancies with sonographic short cervix: a randomized clinical trial of efficacy and safety. Arch Gynecol Obstet 293:61–67
Guimarães Filho HA, Araujo Júnior E, Pires CR, Nardozza LM, Moron AF (2013) Short cervix syndrome: current knowledge from etiology to the control. Arch Gynecol Obstet 287:621–628
Hassan SS, Romero R, Vidyadhari D, PREGNANT Trial et al (2011) Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 38:18–31
Dodd JM, Jones L, Flenady V, Cincotta R, Crowther CA (2013) Prenatal administration of progesterone for preventing preterm birth in women considered to be at risk of preterm birth. Cochrane Database Syst Rev 7:CD004947
Conde-Agudelo A, Romero R, Nicolaides K et al (2013) Vaginal progesterone vs. cervical cerclage for the prevention of preterm birth in women with a sonographic short cervix, previous preterm birth, and singleton gestation: a systematic review and indirect comparison metaanalysis. Am J Obstet Gynecol 208:42.e1–18
Romero R, Nicolaides K, Conde-Agudelo A et al (2012) Vaginal progesterone in women with an asymptomatic sonographic short cervix in the midtrimester decreases preterm delivery and neonatal morbidity: a systematic review and metaanalysis of individual patient data. Am J Obstet Gynecol 206:124.e1–19
Romero R, Nicolaides KH, Conde-Agudelo A et al (2016) Vaginal progesterone decreases preterm birth ≤ 34 weeks of gestation in women with a singleton pregnancy and a short cervix: an updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol 48:308–317
O’Brien JM, Defranco EA, Adair CD, Progesterone Vaginal Gel Study Group et al (2009) Effect of progesterone on cervical shortening in women at risk for preterm birth: secondary analysis from a multinational, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol 34:653–659
Durnwald CP, Lynch CD, Walker H, Iams JD (2009) The effect of treatment with 17 alpha-hydroxyprogesterone caproate on changes in cervical length over time. Am J Obstet Gynecol 201(410):e1–e5
Romero R, Stanczyk FZ (2013) Progesterone is not the same as 17-hydroxyprogesterone caproate: implications for obstetrical practice. Am J Obstet Gynecol 208:421–426
Grobman WA, Thom EA, Spong CY et al (2012) 17 alpha-hydroxyprogesterone caproate to prevent prematurity in nulliparas with cervical length less than 30 mm. Am J Obstet Gynecol 207:390.e1–8
Medicaid Health Plans of America (MHPA) (2014) Preterm birth prevention: evidence-based use of progesterone treatment issue brief and action steps for Medicaid Health Plans. http://www.mhpa.org/_upload/PTBIssueBrief111714MHPA.pdf. Accessed 1 Jul 2016
International Federation of Gynecology and Obstetrics (FIGO) (2014) FIGO good practice advice. http://www.sego.es/Content/pdf/Best_practice_advise-July_2014.pdf. Accessed 10 Jan 2017
Society for Maternal-Fetal Medicine (SMFM) Publications Committee; Berghella V (2012) Progesterone and preterm birth prevention: translating clinical trials data into clinical practice. Am J Obstet Gynecol 206:376–386
American College of Obstetricians and Gynecologists (ACOG) (2012) ACOG practice bulletin no.130: prediction and prevention of preterm birth. Obstet Gynecol 120:964–973
Khandelwal M (2012) Vaginal progesterone in risk reduction of preterm birth in women with short cervix in the midtrimester of pregnancy. Int J Womens Health 4:481–490
National Institute for Health and Care Excellence (NICE) (2015) Preterm labour and birth. NICE guidelines: NG25. https://www.nice.org.uk/guidance/ng25. Accessed 1 Jul 2016
Harris Poll Online (2017) http://www.harrispollonline.com/. Accessed 28 Feb 2017
Sermo Polls (2017) http://www.sermo.com/polls. Accessed 28 Feb 2017
Devine S, Babrowicz J, Hahn R, Vorrasi J, Farid A, Yong J (2015) Intra-operative communication regarding neuromuscular blockade: a survey of anaesthesiologists and surgeons. J Anesth Clin Res 6:524–530
DiBenedetti DB, Nguyen D, Zografos L, Ziemiecki R, Zhou X (2011) A population-based study of Peyronie’s disease: prevalence and treatment patterns in the United States. Adv Urol 2011:282503
DiBenedetti DB, Nguyen D, Zografos L, Ziemiecki R, Zhou X (2011) Prevalence, incidence, and treatments of Dupuytren’s disease in the United States: results from a population-based study. Hand 6:149–158
DiBenedetti D, Baranowski E, Zelt S, Reynolds M, Sherrill B (2015) Assessing US patients’ and dermatologists’ experiences with severe chronic hand eczema. J Clin Aesthet Dermatol 8:19–27
DiBenedetti DB, Zhou X, Reynolds M, Ogale S, Best JH (2015) Assessing methotrexate compliance in rheumatoid arthritis: a cross-sectional survey. Rheumatol Ther 2:73–84
Deal LS, Sleeper-Triplett J, DiBenedetti DB et al (2015) Development and validation of the ADHD Benefits of Coaching Scale (ABCS). J Atten Disord 19:191–199
Williams RE, Kalilani L, DiBenedetti DB et al (2008) Frequency and severity of vasomotor symptoms among peri- and postmenopausal women in the United States. Climacteric 11:32–43
Williams RE, Kalilani L, DiBenedetti DB, Zhou X, Fehnel SE, Clark RV (2007) Healthcare seeking and treatment for menopausal symptoms in the United States. Maturitas 58:348–358
Levine KB, Williams RE, DiBenedetti DB, Fehnel SE, Clark RV (2006) Vulvo-vaginal atrophy and female sexual dysfunction among post-menopausal women: results from the MEPI study. Menopause 13:990
Poulos C, González JM, Lee LJ et al (2013) Physician preferences for extra-glycemic effects of type 2 diabetes treatments. Diabetes Ther 4:443–459
Poulos C, Johnson FR, Krishnarajah G, Anonychuk A, Misurski D (2015) Pediatricians’ preferences for infant meningococcal vaccination. Value Health 18:67–77
Williams VSL, Edin HM, Hogue SL et al (2010) Prevalence and impact of antidepressant-associated sexual dysfunction in three European countries: replication in a cross-sectional patient survey. J Psychopharmacol 24:489–496
Khalifeh A, Berghella V (2016) Universal cervical length screening in singleton gestations without a previous preterm birth: ten reasons why it should be implemented. Am J Obstet Gynecol 214:603.e1–5
Centers for Disease Control and Prevention (2015) Preterm birth. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm. Accessed 27 Jul 2016
Behrman RE, Butler AS (eds) (2007) Preterm birth: causes, consequences, and prevention. 12, societal costs of preterm birth. Institute of Medicine (US) Committee on Understanding Premature Birth and Assuring Healthy Outcomes. National Academies Press, Washington (DC). http://www.ncbi.nlm.nih.gov/books/NBK11358/. Accessed 29 Jul 2016
Acknowledgements
Medical writing services were provided by Kate Lothman of RTI Health Solutions; this support was funded by Juniper Pharmaceuticals.
Author information
Authors and Affiliations
Contributions
All authors participated in data analysis and/or interpretation and contributed to the development of the manuscript, and all authors consented to its submission and publication. Juniper Pharmaceuticals participated in the study design, research, data collection, analysis and interpretation, writing, review, and approval of this publication. The authors’ specific contributions are as follows: BM: Conceptualization, Funding acquisition (lead), Manuscript writing, Interpretation of study data. DBD: Conceptualization, Methodology, Formal analysis, Manuscript writing, Interpretation of study data. HW: Manuscript writing, Interpretation of study data. XZ: Methodology, Formal analysis (lead), Manuscript writing, Interpretation of study data. MR: Methodology, Formal analysis, Manuscript writing, Interpretation of study data. VB: Manuscript writing, Interpretation of study data. SSH: Manuscript writing, Interpretation of study data.
Corresponding author
Ethics declarations
Funding
This research and the preparation of this publication were funded by Juniper Pharmaceuticals.
Conflict of interest
B.M. and H.W. are employees of Juniper Pharmaceuticals. D.B.D., X.Z., and M.R. are employees of RTI Health Solutions. This research was performed under a contract between Juniper Pharmaceuticals and RTI Health Solutions. V.B. and S.H. report no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study procedures and materials were submitted to the institutional review board of RTI International, the responsible organization (submission ID 13956). The study was considered exempt from full review, per the Code of Federal Regulations, Part 46 (45CFR46.101[b]), of the US Health and Human Services’ Office for Human Research Protections.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Martell, B., DiBenedetti, D.B., Weiss, H. et al. Screening and treatment for short cervical length in pregnancy: a physician survey in the United States. Arch Gynecol Obstet 297, 601–611 (2018). https://doi.org/10.1007/s00404-017-4619-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4619-y