Abstract
Objective
To compare the efficacy and safety of intravaginal misoprostol versus dinoprostone cervical gel for cervical ripening and labour induction.
Methods
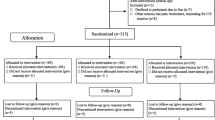
We carried out an experimental clinical trial in which we enrolled 130 cervical consecutive patients with cervical ripening, randomly assigned to one of the following two treatment groups: (1) intravaginal misoprostol and (2) intracervical dinoprostone gel. A total of 50 μm of misoprostol was placed in the posterior vaginal fornix every 6 h for a maximum period of 24 h and 0.5 mg of dinoprostone was administrated in the uterine cervix every 6 h, for a maximum period of 24 h. The primary outcome measure was the number (rate) of women who went to vaginally deliver within 24 h of the protocol initiation.
Results
Among 130 patients evaluated, 65 were allocated to the misoprostol group and 65 to the dinoprostone group. The proportion of vaginal delivery within 24 h was significantly higher in the misoprostol group (75%) than in the dinoprostone group (53.8%) (RR = 1.40, 95% CI [1.07–1.45], P = 0.02). There was no significant difference between the mean time interval of delivery in the misoprostol group and the dinoprostone group (14.9 vs.15.8 h) (P = 0.51). The Bishop score was significantly higher in the misoprostol group, 6 h after the onset of the study (1.38; relative risk, 95% CI [1.02–1.85], P = 0.03). The Caesarean delivery rate for fetal distress was higher in the dinoprostone group (21 vs. 10.8%, P = 0.15). The tachysystole (Misoprostol 6.1% vs. dinoprostone 4.6%, relative risk 1.15, 95% CI [0.6–2.24]) and hyperstimulation syndrome rates (Misoprostol 7.6% vs. dinoprostone 4.6%, relative risk 1.26, 95% CI [0.72–2.24]) were slightly increased in the misoprostol group than in the dinoprostone group without reaching the level of statistical signification.
Conclusion
Misoprostol as used in this protocol is more effective than cervical dinoprostone gel application in the cervical ripening and labour induction. There is a tendency for an increase in the rate of tachysystole and hyperstimulation syndrome.

Similar content being viewed by others
References
Hofmeyr GJ (2003) Induction of labor with unfavourable cervix. Best Pract Res Clin Obstet Gynecol 17:777–794
Chung JH, Huang WH, Rumney PJ (2003) A prospective randomized controlled trial that compared misoprostol, Foley catheter, and combination misoprostol-Foley catheter for labor induction. Am J Obstet Gynecol 189:1031–1035
Hofmeyr GJ, Gulmezoglu AM (2003) Vaginal misoprostol for cervical ripening and induction of labour. The Cochrane Database Syst Rev.CD000941. doi 10.1002/14651858. CD000941
American College of Obstetricians, Gynecologists (2003) New US Food and drug administration labelling on cytotec (Misoprostol) use and Pregnancy, Committee Opinion Number 283. Obstet Gynecol 101:1049–1050
Ghidini A, Spong CY, Korker V, Mariani E (2001) Randomized controlled trial of 50 and 100 mcg of misoprostol for induction of labor at term. Arch Gynecol Obstet 265:128–130
Sanchez-Ramos L, Kaunitz AM, Delke I (2002) Labor induction with 25 μg versus 50 μg intravaginal misoprostol: a systematic review. Obstet Gynecol 99:145–151
Ozosy M, Ozosy D (2004) Induction of labor with 50 and 100 μg of misoprostol: comparison of maternal and foetal outcomes. Eur J Obst Gyn Rep Biol 113:41–44
Wing DA, Ortiz-Omphroy G, Paul RH (1997) A comparison of intermittent vaginal administration of misoprostol with continuous dinoprostone for cervical ripening and labor induction. Am J Obstet Gynecol 177:612–618
Le Roux PA, Olarogun JO, Penny J, Anthony J (2002) Oral and vaginal misoprostol compared with dinoprostone for induction of labor: a randomized controlled trial. Obstet Gynecol 99:201–205
Blanchette H, Nayak S, Erasmus S (1999) Comparison of the safety and efficacy of intravaginal misoprostol (prostaglandin E1) with those of dinoprostone (prostaglandin E2) for cervical ripening and induction of labor in a community hospital. Am J Obstet Gynecol 180:1551–1559
Papanikolaou EG, Plachouras N, Drougia A, Andronikou S, Vlachou C, Stefos T, Paraskevaidis E, Zikopoulos K (2004) Comparison of misoprostol and dinoprostone for elective induction of labour in nulliparous women at full term: a prospective study. Reprod Biol Endocrinol 2:70–77
Agarwal N, Gupta A, Kriplani A, Bhatla N, Parul (2003) Six hourly vaginal misoprostol versus intracervical dinoprostone for cervical ripening and labor induction. J Obstet Gynaecol Res 29:147–151
Lyons C, Beharry K, Akmal Y, Attenello F, Nageotte MP (2003) In vitro response of prostaglandin E2 receptor (EP3) in the term pregnant rat uterus and cervix to misoprostol. Prostaglandins Other Lipid Mediat 70:317–321
Rozenberg P, Chevret S, Goffinet F, Dyrand-Zaleski I, Ville Y, Vayssière C (2001) Induction of labour with a viable infant: a randomised clinical trial comparing intravaginal misoprostol and intravaginal dinoprostone. BJOG 108:1255–1262
Ramsey PS, Ogburn PL, Harris DY, Heise RH, Ramin KD (2000) Effect of vaginal pH on efficacy of misoprostol for cervical ripening and labor induction. Am J Obstet Gynecol 182:1616–1619
Tang OS, Ho PC (2002) Pharmacokinetics of different routes of administration of misoprostol. Hum Reprod 17:332–336
Wolf SB, Sanchez-Ramos L, Kaunitz AM (2005) Sublingual misoprostol for labor induction: a randomized clinical trial. Obstet Gynecol 2:365–371
Bennett BB (1997) Uterine rupture during induction of labor at term with intravaginal misoprostol. Obstet Gynecol 89:832–833
Response to Searle’s drug warning on Misoprostol (2000) ACOG committee opinion no 248. ACOG, Washington
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Denguezli, W., Trimech, A., Haddad, A. et al. Efficacy and safety of six hourly vaginal misoprostol versus intracervical dinoprostone: a randomized controlled trial. Arch Gynecol Obstet 276, 119–124 (2007). https://doi.org/10.1007/s00404-006-0313-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-006-0313-1