Abstract
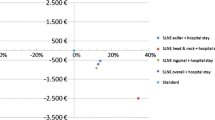
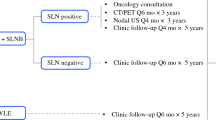
The objective is to determine the cost-effectiveness of sentinel lymph node biopsy (SLNB) for cutaneous squamous cell carcinoma (CSCC) according to the Brigham and Women’s Hospital (BWH) Tumor Staging system. A decision analysis was utilized to examine costs and outcomes associated with the use of SLNB in patients with high-risk head and neck CSCC. Decision tree outcome probabilities were obtained from published literature. Costs were derived from Medicare reimbursement rates (US$) and effectiveness was represented by quality-adjusted life-years (QALYs). The primary outcome was the incremental cost-effectiveness ratio (ICER), with a willingness-to-pay set at $100,000 per QALY gained. SLNB was found to be a cost-effective tool for patients with T3 tumors, with an ICER of $18,110.57. Withholding SLNB was the dominant strategy for both T2a and T2b lesions, with ICERs of − $2468.99 and − $16,694.00, respectively. Withholding SLNB remained the dominant strategy when examining immunosuppressed patients with T2a or T2b lesions. In patients with head and neck CSCC, those with T3 or T2b lesions with additional risk factors not accounted for in the staging system alone, may be considered for SLNB, while in other tumor stages it may be impractical. SLNB should only be offered on an individual patient basis.

Similar content being viewed by others
References
Que SKT, Zwald FO, Schmults CD (2018) Cutaneous squamous cell carcinoma: Incidence, risk factors, diagnosis, and staging. J Am Acad Dermatol 78:237–247
Karia PS, Han J, Schmults CD (2013) Cutaneous squamous cell carcinoma: Estimated incidence of disease, nodal metastasis, and deaths from disease in the United States, 2012. J Am Acad Dermatol 68:957–966. https://doi.org/10.1016/j.jaad.2012.11.037
Thompson AK, Kelley BF, Prokop LJ et al (2016) Risk factors for cutaneous squamous cell carcinoma recurrence, metastasis, and disease-specific death: a systematic review and meta-analysis. JAMA Dermatol 152:419–428. https://doi.org/10.1001/jamadermatol.2015.4994
Blechman AB, Carucci JA, Stevenson ML (2019) Stratification of poor outcomes for cutaneous squamous cell carcinoma in immunosuppressed patients using the American joint committee on cancer eighth edition and Brigham and women’s hospital staging systems. Dermatol Surg 45:1117–1124. https://doi.org/10.1097/DSS.0000000000001774
Howard MD, Su JC, Chong AH (2018) Skin cancer following solid organ transplantation: a review of risk factors and models of care. Am J Clin Dermatol 19:585–597
Mooney CP, Martin RCW, Dirven R et al (2019) Sentinel node biopsy in 105 high-risk cutaneous sccs of the head and neck: results of a multicenter prospective study. Ann Surg Oncol 26:4481–4488. https://doi.org/10.1245/s10434-019-07865-z
Gore SM, Shaw D, Martin RCW et al (2016) Prospective study of sentinel node biopsy for high-risk cutaneous squamous cell carcinoma of the head and neck. Head Neck 38(Suppl 1):E884–E889. https://doi.org/10.1002/hed.24120
Tejera-Vaquerizo A, García-Doval I, Llombart B et al (2018) Systematic review of the prevalence of nodal metastases and the prognostic utility of sentinel lymph node biopsy in cutaneous squamous cell carcinoma. J Dermatol 45:781–790
Quinn PL, Oliver JB, Mahmoud OM, Chokshi RJ (2019) Cost-effectiveness of sentinel lymph node biopsy for head and neck cutaneous squamous cell carcinoma. J Surg Res 241:15–23. https://doi.org/10.1016/j.jss.2019.03.040
Jambusaria-Pahlajani A, Kanetsky PA, Karia PS et al (2013) Evaluation of AJCC tumor staging for cutaneous squamous cell carcinoma and a proposed alternative tumor staging system. JAMA Dermatol 149:402–410. https://doi.org/10.1001/jamadermatol.2013.2456
Karia PS, Jambusaria-Pahlajani A, Harrington DP et al (2014) Evaluation of American joint committee on cancer, international union against cancer, and Brigham and women’s hospital tumor staging for cutaneous squamous cell carcinoma. J Clin Oncol 32:327–334. https://doi.org/10.1200/JCO.2012.48.5326
Ruiz ES, Karia PS, Besaw R, Schmults CD (2019) Performance of the American joint committee on cancer staging manual, 8th edition vs the Brigham and women’s hospital tumor classification system for cutaneous squamous cell carcinoma. JAMA Dermatol 155:819–825. https://doi.org/10.1001/jamadermatol.2019.0032
Sahovaler A, Krishnan RJ, Yeh DH et al (2019) Outcomes of cutaneous squamous cell carcinoma in the head and neck region with regional lymph node metastasis: a systematic review and meta-analysis. JAMA Otolaryngol-Head Neck Surg 145:352–360. https://doi.org/10.1001/jamaoto.2018.4515
Brunner M, Ng BC, Veness MJ, Clark JR (2015) Assessment of the new nodal classification for cutaneous squamous cell carcinoma and its effect on patient stratification. Head Neck 37:336–339. https://doi.org/10.1002/hed.23602
Schmults CD, Blitzblau R, Aasi SZ et al (2021) National comprehensive cancer network clinical practice guidelines—squamous cell skin cancer—version 1.2021. https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1437
Hollman C, Paulden M, Pechlivanoglou P, McCabe C (2017) A comparison of four software programs for implementing decision analytic cost-effectiveness models. Pharmacoeconomics 35:817–830. https://doi.org/10.1007/S40273-017-0510-8
Prasath V, Quinn PL, Oliver JB et al (2021) Cost-effectiveness analysis of infected necrotizing pancreatitis management in an academic setting. Pancreatology. https://doi.org/10.1016/J.PAN.2021.11.011
Wu MP, Sethi RKV, Emerick KS (2020) Sentinel lymph node biopsy for high-risk cutaneous squamous cell carcinoma of the head and neck. Laryngoscope 130:108–114. https://doi.org/10.1002/lary.27881
Amoils M, Lee CS, Sunwoo J et al (2017) Node-positive cutaneous squamous cell carcinoma of the head and neck: survival, high-risk features, and adjuvant chemoradiotherapy outcomes. Head Neck 39:881–885. https://doi.org/10.1002/hed.24692
Hirshoren N, Danne J, Dixon BJ et al (2017) Prognostic markers in metastatic cutaneous squamous cell carcinoma of the head and neck. Head Neck 39:772–778. https://doi.org/10.1002/hed.24683
Jansen P, Petri M, Merz SF et al (2019) The prognostic value of sentinel lymph nodes on distant metastasis–free survival in patients with high-risk squamous cell carcinoma. Eur J Cancer 111:107–115. https://doi.org/10.1016/j.ejca.2019.02.004
Morton DL, Thompson JF, Cochran AJ et al (2014) Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med 370:599–609. https://doi.org/10.1056/nejmoa1310460
Beck JR, Pauker SG, Gottlieb JE et al (1982) A convenient approximation of life expectancy (the “DEALE”). II. Use in medical decision-making. Am J Med 73:889–897. https://doi.org/10.1016/0002-9343(82)90787-2
Morton RL, Tran A, Vessey JY et al (2017) Quality of life following sentinel node biopsy for primary cutaneous melanoma: health economic implications. Ann Surg Oncol 24:2071–2079. https://doi.org/10.1245/s10434-017-5842-2
Neumann PJ, Cohen JT, Weinstein MC (2014) Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med 371:796–797. https://doi.org/10.1056/NEJMp1405158
Ubel PA, Hirth RA, Chernew ME, Fendrick AM (2003) What is the price of life and why doesn’t it increase at the rate of inflation? Arch Intern Med 163:1637–1641
Serra-Arbeloa P, Rabines-Juárez ÁO, Álvarez-Ruiz MS, Guillén-Grima F (2016) Sentinel node biopsy in patients with primary cutaneous melanoma of any thickness: a cost-effectiveness analysis. Surg Oncol 25:205–211. https://doi.org/10.1016/j.suronc.2016.05.020
Agnese DM, Abdessalam SF, Burak WE et al (2003) Cost-effectiveness of sentinel lymph node biopsy in thin melanomas. Surgery 134:542–547. https://doi.org/10.1016/S0039-6060(03)00275-7
Morton RL, Howard K, Thompson JF (2009) The cost-effectiveness of sentinel node biopsy in patients with intermediate thickness primary cutaneous melanoma. Ann Surg Oncol 16:929–940. https://doi.org/10.1245/s10434-008-0164-z
Faries MB, Thompson JF, Cochran AJ et al (2017) Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med 376:2211–2222. https://doi.org/10.1056/nejmoa1613210
Pampena R, Raucci M, Mirra M et al (2019) The role of ultrasound examination for early identification of lymph-node metastasis of cutaneous squamous cell carcinoma: results from a single institutional center. G Ital Dermatol Venereol. https://doi.org/10.23736/S0392-0488.19.06487-3
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design, acquisition of data, analysis, interpretation of data, and final approval of the manuscript. PLQ, JKK, VP, TJK and RJC contributed to the drafting of the article. The critical revision of the article was performed by all of the authors.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Patrick L. Quinn, Dr. Jin K. Kim, Mr. Vishnu Prasath, Mr. Neal Panse, Dr. Thomas J. Knackstedt, and Dr. Ravi J. Chokshi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Quinn, P.L., Kim, J.K., Prasath, V. et al. Sentinel lymph node biopsy for head and neck cutaneous squamous cell carcinoma using the Brigham and Women’s staging system: a cost analysis. Arch Dermatol Res 315, 371–378 (2023). https://doi.org/10.1007/s00403-022-02347-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-022-02347-x