Abstract
Introduction
Anterior cruciate ligament (ACL) reconstruction remains associated with the risk of re-rupture and persisting rotational instability. Additional extraarticular anterolateral stabilization procedures stabilize the tibial internal rotation and lead to lower ACL failure rate and improved knee stability. However, data for additional stabilization of tibial external rotation is lacking and the importance of an anteromedial stabilization procedure is less well evaluated. Aim of this study is to investigate the influence of an extraarticular anteromedial stabilization procedure for the stabilization of the tibial external rotation and protection of the ACL from these rotational forces.
Methods
Internal and external rotations of the tibia were applied to a finite element (FE) model with anatomical ACL, posterior cruciate ligament (PCL), lateral collateral ligament (LCL), medial collateral ligament (MCL) and intact medial and lateral meniscus. Five additional anatomic structures (Anteromedial stabilization/anteromedial ligament, AML, augmented superficial medial collateral ligament, sMCL, posterior oblique ligament, POL, anterolateral ligament, ALL, and popliteal tendon, PLT) were added to the FE model separately and then combined. The force histories within all structures were measured and determined for each case.
Results
The anteromedial stabilization or imaginary AML was the main secondary stabilizer of tibial external rotation (90% of overall ACL force reduction). The AML reduced the load on the ACL by 9% in tibial external rotation which could not be achieved by an augmented sMCL (-1%). The AML had no influence in tibial internal rotation (-1%). In the combined measurements with all additional structures (AML, ALL, PLT, POL) the load on the ACL was reduced by 10% in tibial external rotation.
Conclusion
This study showed that an additional anteromedial stabilization procedure secures the tibial external rotation and has the most protective effect on the ACL during these external rotational forces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction still has a risk of re-rupture and persisting rotational instability and outcomes after ACL revision surgery are worse [1,2,3,4]. It is proven that an additional extraarticular anterolateral stabilization procedure or reconstruction of the anterolateral ligament (ALL) can lead to lower ACL reconstruction failure rate and improved knee stability [5,6,7,8,9,10]. Due to its oblique course the ALL stabilizes besides anterior translation the internal rotation of the tibia and therefore secures the ACL graft when high forces acting on the knee joint. However, the ALL is not able to stabilize the external rotation of the tibia which often is part of the ACL injury mechanism, especially in combination with valgus stressing, a fact that is often overlooked [11,12,13,14]. Therefore, to stabilize the tibial external rotation anteromedial structures should be brought into focus [15]. The fact of high rates of concomitant MCL ruptures during ACL injuries confirms this assumption [16, 17]. Therefore, medial structures should be addressed to restore anteromedial knee stability after an ACL injury and to protect the ACL graft after reconstruction [18,19,20,21,22,23]. To stabilize the knee and the ACL graft in external tibial rotation, a medial structure should be obviously constituted like a mirrored ALL from the lateral side. It should extend obliquely from the medial femoral epicondyle to the anterior medial part of the proximal tibia. This is already backed up by increasing interest in the medial side in ACL injuries and the importance of the complex architecture of the whole MCL with influence of the different fibers like the more anterior superficial MCL (sMCL) and the posterior oblique ligament (POL) [15,16,17, 23,24,25].
Thus, the primary objective of the present study was to assess the efficacy of different parts of the MCL, including an extraarticular anteromedial stabilization procedure, in enhancing knee stability, particularly in tibial external rotation. We evaluated this in a finite element knee model study to assess the impact on the rotational stability of the knee joint and on the ACL itself. Accordingly to the ALL on the lateral side the corresponding structure targeted for reconstruction on the medial side in the anteromedial stabilization procedure was termed the anteromedial ligament. We hypothesized that an extraarticular anteromedial stabilization procedure could serve as the primary stabilizer against tibial external rotation and offer superior protection to the ACL against these rotational forces compared to other medial or lateral extraarticular structures.
Materials
Human knee model
The Global Human Body Model Consortium (GHBMC) full human body model represents a 50th percentile male in an upright standing posture. The model has been developed by GHBMC [26] and is commonly used for traffic accident simulations involving human beings as occupants and pedestrians in combination with the explicit finite element solver LS-DYNA (Livermore Software Technology Corporation, LSTC) [27]. The knee angle has been adjusted to 25° in order to acquire a more critical reference configuration for ACL ruptures. In this configuration, the reference lengths of the ligaments were stated in a recent publication [15]. All material properties and contact definitions in the model components were kept constant and have not been modified.
The same material model with distinct properties for tension and compression (*MAT_PLASTICITY_COMPRESSION_TENSION) already used for the existing knee ligaments has been assigned to the additional extra-articular structures. The material model used for the ligaments follows an approach by Untaroiu et al. [28]. Since ligaments are much stiffer in tension than in compression, an isotropic elastic-plastic material model with different properties in compression and tension is used. Material parameters were described in an earlier publication [15]. Since identical material parameters are applied to all ligaments (including AML), the numerical simulation can quickly reveal a relative load distribution. The predominantly loaded ligaments can be identified easily using this approach, as long as the applied moment is not excessively high and the stress level in the ligaments is not near failure. The average tensile stress-strain curve reported by Quapp et al. [29] and a less stiffer curve were assigned to the material model in tension and compression, respectively [30]. The isolated FE model (knee joint) has been cut approximatively 170 mm above and 140 mm below the tibia plateau. The exact cutting edges are along the given spatial discretization. The model consists of roughly 50,000 elements and 37.000 nodes. All physical components (bones, muscles, ligaments, soft tissue) are organized by a total of 32 components. The isolated knee model encompasses a volume of 3.7 L and has a mass of 4.2 kg. The nodes on both cutting surfaces, on the femoral side and on the tibia side, are kinematically constrained so that no relative movement of the nodes is possible. While the rigid section of the tibia is fixed, the rigid section of the femur is loaded instantaneously by a constant moment of 20 Nm in order to establish both scenarios, femoral external and femoral internal rotation. The duration of the simulation was 100 ms. Since the final nodal positions are almost constant after approximately 60 ms, the final rotation angle and the normal forces within the internal ligaments and the extra-articular structures were averaged from this point of time to the end of the simulation.
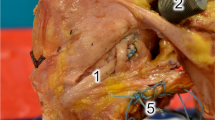
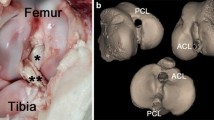
Measurement
The left knee of the GHBMC M50 full human body finite element model with anatomical ACL, posterior cruciate ligament (PCL), lateral collateral ligament (LCL), medial collateral ligament (MCL) and an intact medial and lateral meniscus was isolated (Fig. 1). Five additional anatomic structures (Anteromedial stabilization/anteromedial ligament, AML, augmented superficial medial collateral ligament, sMCL, posterior oblique ligament, POL, anterolateral ligament, ALL, and popliteal tendon, PLT), were added to the human knee model separately and then all together. The additional extraarticular anteromedial stabilization was applied on the medial side and it was set more oblique compared to the anterior part of the sMCL with a course similar to the ALL on the lateral side and was called “imaginary” anteromedial ligament (AML). The femoral footprint was 4 mm posterior and 8 mm proximal to the medial epicondyle and the tibial footprint at a point of the tibial footprint of the ALL (between the Gerdy tubercle and the fibular head, 10 mm below the medial joint line) but mirrored from the midpoint of the tibia plateau to the medial tibial side (Fig. 2). The length of the AML was measured in flexion and extension and showed no differences. Thus, the femoral and tibial AML fixation was performed isometrically. The length of the AML prior to the rotation was 56.8 mm. For the sake of simplicity, any pre-stresses in the ligaments were neglected. The reference configuration of the model was assumed to be completely stress-free and undeformed.
An external-internal torque was applied to the femur (tibial external rotation) section which is defined rigid with and without the three additional anatomic structures by an external load.
The torque was applied about the longitudinal axis of the femur. The longitudinal femoral axis was defined by the center points of the femur at the femur section and the center point on the tibial plateau. The translational movement of the femur section along the transversal direction was restricted. The translational movement along the longitudinal axis was left free, also the remaining rotational degrees of freedom. The tibia section was defined rigid and completely fixed in space, all translational and rotational degrees of freedom were restricted. All other parts of the model were deformable.
The intensity of the applied torque has been selected by trial and error in order to establish a loading scenario where the ligaments are subjected to an intermediate stress level. The intensity should be strong enough to reveal the relative load distribution in all ligaments of interest, but still far below the failure limit to avoid unphysiological results. The maximum forces carried by the ligaments were in the range of 200–400 N and seem to be realistic. Due to Kennedy et al. [28], the tensile strength of a medial collateral ligament is in the range of 467 ± 33 N.
The normal force histories within the ACL, PCL, LCL and MCL and in each extra-articular structure were measured and the final rotational displacements of the rotated body part were determined for each case. Along the half-length of all ligaments in the model, cross-sections have been defined for tracing the forces carried by the ligaments along their longitudinal directions. The location and the orientation of the cross-sections were updated each cycle according to the current nodal positions.
Data collection and descriptive statistical analysis was performed with Statistical Package for the Social Science (SPSS) after measurements.
Results
Our finite element model showed that the additional anteromedial stabilization procedure or imaginary AML reconstruction was the main secondary stabilizer of tibial external rotation (90% of overall ACL force reduction) and the ALL was the main secondary stabilizer of the tibial internal rotation (50% of overall ACL force absorption). The AML reduced the load on the ACL by 9% in tibial external rotation which could not be achieved by an augmented sMCL (-1%). The AML had no influence in tibial internal rotation (-1%) (Table 1; Fig. 3). In contrast, the ALL reduced the load on the ACL in tibial internal rotation by 21% but had no influence in tibial external rotation (-2%). There was no load reduction on other ligaments (PCL, LCL, MCL) by the ALL and AML (Fig. 3). In the combined measurements with all additional structures (AML, ALL, PLT, POL) the load on the ACL was reduced by 41% in tibial internal rotation. In tibial external rotation the load on the ACL was reduced by 10% with all additional structures (Table 1). An augmented sMCL had only a marginal effect as an additional stabilizer on the ACL in external or internal tibial rotation (Table 1).
Discussion
This study showed that an additional anteromedial stabilization procedure secures tibial external rotation and has the most protective effect on the ACL during these external rotational forces.
The ALL developed from a newly recognized and small anatomical structure to an important ligament in ACL surgery, especially during revisions [10, 31,32,33]. Meanwhile many surgeons add an extraarticular anterolateral stabilization procedure in primary or secondary ACL reconstruction to increase graft survival and improve knee stability [7, 10, 34,35,36]. However, the ALL stabilizes besides anterior tibial translation only internal rotation of the tibia and has no stabilizing function in other mechanism of ACL injury such as valgus stressing or tibial external rotation [15, 37, 38]. Admittedly it is already proven that valgus stressing, and external rotation of the tibia are main mechanisms in ACL injuries, but currently there are no guidelines which considers these facts in treatment regimens for ACL injuries [11, 15, 21, 39, 40]. A distinct structure apart from the ACL which sufficiently stabilizes the tibial external rotation is not evident. At least it is accepted that the medial side of the knee joint plays an important role in ACL injuries or valgus stabilization respectively and its impact is just under intense scientific evaluation [18, 19, 23, 41]. The fact that most of the ACL injuries contain valgus stressing as an injury mechanism, which is mainly stabilized by the MCL, put this structure more and more into the focus [11, 39, 40, 42]. However, surgical treatment algorithms of concomitant MCL lesions in ACL injuries are still lacking [18, 41]. Considering this lack of clarity, the authors of the present study hypothesized that a structure at the medial side of the knee joint very similar to the ALL on the lateral side might play a crucial role in the treatment of combined ACL/MCL injuries. The reason of this hypothesis was that such a structure with such a course could not only stabilize valgus gaping and anterior translation but also tibial external rotation. In the present finite element (FE) knee model study an extraarticular anteromedial stabilization procedure with such a structure with a course similar to the ALL on the lateral side was the most important stabilizer in tibial external rotation of the knee joint. Moreover, it reduced forces on the ACL in tibial external rotation most effectively. Therefore, this additional surgical stabilization of the medial side could be rational in several ACL injuries, especially in injuries which involved valgus stressing or tibial external rotation and with involvement of the MCL and radiological changes as severe lateral bone marrow edema with impression or fluid around the anteromedial capsule and/or the sMCL. The surgical technique of a gracilis tenodesis of Wierer et al. to reconstruct an anteromedial instability and the affected superficial MCL by proximal harvesting of the gracilis tendon and fixation at the medial femoral epicondyle could maybe already considered as an extraarticular anteromedial stabilization procedure or the Lemaire reconstruction of the medial knee compartment [25]. It was postulated that this procedure could both restore the MCL stability to bear valgus stressing in slight flexion sufficiently and protect the ACL graft against further stressing. Moreover, recent studies showed that a sMCL graft in combination with an oblique anteromedial stabilization procedure can restore native knee external rotation laxity and achieve better medial knee stability [43, 44]. The present FE knee model study confirmed these assumptions and even showed quantitatively that a procedure like this stabilizes the external tibial rotation and the ACL most effectively. It should be emphasized that this stabilizing effect could not be achieved by an augmentation of the sMCL with or without a reconstruction of the POL. This is also consistent with the existing data about anteromedial stabilization procedures [43, 44]. Finally, it must be mentioned that the AML was responsible for 90% of the overall force reduction on the ACL in tibial external rotation. The ALL for only 50% in tibial internal rotation. This showed the importance of the anteromedial knee structures and the limited compensation mechanisms when these structured are affected. Therefore, the results of present study underlined that combined injuries of the ACL and the MCL should be treated with special care and an additional anteromedial stabilization procedure might be very beneficial in several cases. Even low-grade lesions of the MCL or moderate instabilities after conservative treatment (grad I and II) might be a reasonable indication for surgical stabilization. Whether a common femoral footprint is sufficient and effective for a combined sMCL/AML reconstruction is still a matter of debate. However, future studies are needed to verify these first results of an extraarticular anteromedial stabilization procedure.
The present study has some limitations: First, the human knee model is merely an image of the natural knee and may contain geometric, biomechanical, and material deficiencies so that only biomechanical tendencies may be displayed. Moreover, in present the study the same material model was used for all tested ligaments. This may could have accentuated the results in a quantitative manner. Second, the human knee model includes an intact capsule and an intact medial and lateral meniscus. Therefore, a possible influence of these structures to the load of the ACL or the knee stability in external and internal rotation is not considered. Third, the mechanism of an ACL rupture is mostly a combination of rotational forces and valgus/varus stressing as well as tibial translation. In the present study only the internal and external rotation were considered in 25° flexion. Therefore, structures like the MCL or LCL and the influence of structures in other flexion angles might be underestimated in its function as a protector of the ACL.
Conclusion
This study showed that an additional anteromedial stabilization procedure secures tibial external rotation and has the most protective effect on the ACL during these external rotational forces.
References
Kaplan DJ, Jazrawi LM (2018) Secondary stabilizers of tibial rotation in the Intact and Anterior Cruciate. Clin Sports Med 37(1):49–59
Noyes FR, Huser LE, Levy MS (2017) Rotational knee instability in ACL-Deficient knees: role of the Anterolateral. J Bone Jt Surg Am 99(4):305–314
Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA (2016) u. a. incidence of anterior cruciate ligament tears and Reconstruction: a 21-Year. Am J Sports Med 44(6):1502–1507
Tischer T, Condello V, Menetrey J, Dejour D, Beaufils P, Becker R (2022) Time to focus on ACL revision: ESSKA 2022 consensus. Knee Surg Sports Traumatol Arthrosc. 19
Ra HJ, Kim JH, Lee DH (2020) Comparative clinical outcomes of anterolateral ligament reconstruction versus lateral extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: systematic review and meta-analysis. Arch Orthop Trauma Surg.; (140): 923–931
Helito CP, Camargo DB, Sobrado MF, Bonadio MB, Giglio PN, Pacora C (2018) JR, u. a. combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 26(12):3652–3659
Lee DW, Kim JG, Cho SI, Kim DH (2019) Clinical outcomes of isolated revision Anterior Cruciate Ligament Reconstruction or in Combination with Anatomic Anterolateral Ligament Reconstruction. Am J Sports Med 47(2):324–333
Sonnery-Cottet B, Barbosa NC, Vieira TD, Saithna A (2018) Clinical outcomes of extra-articular tenodesis/anterolateral reconstruction in. Knee Surg Sports Traumatol Arthrosc 26(2):596–604
Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L (2016) u. a. The involvement of the Anterolateral Ligament in Rotational Control of the knee. Am J Sports Med 44(5):1209–1214
Yoon KH, Hwang IU, Kim EJ, Kwon YB, Kim SAO (2020) Anterolateral Ligament Reconstruction Improves Anteroposterior Stability as Well as Rotational Stability in Revision Anterior Cruciate Ligament Reconstruction with High-Grade Pivot Shift. J Knee Surg 34(12):1310–1317
Shimokochi Y, Shultz SJ (2008) Mechanisms of noncontact anterior cruciate ligament injury. J Athl Train 43(4):396–408
Mechanisms for noncontact (2010) Anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med 38(11):2218–2225
Mehl J, Diermeier T, Herbst E, Imhoff AB, Stoffels T, Zantop T (2018) u. a. evidence-based concepts for prevention of knee and ACL injuries. 2017 guidelines. Arch Orthop Trauma Surg 138(1):51–61
Olsen OE, Myklebust G, Engebretsen L, Bahr R (2004) Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med 32(4):1002–1012
Blanke F, Boljen M, Lutter C, Oehler N, Tischer T, Vogt S (2021) Does the anterolateral ligament protect the anterior cruciate ligament in the most common injury mechanisms? A human knee model study. Knee 1 März 29:381–389
Lind M, Jacobsen K, Nielsen T (2020) Medial collateral ligament (MCL) reconstruction results in improved medial stability: results from the Danish knee ligament reconstruction registry (DKRR). Knee Surg Sports Traumatol Arthrosc off J ESSKA März 28(3):881–887
Svantesson E, Hamrin Senorski E, Alentorn-Geli E, Westin O, Sundemo D, Grassi A (2019) u. a. increased risk of ACL revision with non-surgical treatment of a concomitant. Knee Surg Sports Traumatol Arthrosc 27(8):2450–2459
Blanke F, Paul J, Haenle M, Sailer J, Pagenstert G, Wehren LV (2017) u. a. results of a New Treatment Concept for concomitant lesion of medial collateral. J Knee Surg 30(7):652–658
Grant JA, Tannenbaum E, Miller BS, Bedi A (2012) Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthrosc J Arthrosc Relat Surg off Publ Arthrosc Assoc N Am Int Arthrosc Assoc Januar 28(1):110–122
Mazzocca AD, Nissen CW, Geary M, Adams DJ (2003) Valgus medial collateral ligament rupture causes concomitant loading and damage of the anterior cruciate ligament. J Knee Surg Juli 16(3):148–151
Mehl J, Diermeier T, Herbst E, Imhoff AB, Stoffels T, Zantop T (2018) u. a. evidence-based concepts for prevention of knee and ACL injuries. 2017 guidelines of the ligament committee of the German Knee Society (DKG). Arch Orthop Trauma Surg Januar 138(1):51–61
Meyer P, Reiter A, Akoto R et al (2022) Imaging of the medial collateral ligament of the knee: a systematic review. Arch Orthop Trauma Surg 142:3721–3736
Reider B (1996) Medial collateral ligament injuries in athletes. Sports Med 21(2):147–156
Tischer T, Condello V, Menetrey J, Dejour D, Beaufils P, Becker R (2023) Time to focus on ACL revision: ESSKA 2022 consensus. Knee Surg Sports Traumatol Arthrosc off J ESSKA November 31(11):4637–4638
Wierer G, Kittl C, Fink C, Weiler A (2022) Medial collateral Ligament Reconstruction: a gracilis tenodesis for anteromedial knee instability. Arthrosc Tech August 11(8):e1409–e1418
Elemance K, Clemmons NC (2018)
Hallquist JO (2018) LS-DYNA Keyword user’s Manual. Livermore Software and Technology Corporation
Kennedy JC, Hawkins RJ, Willis RB, Danylchuk KD (1976) Tension studies of human knee ligaments. J Bone Jt Surg 58(3):350–355
Quapp KM, Weiss JA (1998) Material characterization of human medial collateral ligament. J Biomech Eng Dezember 120(6):757–763
Untaroiu CD, Jacob B, Matt L, Gayzik F (2018) Development and preliminary validation of a 50th Percentile Pedestrian Finite element Model. J Biomech Eng 140(1):28877309
Getgood A, Brown C, Lording T, Amis A, Claes S, Geeslin A (2019) u. a. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc 27(1):166–176
Noyes FR, Huser LE, Levy MS (2017) Rotational knee instability in ACL-Deficient knees: role of the Anterolateral Ligament and Iliotibial Band as defined by Tibiofemoral Compartment translations and rotations. J Bone Joint Surg Am 15 Februar 99(4):305–314
Sonnery-Cottet B, Barbosa NC, Vieira TD, Saithna A (2018) Clinical outcomes of extra-articular tenodesis/anterolateral reconstruction in the ACL injured knee. Knee Surg Sports Traumatol Arthrosc off J ESSKA Februar 26(2):596–604
Hamido F, Habiba AA, Marwan Y, Soliman ASI, Elkhadrawe TA, Morsi MG (2021) u. a. anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc off J ESSKA April 29(4):1173–1180
Helito CP, Camargo DB, Sobrado MF, Bonadio MB, Giglio PN, Pécora JR (2018) u. a. combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc off J ESSKA Dezember 26(12):3652–3659
Inderhaug E, Stephen JM, Williams A, Amis AA (2017) Anterolateral Tenodesis or Anterolateral Ligament Complex Reconstruction: Effect of Flexion Angle at graft fixation when combined with ACL Reconstruction. Am J Sports Med November 45(13):3089–3097
Nitri M, Rasmussen MT, Williams BT, Moulton SG, Cruz RS, Dornan GJ (2016) u. a. An in Vitro Robotic Assessment of the Anterolateral Ligament, Part 2: Anterolateral Ligament Reconstruction Combined with Anterior Cruciate Ligament Reconstruction. Am J Sports Med 44(3):593–601
Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L (2016) u. a. The involvement of the Anterolateral Ligament in Rotational Control of the knee. Am J Sports Med Mai 44(5):1209–1214
Grassi A, Smiley SP, Sarsina T, Signorelli C, Marcheggiani Muccioli GM, Bondi A (2017) u. a. mechanisms and situations of anterior cruciate ligament injuries in professional. Eur J Orthop Surg Traumatol 27(7):967–981
Olsen OE, Myklebust G, Engebretsen L, Bahr R (2004) Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med Juni 32(4):1002–1012
Elkin JL, Zamora E, Gallo RA (2019) Combined anterior cruciate ligament and medial collateral ligament knee injuries. Curr Rev Musculoskelet Med 12(2):239–244
Koga H, Nakamae A, Shima Y, Iwasa J, Myklebust G, Engebretsen L (2010) u. a. mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med November 38(11):2218–2225
Behrendt P, Herbst E, Robinson J, Negenborn L, Raschke M, Wermers J (2022) u. a. The control of Anteromedial Rotatory instability is improved with combined flat sMCL and Anteromedial Reconstruction. Am J Sports Med 50(8):2093–2101
Miyaji N, Holthof S, Ball S, Williams A, Amis A (2022) Medial collateral Ligament Reconstruction for Anteromedial instability of the knee: a Biomechanical Study in Vitro. Am J Sports Med 50(7):1823–1831
Acknowledgements
Not applicable.
Funding
There is no funding source.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All six authors made substantial contributions to the conception, design, acquisition, analysis and interpretation of data for the work. Moreover, all authors took part in drafting the work and revising it critically for important intellectual content. All authors participated in the final approval of the version to be published and are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in this study were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not necessary because no patients were included in present FE study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Blanke, F., Boljen, M., Oehler, N. et al. An anteromedial stabilization procedure has the most protective effect on the anterior cruciate ligament in tibial external rotation. A human knee model study. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05357-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05357-8