Abstract
Introduction
Reduced bone mineral density (BMD) and disruption of normal bony architecture are the characteristics of osteopenia and osteoporosis and in patients undergoing total hip arthroplasty (THA) may cause failure of trabecular ingrowth. The purpose of this study is to evaluate the impact of reduced BMD on outcomes following primary elective THA.
Methods
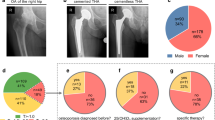
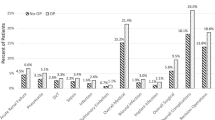
A retrospective chart review of 650 elective THAs with a DEXA scan in their electronic health record (EHR) from 2011 to 2020 was conducted at an urban, academic center and a regional, health center. Patients were separated into three cohorts based on their t-score and the World Health Organizations definitions: normal (t-score ≥ − 1), osteopenia (t-score < − 1.0 and > − 2.5), and osteoporosis (t-score ≤ − 2.5). Demographic and outcome data were assessed. Subsidence was assessed for patients with non-cemented THAs. Regression models were used to account for demographic differences.
Results
650 elective THAs, of which only 11 were cemented, were included in the study. Patients with osteopenia and osteoporosis were significantly older than those without (p = 0.002 and p < 0.0001, respectively) and had a lower BMI (p < 0.0001 and p < 0.0001, respectively). PFx was significantly greater in patients with osteoporosis when compared to those with normal BMD (6.5% vs. 1.0%; p = 0.04). No such difference was found between osteoporotic and osteopenic patients. The revision rate was significantly higher for osteoporotic patients than osteopenic patients (7.5% vs. 1.5%; p = 0.04). No such difference was found between the other comparison groups.
Conclusion
Patients with osteoporosis were older with reduced BMI and had increased PFx after non-cemented elective THA. Understanding this can help surgeons formulate an appropriate preoperative plan for the treatment of patients with osteoporotic bone undergoing elective THA.
Similar content being viewed by others
Data availability
The datasets generated and analyzed during the study are not publicly available, but may be available from the corresponding author upon reasonable request.
References
Domingues VR, de Campos GC, Plapler PG, de Rezende MU (2015) Prevalence of osteoporosis in patients awaiting total hip arthroplasty. Acta Ortop Bras. https://doi.org/10.1590/1413-78522015230100981
Porter JL, Varacallo M (2022) Osteoporosis. In: StatPearls. StatPearls Publishing, Treasure Island (FL)
Office of the Surgeon General (US) (2004) The Frequency of Bone Disease Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville
Varacallo M, Seaman TJ, Jandu JS, Pizzutillo P (2022) Osteopenia. In: StatPearls. StatPearls Publishing, Treasure Island (FL)
Bernatz JT, Brooks AE, Nguyen BP, Shin ED, Binkley NC, Anderson PA et al (2020) Prevalence and treatment of osteoporosis prior to elective shoulder arthroplasty. JAAOS. https://doi.org/10.5435/JAAOSGlobal-D-20-00204
Rhyu KH, Lee SM, Chun YS, Kim K, Cho YJ, Yoo MC (2012) Does osteoporosis increase early subsidence of cementless double-tapered femoral stem in hip arthroplasty? J Arthroplasty. https://doi.org/10.1016/j.arth.2011.10.026
Karuppal R (2016) Biological fixation of total hip arthroplasty: facts and factors. J Orthop. https://doi.org/10.1016/j.jor.2016.06.002
Aro HT, Alm JJ, Moritz N, Mäkinen TJ, Lankinen P (2012) Low BMD affects initial stability and delays stem osseointegration in cementless total hip arthroplasty in women: a 2-year RSA study of 39 patients. Acta Orthop 83:107–114. https://doi.org/10.3109/17453674.2012.678798
Maier GS, Kolbow K, Lazovic D, Maus U (2016) The importance of bone mineral density in hip arthroplasty: results of a survey asking orthopaedic surgeons about their opinions and attitudes concerning osteoporosis and hip arthroplasty. Adv Orthop 2016:8079354. https://doi.org/10.1155/2016/8079354
Demontiero O, Vidal C, Duque G (2012) Aging and bone loss: new insights for the clinician. Ther Adv Musculoskelet Dis. https://doi.org/10.1177/1759720X11430858
Kligman M, Kirsh G (2000) Hydroxyapatite-coated total hip arthroplasty in osteoporotic patients. Bull Hosp Jt Dis 59(3):136–139
Akkawi I, Zmerly H (2018) Osteoporosis: current concepts. Joints. https://doi.org/10.1055/s-0038-1660790
Clair AJ, Gabor JA, Patel KS, Friedlander S, Deshmukh AJ, Schwarzkopf R (2020) Subsidence following revision total hip arthroplasty using modular and monolithic components. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.03.008
Ries C, Boese CK, Dietrich F, Miehlke W, Heisel C (2019) Femoral stem subsidence in cementless total hip arthroplasty: a retrospective single-centre study. Int Orthop. https://doi.org/10.1007/s00264-018-4020-x
Karaguzel G, Holick MF (2010) Diagnosis and treatment of osteopenia. Rev Endocr Metab Disord 11:237–251. https://doi.org/10.1007/s11154-010-9154-0
Yang C, Han X, Wang J, Yuan Z, Wang T, Zhao M et al (2019) Cemented versus uncemented femoral component total hip arthroplasty in elderly patients with primary osteoporosis: retrospective analysis with 5-year follow-up. J Int Med Res. https://doi.org/10.1177/0300060518825428
DeMik DE, Carender CN, Kohler JG, An Q, Brown TS, Bedard NA (2022) Recent increases in outpatient total hip arthroplasty have not increased early complications. J Arthroplasty 37:325-329.e1. https://doi.org/10.1016/j.arth.2021.11.003
Sheehy AM, Caponi B, Gangireddy S, Hamedani AG, Pothof JJ, Siegal E et al (2014) Observation and inpatient status: clinical impact of the 2-midnight rule. J Hosp Med 9:203–209. https://doi.org/10.1002/jhm.2163
DeMik DE, Carender CN, Glass NA, Callaghan JJ, Bedard NA (2021) Home discharge has increased after total hip arthroplasty, however rates vary between large databases. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.08.039
Burn E, Edwards CJ, Murray DW, Silman A, Cooper C, Arden NK et al (2018) Trends and determinants of length of stay and hospital reimbursement following knee and hip replacement: evidence from linked primary care and NHS hospital records from 1997 to 2014. BMJ Open. https://doi.org/10.1136/bmjopen-2017-019146
Giaretta S, Momoli A, Porcelli G, Micheloni GM (2019) Diagnosis and management of periprosthetic femoral fractures after hip arthroplasty. Injury 50(Suppl 2):S29-33. https://doi.org/10.1016/j.injury.2019.01.053
Pavone V, de Cristo C, di Stefano A, Costarella L, Testa G, Sessa G (2019) Periprosthetic femoral fractures after total hip arthroplasty: an algorithm of treatment. Injury 50(Suppl 2):S45-51. https://doi.org/10.1016/j.injury.2019.01.044
Lee S-W, Kim W-Y, Song J-H, Kim J-H, Lee H-H (2021) Factors affecting periprosthetic bone loss after hip arthroplasty. Hip Pelvis 33:53–61. https://doi.org/10.5371/hp.2021.33.2.53
Sheth NP, Nelson CL, Paprosky WG (2013) Femoral bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg 21:601–612. https://doi.org/10.5435/JAAOS-21-10-601
Delsmann MM, Strahl A, Mühlenfeld M, Jandl NM, Beil FT, Ries C et al (2021) High prevalence and undertreatment of osteoporosis in elderly patients undergoing total hip arthroplasty. Osteop Int. https://doi.org/10.1007/s00198-021-05881-y
Bernatz JT, Brooks AE, Squire MW, Illgen RI, Binkley NC, Anderson PA (2019) Osteoporosis is common and undertreated prior to total joint arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.03.044
Khatod M, Inacio MCS, Dell RM, Bini SA, Paxton EW, Namba RS (2015) Association of bisphosphonate use and risk of revision after THA: outcomes from a US Total Joint Replacement Registry. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-015-4263-4
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fiedler, B., Patel, V., Lygrisse, K.A. et al. The effect of reduced bone mineral density on elective total hip arthroplasty outcomes. Arch Orthop Trauma Surg 143, 5993–5999 (2023). https://doi.org/10.1007/s00402-023-04830-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04830-0