Abstract
Background
Despite advancements in total hip arthroplasty (THA) and the increased utilization of tranexamic acid, acute blood loss anemia necessitating allogeneic blood transfusion persists as a post-operative complication. The prevalence of allogeneic blood transfusion in primary THA has been reported to be as high as 9%. Therefore, this study aimed to develop and validate novel machine learning models for the prediction of transfusion rates following primary total hip arthroplasty.
Methods
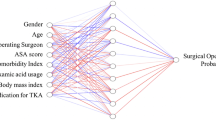
A total of 7265 consecutive patients who underwent primary total hip arthroplasty were evaluated using a single tertiary referral institution database. Patient charts were manually reviewed to identify patient demographics and surgical variables that may be associated with transfusion rates. Four state-of-the-art machine learning algorithms were developed to predict transfusion rates following primary THA, and these models were assessed by discrimination, calibration, and decision curve analysis.
Results
The factors most significantly associated with transfusion rates include tranexamic acid usage, bleeding disorders, and pre-operative hematocrit (< 33%). The four machine learning models all achieved excellent performance across discrimination (AUC > 0.78), calibration, and decision curve analysis.
Conclusion
This study developed machine learning models for the prediction of patient-specific transfusion rates following primary total hip arthroplasty. The results represent a novel application of machine learning, and has the potential to improve outcomes and pre-operative planning.
Level of evidence
III, case–control retrospective analysis.



Similar content being viewed by others
References
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The safety of tranexamic acid in total joint arthroplasty: a direct meta-analysis. J Arthroplasty 33:3070-3082.e1. https://doi.org/10.1016/j.arth.2018.03.031
Bedard NA, Pugely AJ, Lux NR et al (2017) Recent trends in blood utilization after primary hip and knee arthroplasty. J Arthroplasty 32:724–727. https://doi.org/10.1016/j.arth.2016.09.026
Houston BL, Fergusson DA, Falk J et al (2020) Evaluation of transfusion practices in noncardiac surgeries at high risk for red blood cell transfusion: a retrospective cohort study. Transfus Med Rev. https://doi.org/10.1016/j.tmrv.2020.08.001
Menendez ME, Lu N, Huybrechts KF et al (2016) Variation in use of blood transfusion in primary total hip and knee arthroplasties. J Arthroplasty 31:2757-2763.e2. https://doi.org/10.1016/j.arth.2016.05.022
Bert JM, Hooper J, Moen S (2017) Outpatient total joint arthroplasty. Curr Rev Musculoskelet Med 10:567–574. https://doi.org/10.1007/s12178-017-9451-2
Dorenkamp BC, Janssen MK, Janssen ME (2019) Improving blood product utilization at an ambulatory surgery center: a retrospective cohort study on 50 patients with lumbar disc replacement. Patient Saf Surg 13:45–51. https://doi.org/10.1186/s13037-019-0226-0
Kehlet H, Søballe K (2010) Fast-track hip and knee replacement—what are the issues? Acta Orthop 81:271–272
Toy PC, Fournier MN, Throckmorton TW, Mihalko WM (2018) Low rates of adverse events following ambulatory outpatient total hip arthroplasty at a free-standing surgery center. J Arthroplasty 33:46–50. https://doi.org/10.1016/j.arth.2017.08.026
Pennestrì F, Maffulli N, Sirtori P et al (2019) Blood management in fast-track orthopedic surgery: an evidence-based narrative review. J Orthop Surg Res 14:263–269. https://doi.org/10.1186/s13018-019-1296-5
Cao G, Huang Z, Huang Q et al (2018) Incidence and risk factors for blood transfusion in simultaneous bilateral total joint arthroplasty: a multicenter retrospective study. J Arthroplasty 33:2087–2091. https://doi.org/10.1016/j.arth.2018.02.041
Song K, Pan P, Yao Y et al (2019) The incidence and risk factors for allogenic blood transfusion in total knee and hip arthroplasty. J Orthop Surg Res 14:273–278. https://doi.org/10.1186/s13018-019-1329-0
Newman JM, Webb MR, Klika AK et al (2017) Quantifying blood loss and transfusion risk after primary vs conversion total hip arthroplasty. J Arthroplasty 32:1902–1909. https://doi.org/10.1016/j.arth.2017.01.038
Ramkumar PN, Haeberle HS, Bloomfield MR et al (2019) Artificial intelligence and arthroplasty at a single institution: real-world applications of machine learning to big data, value-based care, mobile health, and remote patient monitoring. J Arthroplasty 34:2204–2209. https://doi.org/10.1016/j.arth.2019.06.018
Bini SA (2018) Artificial intelligence, machine learning, deep learning, and cognitive computing: what do these terms mean and how will they impact health care? J Arthroplasty 33:2358–2361. https://doi.org/10.1016/j.arth.2018.02.067
Obermeyer Z, Emanuel EJ (2016) Predicting the future—big data, machine learning, and clinical medicine. N Engl J Med 375:1216–1219. https://doi.org/10.1056/NEJMp1606181
Kimball CC, Nichols CI, Vose JG (2019) Blood transfusion trends in primary and revision total joint arthroplasty: recent declines are not shared equally. J Am Acad Orthop Surg 27:e920–e927. https://doi.org/10.5435/JAAOS-D-18-00205
Burnett RA, Bedard NA, DeMik DE et al (2017) Recent trends in blood utilization after revision hip and knee arthroplasty. J Arthroplasty 32:3693–3697. https://doi.org/10.1016/j.arth.2017.08.038
Karhade AV, Schwab JH, Bedair HS (2019) Development of machine learning algorithms for prediction of sustained postoperative opioid prescriptions after total hip arthroplasty. J Arthroplasty 34:2272-2277.e1. https://doi.org/10.1016/j.arth.2019.06.013
Haeberle HS, Helm JM, Navarro SM et al (2019) Artificial intelligence and machine learning in lower extremity arthroplasty: a review. J Arthroplasty 34:2201–2203. https://doi.org/10.1016/j.arth.2019.05.055
Helm JM, Swiergosz AM, Haeberle HS et al (2020) Machine learning and artificial intelligence: definitions, applications, and future directions. Curr Rev Musculoskelet Med 13:69–76. https://doi.org/10.1007/s12178-020-09600-8
Pempe C, Werdehausen R, Pieroh P et al (2021) Predictors for blood loss and transfusion frequency to guide blood saving programs in primary knee- and hip-arthroplasty. Sci Rep 11:4386–4392. https://doi.org/10.1038/s41598-021-82779-z
Erben H-C, Hess F, Welter J et al (2021) Perioperative blood transfusions in hip and knee arthroplasty: a retrospective assessment of combined risk factors. Arch Orthop Trauma Surg 11:23–29. https://doi.org/10.1007/s00402-021-03763-w
Slover J, Lavery JA, Schwarzkopf R et al (2017) Incidence and risk factors for blood transfusion in total joint arthroplasty: analysis of a statewide database. J Arthroplasty 32:2684-2687.e1. https://doi.org/10.1016/j.arth.2017.04.048
To J, Sinha R, Kim SW et al (2017) Predicting perioperative transfusion in elective hip and knee arthroplasty: a validated predictive model. Anesthesiology 127:317–325. https://doi.org/10.1097/ALN.0000000000001709
Bailey A, Eisen I, Palmer A et al (2021) Preoperative anemia in primary arthroplasty patients-prevalence, influence on outcome, and the effect of treatment. J Arthroplasty 14:71–77. https://doi.org/10.1016/j.arth.2021.01.018
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The efficacy of tranexamic acid in total knee arthroplasty: a network meta-analysis. J Arthroplasty 33:3090-3098.e1. https://doi.org/10.1016/j.arth.2018.04.043
Fillingham YA, Ramkumar DB, Jevsevar DS et al (2018) The efficacy of tranexamic acid in total hip arthroplasty: a network meta-analysis. J Arthroplasty 33:3083-3089.e4. https://doi.org/10.1016/j.arth.2018.06.023
Melvin JS, Stryker LS, Sierra RJ (2015) Tranexamic acid in hip and knee arthroplasty. J Am Acad Orthop Surg 23:732–740. https://doi.org/10.5435/JAAOS-D-14-00223
Liu D, Dan M, Martinez Martos S, Beller E (2016) Blood management strategies in total knee arthroplasty. Knee Surg Relat Res 28:179–187. https://doi.org/10.5792/ksrr.2016.28.3.179
Hines JT, Hernandez NM, Amundson AW et al (2019) Intravenous tranexamic acid safely and effectively reduces transfusion rates in revision total hip arthroplasty. Bone Joint J 101:104–109. https://doi.org/10.1302/0301-620X.101B6.BJJ-2018-1376.R1
Hines JT, Petis SM, Amundson AW et al (2020) Intravenous tranexamic acid safely and effectively reduces transfusion rates in revision total knee arthroplasties. J Bone Joint Surg Am 102:381–387. https://doi.org/10.2106/JBJS.19.00857
Fillingham YA, Darrith B, Calkins TE et al (2019) 2019 Mark coventry award: a multicentre randomized clinical trial of tranexamic acid in revision total knee arthroplasty: does the dosing regimen matter? Bone Joint J 33:49–56. https://doi.org/10.1302/0301-620X.101B7.BJJ-2018-1451.R1
Levine BR, Haughom BD, Belkin MN, Goldstein ZH (2014) Weighted versus uniform dose of tranexamic acid in patients undergoing primary, elective knee arthroplasty: a prospective randomized controlled trial. J Arthroplasty 29:186–188. https://doi.org/10.1016/j.arth.2014.01.038
Abdel MP, Chalmers BP, Taunton MJ et al (2018) Intravenous versus topical tranexamic acid in total knee arthroplasty: both effective in a randomized clinical trial of 640 patients. J Bone Joint Surg Am 100:1023–1029. https://doi.org/10.2106/JBJS.17.00908
Gomez-Barrena E, Ortega-Andreu M, Padilla-Eguiluz NG et al (2014) Topical intra-articular compared with intravenous tranexamic acid to reduce blood loss in primary total knee replacement: a double-blind, randomized, controlled, noninferiority clinical trial. J Bone Joint Surg Am 96:1937–1944. https://doi.org/10.2106/JBJS.N.00060
Donovan RL, Lostis E, Jones I, Whitehouse MR (2021) Estimation of blood volume and blood loss in primary total hip and knee replacement: an analysis of formulae for perioperative calculations and their ability to predict length of stay and blood transfusion requirements. J Orthop 24:227–232. https://doi.org/10.1016/j.jor.2021.03.004
Carling MS, Jeppsson A, Eriksson BI, Brisby H (2015) Transfusions and blood loss in total hip and knee arthroplasty: a prospective observational study. J Orthop Surg Res 10:48–55. https://doi.org/10.1186/s13018-015-0188-6
Klemt C, Harvey MJ, Robinson MG et al (2022) Machine learning algorithms predict extended postoperative opioid use in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 7:61–68. https://doi.org/10.1007/s00167-021-06812-4
Yeo I, Klemt C, Robinson MG et al (2022) The use of artificial neural networks for the prediction of surgical site infection following TKA. J Knee Surg 43:13–19. https://doi.org/10.1055/s-0041-1741396
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained for the retrospective patient chart review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cohen-Levy, W.B., Klemt, C., Tirumala, V. et al. Artificial neural networks for the prediction of transfusion rates in primary total hip arthroplasty. Arch Orthop Trauma Surg 143, 1643–1650 (2023). https://doi.org/10.1007/s00402-022-04391-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04391-8