Abstract
Introduction
The rationale of focal articular prosthetic resurfacing used as a primary arthroplasty procedure in the treatment of articular cartilage defects is still under debate. Conflicting reports raise concern about high rates of re-operations and continued development of osteoarthritis, while others have reported good outcomes. The goal of this paper is to present the long-term results of two patients with a 12-year follow-up and to report the results of a literature review.
Materials and methods
Two patients (male, 70 years; female 63 years) with a follow-up of 12 years were reviewed. Patients were evaluated with standard radiographs to assess the progression of osteoarthritis (OA), a clinical examination including the Knee Injury and Osteoarthritis Outcome Score (KOOS) and Tegner activity scale. The literature review was performed using the search terms HemiCAP, focal, femoral, condyle, inlay, and resurfacing to identify articles published in the English language up until September 25, 2016.
Results
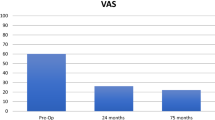
The clinical and radiographic follow-ups of the patients were 11.9 and 11.8 years, respectively. Both patients were satisfied with their outcome and would have the operation again. Comparing the first postoperative to 12-year follow-up X-rays, the radiographic results demonstrated no signs of periprosthetic loosening, preservation of joint space, and no change in the osteoarthritic stage. KOOS Scores were 86 and 83 for pain, 89 and 93 for symptoms, 88 and 100 for activities of daily living (ADL), 75 and 65 for sports and recreation, and 75 and 81 for quality of life (QOL). The Tegner activity level was 5 and 4. The literature review comprised 6 studies with 169 focal articular prosthetic resurfacing procedures in 169 patients (84 male, 85 female) with a mean age at implantation ranging from 44.7 to 53.7 years and a follow-up range of 20 months to 7 years. Five studies were classified as level 4 and one as level 3. Clinical and radiographic results showed mainly good to excellent outcomes but were different among the studies depending on the indication. Re-operation rates ranged from 0 to 23% depending on the length of follow-up.
Conclusions
The results suggest that focal articular prosthetic resurfacing is an effective and safe treatment option in selected cases.


Similar content being viewed by others
References
(2015) Australian Orthopaedic Association National Joint Replacement Registry (ed)
Becher C, Huber R, Thermann H, Tibesku CO, von Skrbensky G (2009) Tibiofemoral contact mechanics with a femoral resurfacing prosthesis and a non-functional meniscus. Clin Biomech (Bristol, Avon) 24(8):648–654
Becher C, Kalbe C, Thermann H et al (2011) Minimum 5-year results of focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee. Arch Orthop Trauma Surg 131(8):1135–1143
Bekkers JE, de Windt TS, Raijmakers NJ, Dhert WJ, Saris DB (2009) Validation of the Knee Injury and Osteoarthritis Outcome Score (KOOS) for the treatment of focal cartilage lesions. Osteoarthr Cartil 17(11):1434–1439
Bollars P, Bosquet M, Vandekerckhove B, Hardeman F, Bellemans J (2012) Prosthetic inlay resurfacing for the treatment of focal, full thickness cartilage defects of the femoral condyle: a bridge between biologics and conventional arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(9):1753–1759
Briggs DT, Sadr KN, Pulido PA, Bugbee WD (2015) The use of osteochondral allograft transplantation for primary treatment of cartilage lesions in the knee. Cartilage 6(4):203–207
Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 10(1):2–11
Dhollander AA, Almqvist KF, Moens K et al (2015) The use of a prosthetic inlay resurfacing as a salvage procedure for a failed cartilage repair. Knee Surg Sports Traumatol Arthrosc 23(8):2208–2212
Goebel L, Kohn D, Madry H (2016) Biological reconstruction of the osteochondral unit after failed focal resurfacing of a chondral defect in the knee. Am J Sports Med 44(11):2911–2916
Goyal D, Keyhani S, Goyal A, Lee EH, Hui JH, Vaziri AS (2014) Evidence-based status of osteochondral cylinder transfer techniques: a systematic review of level I and II studies. Arthroscopy 30(4):497–505
Hambly K, Griva K (2008) IKDC or KOOS? Which measures symptoms and disabilities most important to postoperative articular cartilage repair patients? Am J Sports Med 36(9):1695–1704
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Jt Surg Am 85-A(Suppl 2):25–32
Hobbs H, Ketse-Matiwani N, Van der Merwe W, Posthumus M (2013) Focal full thickness articular cartilage lesions treated with an articular resurfacing prosthesis in the middle-aged. S Afr Orthop J 12(4):6
Jungmann PM, Salzmann GM, Schmal H, Pestka JM, Sudkamp NP, Niemeyer P (2012) Autologous chondrocyte implantation for treatment of cartilage defects of the knee: what predicts the need for reintervention? Am J Sports Med 40(1):58–67
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kirker-Head CA, Van Sickle DC, Ek SW, McCool JC (2006) Safety of, and biological and functional response to, a novel metallic implant for the management of focal full-thickness cartilage defects: preliminary assessment in an animal model out to 1 year. J Orthop Res 24(5):1095–1108
Knutsen G, Drogset JO, Engebretsen L et al (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Jt Surg Am 89(10):2105–2112
Kon E, Verdonk P, Condello V et al (2009) Matrix-assisted autologous chondrocyte transplantation for the repair of cartilage defects of the knee: systematic clinical data review and study quality analysis. Am J Sports Med 37(Suppl 1):156S–166S
Kreuz PC, Erggelet C, Steinwachs MR et al (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22(11):1180–1186
Laursen JO, Lind M (2015) Treatment of full-thickness femoral cartilage lesions using condyle resurfacing prosthesis. Knee Surg Sports Traumatol Arthrosc 25(3):746–751
Maier MW, Kuhs F, Streit MR et al (2015) Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg 135(8):1169–1175
Manda K, Ryd L, Eriksson A (2011) Finite element simulations of a focal knee resurfacing implant applied to localized cartilage defects in a sheep model. J Biomech 44(5):794–801
Martinez-Carranza N, Berg HE, Hultenby K, Nurmi-Sandh H, Ryd L, Lagerstedt AS (2013) Focal knee resurfacing and effects of surgical precision on opposing cartilage. A pilot study on 12 sheep. Osteoarthr Cartil 21(5):739–745
Martinez-Carranza N, Ryd L, Hultenby K et al (2016) Treatment of full thickness focal cartilage lesions with a metallic resurfacing implant in a sheep animal model, 1 year evaluation. Osteoarthr Cartil 24(3):484–493
Mobasheri A, Kalamegam G, Musumeci G, Batt ME (2014) Chondrocyte and mesenchymal stem cell-based therapies for cartilage repair in osteoarthritis and related orthopaedic conditions. Maturitas 78(3):188–198
Niemeyer P, Feucht MJ, Fritz J, Albrecht D, Spahn G, Angele P (2016) Cartilage repair surgery for full-thickness defects of the knee in Germany: indications and epidemiological data from the German Cartilage Registry (KnorpelRegister DGOU). Arch Orthop Trauma Surg 136(7):891–897
Oussedik S, Tsitskaris K, Parker D (2015) Treatment of articular cartilage lesions of the knee by microfracture or autologous chondrocyte implantation: a systematic review. Arthroscopy 31(4):732–744
Pascual-Garrido C, Daley E, Verma NN, Cole BJ (2016) A Comparison of the outcomes for cartilage defects of the knee treated with biologic resurfacing versus focal metallic implants. Arthroscopy 33(2):364–373
Peterson L, Minas T, Brittberg M, Lindahl A (2003) Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am 85-A(Suppl 2):17–24
Petri M, Ettinger M, von Falck C, Hawi N, Jagodzinski M, Haasper C (2013) Reconstruction of osteochondral defects by combined bone grafting and a bilayer collagen membrane as a sandwich technique. Orthop Rev (Pavia) 5(4):e36
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96
Saris D, Price A, Widuchowski W et al (2014) Matrix-applied characterized autologous cultured chondrocytes versus microfracture: two-year follow-up of a prospective randomized trial. Am J Sports Med 42(6):1384–1394
Saris DB, Vanlauwe J, Victor J et al (2009) Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med 37(Suppl 1):10S–19S
Spahn G, Fritz J, Albrecht D, Hofmann GO, Niemeyer P (2016) Characteristics and associated factors of Klee cartilage lesions: preliminary baseline-data of more than 1000 patients from the German cartilage registry (KnorpelRegister DGOU). Arch Orthop Trauma Surg 136(6):805–810
Steadman JR, Rodkey WG, Rodrigo JJ (2001) Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res 391 Suppl:S362–S369
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Wood JJ, Malek MA, Frassica FJ et al (2006) Autologous cultured chondrocytes: adverse events reported to the United States Food and Drug Administration. J Bone Jt Surg Am 88(3):503–507
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A(1):1–3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A fee for speaking and reimbursement for attending a symposium was received by the corresponding author from 2med GmbH, Hamburg, Germany (Distributor of Arthrosurface in Germany) in 2015. The authors declare no other conflict of interest.
Funding
There is no funding source.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. The follow-up examinations were performed on a regular base of follow-up and not for study reasons.
Informed consent
Informed consent was obtained from both participants included in the report of the two cases.
Rights and permissions
About this article
Cite this article
Becher, C., Cantiller, E.B. Focal articular prosthetic resurfacing for the treatment of full-thickness articular cartilage defects in the knee: 12-year follow-up of two cases and review of the literature. Arch Orthop Trauma Surg 137, 1307–1317 (2017). https://doi.org/10.1007/s00402-017-2717-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2717-8