Abstract
Introduction
The goal of this retrospective study was to compare the long-term results after implantation of the nonresorbable glass–ceramic material and transplantation of the cancellous allografts into the defects of long bones.
Method
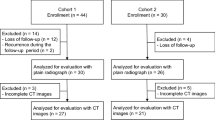
The bone cysts were excochleated and filled using granules of glass–ceramic material or cancellous allografts. Clinical, radiographic and scintigraphic examinations of 30 patients were carried out 2–14 years after their surgery.
Results
Though signs of complete incorporation allowing full weight-bearing capacity were observed on plain radiographs, we detected pain in six out of nine patients after diaphyseal implantation of nonresorbable glass–ceramic. We found an increase in 99 mTc-methylene diphosphonate uptake on the delayed images in the area of glass–ceramic implantation, mainly in its diaphyseal location. In patients after bone transplantation, the cancellous allografts were completely integrated and the scintigraphic findings were physiological.
Conclusion
The implantation of the nonresorbable glass–ceramic material into the diaphyseal defects of long bones is not suitable based on our study.






Similar content being viewed by others
References
Acharya NK, Kumar RJ, Varma HK, Menon VK (2008) Hydroxyapatite-bioactive glass ceramic composite as stand-alone graft substitute for posterolateral vision of lumbar spine: a prospective, matched, and controlled study. J Spinal Disord Tech 21:106–111. doi:10.1097/BSD.0b013e31805fea1f
Aho AJ, Suominen E, Alanen A, Yli-Urpo A, Knuuti J, Aho HJ (2003) Remodeling of the tibia after grafting of a large cavity with particulate bioactive glass- hydroxyapatite: case report on treatment of fibrous dysplasia with 13 years′ follow-up. Acta Orthop Scand 74:766–770. doi:10.1080/00016470310018342
Andersson OH, Liu G, Karlsson KH (1990) In vivo behaviour of glasses in the SiO2–Na2O–CaO–P2O5–Al2O3–B2O3 system. J Mater Sci 1:219–227. doi:10.1007/BF00701080
Asano S, Kaneda K, Satoh S, Abumi K, Hashimoto T, Fujiya M (1994) Reconstruction of an iliac crest defect with a bioactive ceramic prosthesis. Eur Spine J 3:39–44. doi:10.1007/BF02428315
Athanasiou KA, Zhu C, Lanctot DR, Agrawal CM, Wang X (2000) Fundamentals of biomechanics in tissue engineering of bone. Tissue Eng 6:361–381. doi:10.1089/107632700418083
Bucholz RW, Carlton A, Holmes R (1989) Interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Clin Orthop Relat Res 240:53–62
Damien E, Revell PA (2004) Coralline hydroxyapatite bone graft substitute: a review of experimental studies and biomedical applications. J App Biomater Biomech 2:65–73
DeLong WG, Einhorn TA, Koval K, McKee M, Smith W, Sanders R, Watson T (2007) Bone grafts and bone graft substitutes in orthopaedic trauma surgery. J Bone Joint Surg 89-A:649–658. doi:10.2106/JBJS.F.00465
Duffy PJ, Masri BA, Garbuz DS, Duncan CP (2005) Evaluation of patients with pain following total hip replacement. J Bone Joint Surg 87-A:2566–2575
Duskova M, Kozak J, Mazanek J, Smahel Z (2000) Augmentation of facial skeleton with ceramics in congenital disorders and in post-traumatic or postoperative deformities: a preliminary report. Eur J Plast Surg 23:57–63. doi:10.1007/s002380050016
Finkemeier CG (2002) Bone-grafting and bone-graft substitutes. J Bone Joint Surg 84-A:454–464
Hisatome T, Yasunaga Y, Takahashi K, Ochi M (2004) Bone remodelling after impacted cancellous allograft in revision hip arthoplasty based on 99mTc-MDP bone scintigraphy. Arch Orthop Trauma Surg 124:52–55. doi:10.1007/s00402-003-0589-6
Holmes RE, Bucholz RW, Mooney V (1987) Porous hydroxyapatite as a bone graft substitute in diaphyseal defects: a histometric study. J Orthop Res 5:114–121. doi:10.1002/jor.1100050114
Ido K, Asada Y, Sakamoto T, Hayashi R, Kuriyama S (2000) Radiographic evaluation of bioactive glass–ceramic grafts in postero-lateral lumbar fusion. Spinal Cord 38:315–318. doi:10.1038/sj.sc.3100992
Ilharreborde B, Morel E, Fitoussi F, Presedo A, Souchot P, Pennecot GF, Mazda K (2008) Bioactive glass as a bone substitute for spinal vision in adolescent idiopathic scoliosis: a comparative study with iliac crest autograft. J Pediatr Orthop 28:347–351
Ito M, Abumi K, Moridaira H, Shono Y, Kotani Y, Minami A, Kaneda K (2005) Iliac crest reconstruction with a bioactive ceramic spacer. Eur Spine J 14:99–102. doi:10.1007/s00586-004-0765-6
Itokazu M, Matsunaga T, Ishii M, Kusakabe H, Wyni Y (1996) Use of arthroscopy and interporous hydroxyapatite as a bone graft substitute in tibial plateau fractures. Arch Orthop Trauma Surg 115:45–48. doi:10.1007/BF00453217
Matsumine A, Myoui A, Kusazaki K, Araki N, Seto M, Yoshikawa H, Uchida A (2004) Calcium hydroxyapatite ceramic implants in bone tumour surgery: a long-term follow-up study. J Bone Joint Surg 86-B:719–725. doi:10.1302/0301-620X.86B5.14242
Muschler GF, Nakamoto C, Griffith LG (2004) Engineering principles of clinical cell-based tissue engineering. J Bone Joint Surg 86-A:1541–1558
Nigro N, Grace D (1996) Radiographic evaluation of bone grafts. J Foot Ankle Surg 35:378–385
Oswald SG, Van Nostrand D, Savory CG, Callaghan JJ (1989) Three-phase bone scan and indium white blood cell scintigraphy following porous coated hip arthroplasty: a prospective study of the prosthetic tip. J Nucl Med 30:1321–1331
Patka P, Den Hollander W, Den Otter G, Heidendal AK, De Groot K (1985) Scintigraphic studies to evaluate stability of ceramics (hydroxyapatite) in bone replacement. J Nucl Med 26:263–271
Sponer P, Urban K, Karpas K, Urbanova E (2007) Scintigraphic evaluation of osteoblast activity after implantation of BAS-0 bioactive glass-ceramic into long bone defects. J Child Orthop 1:S14
Strnad Z, Barcalova L, Urban K (1989) Surface active glass-ceramic materials. Sklář a keramik 38:292–299
Suominen EA, Aho AJ, Juhanoja J, Yli-Urpo A (1995) Hydroxyapatite-glass composite as a bone substitute in large metaphyseal cavities in rabbits. Int Orthop 19:167–173. doi:10.1007/BF00181863
Uchida A, Araki N, Shinto Y, Yoshikawa H, Kurisaki E, Ono K (1990) The use of calcium hydroxyapatite ceramic in bone tumour surgery. J Bone Joint Surg 72-B:298–302
Urban K (2002) Use of bioactive glass ceramics in the treatment of tibial plateau fractures. Acta Chir Orthop Traumatol Cech 69:295–301
Yamamoto T, Onga T, Marui T, Mizuno K (2000) Use of hydroxyapatite to fill cavities after excision of benign bone tumours. J Bone Joint Surg 82-B:1117–1120. doi:10.1302/0301-620X.82B8.11194
Acknowledgments
This research was supported by a grant from the Grant Agency of Ministry of Health, Prague, Czech Republic.
Conflict of interest statement
None of the authors have a conflict of interest in relation to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Šponer, P., Urban, K., Urbanová, E. et al. Behaviour of nonresorbable bioactive glass–ceramic implanted into long bone defects: comparison with cancellous allografts. Arch Orthop Trauma Surg 129, 1353–1360 (2009). https://doi.org/10.1007/s00402-009-0839-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-009-0839-3