Abstract
Purpose
We assessed the cross-sectional association between healthy dietary patterns [alternate Mediterranean diet (aMED), Dietary Approaches to Stop Hypertension (DASH), alternative Healthy Eating Index (aHEI), and Healthy Eating Index 2015 (HEI-2015)] and urinary biomarkers of oxidative stress.
Methods
Between 2003 and 2009, the Sister Study enrolled 50,884 breast cancer-free US women aged 35 to 74 (non-Hispanic White, 83.7%). Data were analyzed for 844 premenopausal and 454 postmenopausal women who had urine samples analyzed for F2-isoprostanes and non-missing covariate data. Food frequency questionnaire responses were used to calculate dietary pattern scores. Concentrations of 8-iso-prostaglandin F2α (8-iso-PGF2α) and its metabolite (8-iso-PGF2α-M) were measured in urine samples by GC/MS for premenopausal women and LC/MS for postmenopausal women. Multivariable linear regression models were used to estimate associations between aMED, DASH, aHEI, and HEI-2015 and urinary F2-isoprostanes by menopausal status. Effect modification by sociodemographic, lifestyle, and clinical characteristics was also evaluated.
Results
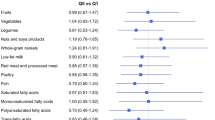
Among premenopausal women, the four dietary indices were inversely associated with 8-iso-PGF2α (aMED βQ4vsQ1: − 0.17, 95% CI − 0.27, − 0.08; DASH βQ4vsQ1: − 0.18, 95% CI − 0.28, − 0.08; aHEI βQ4vsQ1: − 0.20, 95% CI − 0.30, − 0.10; HEI-2015 βQ4vsQ1: − 0.19, 95% CI − 0.29, − 0.10). In contrast, inverse associations with 8-iso-PGF2α-M were found for the continuous aMED, aHEI, and HEI-2015. Associations between dietary indices and 8-iso-PGF2α were generally stronger among younger women, women with lower income, and women with higher BMI. Similar results were observed among postmenopausal women, though only the continuous DASH and aHEI models were statistically significant.
Conclusion
Healthy dietary patterns were associated with lower levels of oxidative stress.
Similar content being viewed by others
Data availability
Data from the Sister Study and analytic code may be obtained by following procedures described on the Sister Study Website [The Sister Study: Collaborations and Data Requests (nih.gov)].
References
Rani V, Deep G, Singh RK, Palle K, Yadav UC (2016) Oxidative stress and metabolic disorders: Pathogenesis and therapeutic strategies. Life Sci 148:183–193. https://doi.org/10.1016/j.lfs.2016.02.002
Lushchak VI (2014) Free radicals, reactive oxygen species, oxidative stress and its classification. Chem Biol Interact 224:164–175. https://doi.org/10.1016/j.cbi.2014.10.016
Kurutas EB (2016) The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutr J 15(1):71. https://doi.org/10.1186/s12937-016-0186-5
Hu L, Wang Z, Carmone C, Keijer J, Zhang D (2021) Role of oxidative DNA damage and repair in atrial fibrillation and ischemic heart disease. Int J Mol Sci 22(8):3838. https://doi.org/10.3390/ijms22083838
Nakayama H, Otsu K (2018) Mitochondrial DNA as an inflammatory mediator in cardiovascular diseases. Biochem J 475(5):839–852. https://doi.org/10.1042/BCJ20170714
Kawanishi S, Ohnishi S, Ma N, Hiraku Y, Murata M (2017) Crosstalk between DNA damage and inflammation in the multiple steps of carcinogenesis. Int J Mol Sci 18(8):1808. https://doi.org/10.3390/ijms18081808
US Preventive Services Task Force, Mangione CM, Barry MJ et al (2022) Vitamin, mineral, and multivitamin supplementation to prevent cardiovascular disease and cancer: US preventive services task force recommendation statement. JAMA 327(23):2326–2333. https://doi.org/10.1001/jama.2022.8970
Tapsell LC, Neale EP, Satija A, Hu FB (2016) Foods, nutrients, and dietary patterns: Interconnections and implications for dietary guidelines. Adv Nutr 7(3):445–454. https://doi.org/10.3945/an.115.011718
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002
Krebs-Smith SM, Subar AF, Reedy J (2015) Examining dietary patterns in relation to chronic disease: matching measures and methods to questions of interest. Circulation 132(9):790–793. https://doi.org/10.1161/CIRCULATIONAHA.115.018010
Aleksandrova K, Koelman L, Rodrigues CE (2021) Dietary patterns and biomarkers of oxidative stress and inflammation: a systematic review of observational and intervention studies. Redox Biol 42:101869. https://doi.org/10.1016/j.redox.2021.101869
Mitjavila MT, Fandos M, Salas-Salvadó J et al (2013) The mediterranean diet improves the systemic lipid and DNA oxidative damage in metabolic syndrome individuals a randomized controlled trial. Clin Nutr. 32(2):172–178. https://doi.org/10.1016/j.clnu.2012.08.002
Bettermann EL, Hartman TJ, Easley KA et al (2018) Higher mediterranean diet quality scores and lower body mass index are associated with a less-oxidized plasma glutathione and cysteine redox status in adults. J Nutr 148(2):245–253. https://doi.org/10.1093/jn/nxx045
Razavi Zade M, Telkabadi MH, Bahmani F, Salehi B, Farshbaf S, Asemi Z (2016) The effects of DASH diet on weight loss and metabolic status in adults with non-alcoholic fatty liver disease: a randomized clinical trial. Liver Int 36(4):563–571. https://doi.org/10.1111/liv.12990
Kim JY, Yang YJ, Yang YK et al (2011) Diet quality scores and oxidative stress in Korean adults. Eur J Clin Nutr 65(12):1271–1278. https://doi.org/10.1038/ejcn.2011.120
Jung S, Smith-Warner SA, Willett WC et al (2016) Healthy dietary patterns and oxidative stress as measured by fluorescent oxidation products in Nurses’ Health Study. Nutrients 8(9):587. https://doi.org/10.3390/nu8090587
Frijhoff J, Winyard PG, Zarkovic N et al (2015) Clinical relevance of biomarkers of oxidative stress. Antioxid Redox Signal 23(14):1144–1170. https://doi.org/10.1089/ars.2015.6317
Milne GL, Yin H, Hardy KD, Davies SS, Roberts LJ 2nd (2011) Isoprostane generation and function. Chem Rev 111(10):5973–5996. https://doi.org/10.1021/cr200160h
Wu X, Cai H, Xiang YB et al (2010) Intra-person variation of urinary biomarkers of oxidative stress and inflammation. Cancer Epidemiol Biomarkers Prev 19(4):947–952. https://doi.org/10.1158/1055-9965.EPI-10-0046
Milne GL, Dai Q, Roberts LJ 2nd (2016) The isoprostanes--25 years later. Biochim Biophys Acta 1851 (4):433-445. https://doi.org/10.1016/j.bbalip.2014.10.007
Dorjgochoo T, Gao YT, Chow WH et al (2012) Major metabolite of F2-isoprostane in urine may be a more sensitive biomarker of oxidative stress than isoprostane itself. Am J Clin Nutr 96(2):405–414. https://doi.org/10.3945/ajcn.112.034918
Sánchez-Rodríguez MA, Zacarías-Flores M, Arronte-Rosales A, Correa-Muñoz E, Mendoza-Núñez VM (2012) Menopause as risk factor for oxidative stress. Menopause 19(3):361–367. https://doi.org/10.1097/gme.0b013e318229977d
Bourgonje MF, Bourgonje AR, Abdulle AE et al (2021) Systemic oxidative stress, aging and the risk of cardiovascular events in the general female population. Front Cardiovasc Med 8:630543. https://doi.org/10.3389/fcvm.2021.630543
Sandler DP, Hodgson ME, Deming-Halverson SL et al (2017) The sister study cohort: baseline methods and participant characteristics. Environ Health Perspect 125(12):127003. https://doi.org/10.1289/EHP1923
Nichols HB, Anderson C, White AJ, Milne GL, Sandler DP (2017) Oxidative stress and breast cancer risk in premenopausal women. Epidemiology 28(5):667–674. https://doi.org/10.1097/EDE.0000000000000685
Park YM, Lilyquist J, Van’t Erve TJ, O’Brien KM, Nichols HB, Milne GL, Weinberg CR, Sandler DP (2022) Association of dietary and plasma carotenoids with urinary F2-isoprostanes. Eur J Nutr 61(5):2711–2723. https://doi.org/10.1007/s00394-022-02837-8
Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L (1986) A data-based approach to diet questionnaire design and testing. Am J Epidemiol 124(3):453–469. https://doi.org/10.1093/oxfordjournals.aje.a114416
Boucher B, Cotterchio M, Kreiger N, Nadalin V, Block T, Block G (2006) Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr 9(1):84–93. https://doi.org/10.1079/phn2005763
Bowman SA, Clemens JC, Friday JE, Thoerig RC,Moshfegh AJ (2014) Food patterns equivalents database 2011–12: Methodology and user guide. Beltsville, Maryland: Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, U.S. Department of Agriculture
Fung TT, Rexrode KM, Mantzoros CS, Manson JE, Willett WC, Hu FB (2009) Mediterranean diet and incidence of and mortality from coronary heart disease and stroke in women. Circulation 119(8):1093–1100. https://doi.org/10.1161/CIRCULATIONAHA.108.816736
Fung TT, Chiuve SE,McCullough ML, Rexrode KM, LogroscinoG,Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women (2008). Arch Intern Med 168 (7): 713–20. https://doi.org/10.1001/archinte.168.7.713
Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC (2012) Alternative dietary indices both strongly predict risk of chronic disease. J Nutr 142(6):1009–1018. https://doi.org/10.3945/jn.111.157222
Krebs-Smith SM, Pannucci TE, Subar AF, Kirkpatrick SI, Lerman JL, Tooze JA, Wilson MM, Reedy J (2018) Update of the healthy eating index: HEI-2015. J Acad Nutr Diet 118(9):1591–1602. https://doi.org/10.1016/j.jand.2018.05.021
Milne GL, Sanchez SC, Musiek ES, Morrow JD (2007) Quantification of F2-isoprostanes as a biomarker of oxidative stress. Nat Protoc 2(1):221–226. https://doi.org/10.1038/nprot.2006.375
Milne GL, Gao B, Terry ES, Zackert WE, Sanchez SC (2013) Measurement of F2-isoprostanes and isofurans using gas chromatography-mass spectrometry. Free Radical Biol Med 59:36–44. https://doi.org/10.1016/j.freeradbiomed.2012.09.030
O’Brien KM, Upson K, Cook NR, Weinberg CR (2016) Environmental chemicals in urine and blood: improving methods for creatinine and lipid adjustment. Environ Health Perspect 124(2):220–227. https://doi.org/10.1289/ehp.1509693
Gaskins AJ, Rovner AJ, Mumford SL et al (2010) Adherence to a Mediterranean diet and plasma concentrations of lipid peroxidation in premenopausal women. Am J Clin Nutr 92(6):1461–1467. https://doi.org/10.3945/ajcn.110.000026
Whalen KA, McCullough ML, Flanders WD, Hartman TJ, Judd S, Bostick RM (2016) Paleolithic and mediterranean diet pattern scores are inversely associated with biomarkers of inflammation and oxidative balance in adults. J Nutr 146(6):1217–1226. https://doi.org/10.3945/jn.115.224048
Davis CR, Bryan J, Hodgson JM, Woodman R, Murphy KJ (2017) A Mediterranean diet reduces F2-Isoprostanes and triglycerides among older Australian men and women after 6 months. J Nutr 147(7):1348–1355. https://doi.org/10.3945/jn.117.248419
Esposito K, Di Palo C, Maiorino MI et al (2010) Long-term effect of mediterranean-style diet and calorie restriction on biomarkers of longevity and oxidative stress in overweight men. Cardiol Res Pract 2011:293916. https://doi.org/10.4061/2011/293916
Patel RS, Ghasemzadeh N, Eapen DJ et al (2016) Novel biomarker of oxidative stress Is associated with risk of death in patients with coronary artery disease. Circulation 133(4):361–369. https://doi.org/10.1161/CIRCULATIONAHA.115.019790
Go YM, Jones DP (2011) Cysteine/cystine redox signaling in cardiovascular disease. Free Radic Biol Med 50(4):495–509. https://doi.org/10.1016/j.freeradbiomed.2010.11.029
Wu T, Willett WC, Rifai N, Rimm EB (2007) Plasma fluorescent oxidation products as potential markers of oxidative stress for epidemiologic studies. Am J Epidemiol 166(5):552–560. https://doi.org/10.1093/aje/kwm119
Gaman M, Epingeac ME, Gad M, Diaconu CC, Gaman AM (2019) Oxidative stress levels are increased in obesity and obesity-related complications. J Hypertens 37:e206–e207
Manna P, Jain SK (2015) Obesity, Oxidative Stress, Adipose Tissue Dysfunction, and the Associated Health Risks: Causes and Therapeutic Strategies. Metab Syndr Relat Disord 13(10):423–444. https://doi.org/10.1089/met.2015.0095
Fernández-Sánchez A, Madrigal-Santillán E, Bautista M et al (2011) Inflammation, oxidative stress, and obesity. Int J Mol Sci 12(5):3117–3132. https://doi.org/10.3390/ijms12053117
Wheatcroft SB, Williams IL, Shah AM, Kearney MT (2003) Pathophysiological implications of insulin resistance on vascular endothelial function. Diabet Med 20(4):255–268. https://doi.org/10.1046/j.1464-5491.2003.00869.x
Martínez JA (2006) Mitochondrial oxidative stress and inflammation: an slalom to obesity and insulin resistance. J Physiol Biochem 62(4):303–306. https://doi.org/10.1007/BF03165759
Pingitore A, Lima GP, Mastorci F, Quinones A, Iervasi G, Vassalle C (2015) Exercise and oxidative stress: potential effects of antioxidant dietary strategies in sports. Nutrition 31(7–8):916–922. https://doi.org/10.1016/j.nut.2015.02.005
Powers SK, Deminice R, Ozdemir M, Yoshihara T, Bomkamp MP, Hyatt H (2020) Exercise-induced oxidative stress: friend or foe? J Sport Health Sci 9(5):415–425. https://doi.org/10.1016/j.jshs.2020.04.001
Radak Z, Chung HY, Koltai E, Taylor AW, Goto S (2008) Exercise, oxidative stress and hormesis. Ageing Res Rev 7(1):34–42. https://doi.org/10.1016/j.arr.2007.04.004
Doshi SB, Agarwal A (2013) The role of oxidative stress in menopause. J Midlife Health 4(3):140–146. https://doi.org/10.4103/0976-7800.118990
Funding
BC is supported by grant number T32-GM081740 from NIH-NIGMS. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIGMS or NIH. This work was supported by the Intramural Research Program of the National Institutes of Health, the National Institute of Environmental Health Sciences [Z01-ES044005], NIH Office of Dietary Supplements Research Scholars Program, and the Avon Foundation [02-2012-085]. This work was also partially supported by a grant from the Arkansas Breast Cancer Research Program.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None reported.
Ethical approval
The Sister Study is overseen by the NIH Institutional Review Board and the University of South Carolina Institutional Review Board (Approval number: Pro00113780).
Consent to participate
Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Crawford, B., Steck, S.E., Sandler, D.P. et al. Association between healthy dietary patterns and markers of oxidative stress in the Sister Study. Eur J Nutr 63, 485–499 (2024). https://doi.org/10.1007/s00394-023-03280-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-023-03280-z