Abstract
Background and aim
Prospective cohort studies have suggested that sugar-sweetened beverages (SSBs) intake is significantly associated with the risk of colorectal cancer (CRC). However, it remains unclear whether this observed association was susceptible to potential confounding factors due to the long-term development process of CRC, and the risk of CRC associated with sweet beverages has rarely been reported. We aimed to investigate the association between SSBs/sweet beverages and CRC risk.
Methods
We performed two-sample Mendelian randomization (MR) analysis using independent genetic variants for SSBs and sweet beverages from a published genome-wide association study (GWAS). Summary statistics for instrument-outcome associations from two databases for malignant neoplasms of the colon and the rectum (FinnGen and UK Biobank). The inverse weighted method (IVW) meta-analysis was the main method used to estimate the relationship, and sensitivity analyses were performed with Cochran’s Q test, leave-one-out analysis, MR–Egger regression, Steiger filtering, and the MR PRESSO test.
Results
Genetically predicted SSBs intake was associated with a higher colonic malignant neoplasms risk (odds ratio (OR): 1.013; 95% confidence interval (CI) 1.001, 1.026; P = 0.036) in a combined sample size of 579,986 individuals (4029 cases). Such a significant causal effect of SSBs on rectal malignant neoplasms or sweet beverages on CRC was not observed.
Conclusion
Our findings corroborated a causal association between SSBs and colonic malignant neoplasms risk but did not support such a relationship in the analysis of the rectal malignant neoplasms nor the sweet beverage intake, which might be interpreted with caution and further confirmed.

Similar content being viewed by others
References
Global Burden of Disease Cancer, C., Kocarnik JM, Compton K et al (2021) Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the global burden of disease study 2019. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2021.6987
Vuik FE, Nieuwenburg SA, Bardou M et al (2019) Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 68:1820–1826. https://doi.org/10.1136/gutjnl-2018-317592
Patel S, May F, Anderson J et al (2021) Updates on age to start and stop colorectal cancer screening: recommendations from the U.S. multi-society task force on colorectal cancer. Gastroenterology. https://doi.org/10.1053/j.gastro.2021.10.007
Schwingshackl L, Schwedhelm C, Hoffmann G et al (2018) Food groups and risk of colorectal cancer. Int J Cancer 142:1748–1758. https://doi.org/10.1002/ijc.31198
Burnett-Hartman AN, Lee JK, Demb J, Gupta S (2021) An update on the epidemiology, molecular characterization, diagnosis, and screening strategies for early-onset colorectal cancer. Gastroenterology 160:1041–1049. https://doi.org/10.1053/j.gastro.2020.12.068
Miller G, Merlo C, Demissie Z et al (2017) Trends in beverage consumption among high school students—United States, 2007–2015. Morb Mortal Wkly Rep 66:112–116. https://doi.org/10.1558/mmwr.mm6604a5
Marriott BP, Hunt KJ, Malek AM, Newman JC (2019) Trends in intake of energy and total sugar from sugar-sweetened beverages in the United States among children and adults, NHANES 2003–2016. Nutrients. https://doi.org/10.3390/nu11092004
Bray GA, Popkin BM (2014) Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes? Health be damned! Pour on the sugar. Diabetes Care 37:950–956. https://doi.org/10.2337/dc13-2085
Park S, Xu F, Town M, Blanck HJMM, Report MW (2016) Prevalence of sugar-sweetened beverage intake among adults—23 States and the District of Columbia, 2013. 65:169–174.https://doi.org/10.15585/mmwr.mm6507a1
Della Corte K, Fife J, Gardner A et al (2021) World trends in sugar-sweetened beverage and dietary sugar intakes in children and adolescents: a systematic review. Nutr Rev 79:274–288. https://doi.org/10.1093/nutrit/nuaa070
Joh H, Lee D, Hur J et al (2021) Simple sugar and sugar-sweetened beverage intake during adolescence and risk of colorectal cancer precursors. Gastroenterology 161:128-142.e120. https://doi.org/10.1053/j.gastro.2021.03.028
Hur J, Otegbeye E, Joh HK et al (2021) Sugar-sweetened beverage intake in adulthood and adolescence and risk of early-onset colorectal cancer among women. Gut 70:2330–2336. https://doi.org/10.1136/gutjnl-2020-323450
Sung H, Siegel RL, Rosenberg PS, Jemal A (2019) Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry. Lancet Public Health 4:e137–e147. https://doi.org/10.1016/s2468-2667(18)30267-6
Zhang X, Albanes D, Beeson WL et al (2010) Risk of colon cancer and coffee, tea, and sugar-sweetened soft drink intake: pooled analysis of prospective cohort studies. J Natl Cancer Inst 102:771–783. https://doi.org/10.1093/jnci/djq107
Mohammed A, Pacheco LS, Anderson CAM et al (2019) Sugar-sweetened beverages and colorectal cancer risk in the California Teachers Study. PLoS ONE. https://doi.org/10.1371/journal.pone.0223638
Zhong VW, Kuang A, Danning RD et al (2019) A genome-wide association study of bitter and sweet beverage consumption. Hum Mol Genet 28:2449–2457. https://doi.org/10.1093/hmg/ddz061
Luo J, Xu Z, Noordam R, van Heemst D, Li-Gao R (2021) Depression and inflammatory bowel disease: a bidirectional two-sample Mendelian randomization study. J Crohns Colitis. https://doi.org/10.1093/ecco-jcc/jjab191
Burgess S, Butterworth A, Thompson SJ (2013) Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 37:658–665. https://doi.org/10.1002/gepi.21758
Bowden J, Davey Smith G, Haycock P, Burgess SJ (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40:304–314. https://doi.org/10.1002/gepi.21965
Bowden J, Davey Smith G, Burgess SJI (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44:512–525. https://doi.org/10.1093/ije/dyv080
Verbanck M, Chen C, Neale B, Do RJ (2018) Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 50:693–698. https://doi.org/10.1038/s41588-018-0099-7
Hemani G, Tilling K, Davey Smith GJ (2017) Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLOS Genet 13:1007081. https://doi.org/10.1371/journal.pgen.1007081
Zhou B, Ichikawa R, Parnell LD et al (2020) Metabolomic links between sugar-sweetened beverage intake and obesity. J Obes 2020:7154738. https://doi.org/10.1155/2020/7154738
Bull CJ, Bell JA, Murphy N et al (2020) Adiposity, metabolites, and colorectal cancer risk: Mendelian randomization study. BMC Med 18:396. https://doi.org/10.1186/s12916-020-01855-9
Li H, Boakye D, Chen X et al (2021) Associations of body mass index at different ages with early-onset colorectal cancer. Gastroenterology. https://doi.org/10.1053/j.gastro.2021.12.239
Li H, Boakye D, Chen X, Hoffmeister M, Brenner HJT (2021) Association of body mass index with risk of early-onset colorectal cancer: systematic review and meta-analysis. Am J Gastroenterol. https://doi.org/10.14309/ajg.0000000000001393
Fulgoni V 3rd (2008) High-fructose corn syrup: everything you wanted to know, but were afraid to ask. Am J Clin Nutr 88:1715S. https://doi.org/10.3945/ajcn.2008.25825A
Goncalves M, Lu C, Tutnauer J et al (2019) High-fructose corn syrup enhances intestinal tumor growth in mice. Science 363:1345–1349. https://doi.org/10.1126/science.aat8515
Potter J, McMichael AJ (1986) Diet and cancer of the colon and rectum: a case-control study. J Natl Cancer Institut 76:557–569. https://doi.org/10.1093/jnci/76.4.557
Hwang LD, Lin C, Gharahkhani P et al (2019) New insight into human sweet taste: a genome-wide association study of the perception and intake of sweet substances. Am J Clin Nutr 109:1724–1737. https://doi.org/10.1093/ajcn/nqz043
Belloir C, Neiers F, Briand L (2017) Sweeteners and sweetness enhancers. Curr Opin Clin Nutr Metab Care 20:279–285. https://doi.org/10.1097/MCO.0000000000000377
Choudhary AK, Pretorius E (2017) Revisiting the safety of aspartame. Nutr Rev 75:718–730. https://doi.org/10.1093/nutrit/nux035
Ramne S, Brunkwall L, Ericson U et al (2021) Gut microbiota composition in relation to intake of added sugar, sugar-sweetened beverages and artificially sweetened beverages in the Malmo Offspring Study. Eur J Nutr 60:2087–2097. https://doi.org/10.1007/s00394-020-02392-0
Tilg H, Adolph TE, Gerner RR, Moschen AR (2018) The intestinal microbiota in colorectal cancer. Cancer Cell 33:954–964. https://doi.org/10.1016/j.ccell.2018.03.004
Chazelas E, Srour B, Desmetz E et al (2019) Sugary drink consumption and risk of cancer: results from NutriNet-Sante prospective cohort. BMJ 366:l2408. https://doi.org/10.1136/bmj.l2408
Zhang Y, Liu Z, Choudhury T, Cornelis MC, Liu W (2021) Habitual coffee intake and risk for nonalcoholic fatty liver disease: a two-sample Mendelian randomization study. Eur J Nutr 60:1761–1767. https://doi.org/10.1007/s00394-020-02369-z
Acknowledgements
The authors thank the professional editors of AJE Company (www.aje.cn) for editing the English of this manuscript.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
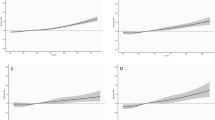
394_2022_2993_MOESM1_ESM.tif
Supplementary file1 Leave-one-out plot of MR analyses from SSB/sweet beverage intake to colorectal malignant neoplasm in each database (TIF 758 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, C., Zheng, S., Gao, H. et al. Causal relationship of sugar-sweetened and sweet beverages with colorectal cancer: a Mendelian randomization study. Eur J Nutr 62, 379–383 (2023). https://doi.org/10.1007/s00394-022-02993-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-022-02993-x