Abstract
Purpose
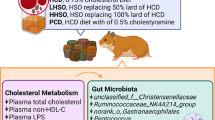
Peony (Paeonia spp.) seed oil (PSO) contains a high amount of α-linolenic acid. The effects of PSO on hypercholesterolemia and gut microbiota remains unclear. The present study was to investigate effects of PSO supplementation on cholesterol metabolism and modulation of the gut microbiota.
Methods
Male Golden Syrian hamsters (n = 40) were randomly divided into five groups (n = 8, each) fed one of the following diets namely low-cholesterol diet (LCD); high cholesterol diet (HCD); HCD with PSO substituting 50% lard (LPSO), PSO substituting 100% lard (HPSO) and HCD with addition of 0.5% cholestyramine (PCD), respectively, for 6 weeks.
Results
PSO supplementation dose-dependently reduced plasma total cholesterol (TC) by 9–14%, non-high-density lipoprotein cholesterol (non-HDL-C) by 7–18% and triacylglycerols (TG) by 14–34% (p < 0.05). In addition, feeding PSO diets reduced the formation of plaque lesions by 49–61% and hepatic lipids by 9–19% compared with feeding HCD diet (p < 0.01). PSO also altered relative genus abundance of unclassified_f__Coriobacteriaceae, unclassified_f__Erysipelotrichaceae, Peptococcus, unclassified_f__Ruminococcaceae, norank_o__Mollicutes_RF9 and Christensenellaceae_R-7_group.
Conclusions
It was concluded that PSO was effective in reducing plasma cholesterol and hepatic lipids and favorably modulating gut microbiota associated with cholesterol metabolism.
Graphical abstract











Similar content being viewed by others
References
Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3:e442. https://doi.org/10.1371/journal.pmed.0030442
Fuster V, Mearns BM (2009) The CVD paradox: mortality vs prevalence. Nat Rev Cardiol 6:669–669. https://doi.org/10.1038/nrcardio.2009.187
Mensah GA, Wei GS, Sorlie PD et al (2017) Decline in cardiovascular mortality: possible causes and implications. Circ Res 120:366–380. https://doi.org/10.1161/CIRCRESAHA.116.309115
Ford ES, Ajani UA, Croft JB et al (2007) Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med 356:2388–2398. https://doi.org/10.1056/NEJMsa053935
Ezzati M, Obermeyer Z, Tzoulaki I et al (2015) Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol 12:508–530. https://doi.org/10.1038/nrcardio.2015.82
Nelson RH (2013) Hyperlipidemia as a risk factor for cardiovascular disease. Prim Care 40:195–211. https://doi.org/10.1016/j.pop.2012.11.003
Law MR, Wald NJ, Thompson SG (1994) By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ 308:367–372. https://doi.org/10.1136/bmj.308.6925.367
Chen Z-Y, Ma KY, Liang Y et al (2011) Role and classification of cholesterol-lowering functional foods. J Funct Foods 3:61–69. https://doi.org/10.1016/j.jff.2011.02.003
Thursby E, Juge N (2017) Introduction to the human gut microbiota. Biochem J 474:1823–1836. https://doi.org/10.1042/BCJ20160510
David LA, Maurice CF, Carmody RN et al (2014) Diet rapidly and reproducibly alters the human gut microbiome. Nature 505:559–563. https://doi.org/10.1038/nature12820
Flint HJ, Scott KP, Louis P, Duncan SH (2012) The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol 9:577–589. https://doi.org/10.1038/nrgastro.2012.156
Mondot S, de Wouters T, Doré J, Lepage P (2013) The human gut microbiome and its dysfunctions. Dig Dis 31:278–285. https://doi.org/10.1159/000354678
Hooks KB, O’Malley MA (2017) Dysbiosis and its discontents. MBio. https://doi.org/10.1128/mBio.01492-17
Wilson TWH, Takeshi K, Hazen SL (2017) Gut microbiota in cardiovascular health and disease. Circ Res 120:1183–1196. https://doi.org/10.1161/CIRCRESAHA.117.309715
Marco W, Weeks TL, Hazen SL (2020) Gut microbiota and cardiovascular disease. Circ Res 127:553–570. https://doi.org/10.1161/CIRCRESAHA.120.316242
Hemarajata P, Versalovic J (2013) Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Ther Adv Gastroenterol 6:39–51. https://doi.org/10.1177/1756283X12459294
Vijay A, Astbury S, Le Roy C et al (2021) The prebiotic effects of omega-3 fatty acid supplementation: a six-week randomised intervention trial. Gut Microbes 13:1–11. https://doi.org/10.1080/19490976.2020.1863133
Costantini L, Molinari R, Farinon B, Merendino N (2017) Impact of omega-3 fatty acids on the gut microbiota. Int J Mol Sci 18:2645. https://doi.org/10.3390/ijms18122645
He C, Peng Y, Xiao W et al (2013) Determination of chemical variability of phenolic and monoterpene glycosides in the seeds of Paeonia species using HPLC and profiling analysis. Food Chem 138:2108–2114. https://doi.org/10.1016/j.foodchem.2012.11.049
Zhu W, Li X, Liu S et al (2010) Toxicological assessment of peony seed oil. Food Sci 31:248. https://doi.org/10.7506/spkx1002-6630-201011054
Yang X, Zhang D, Song L et al (2017) Chemical profile and antioxidant activity of the oil from Peony seeds (Paeonia suffruticosa Andr.). Oxid Med Cell Longev. https://doi.org/10.1155/2017/9164905
He D-Y, Dai S-M (2011) Anti-inflammatory and immunomodulatory effects of Paeonia lactiflora Pall., a traditional Chinese herbal medicine. Front Pharmacol. https://doi.org/10.3389/fphar.2011.00010
Sevim D, Senol FS, Gulpinar AR et al (2013) Discovery of potent in vitro neuroprotective effect of the seed extracts from seven Paeonia L. (peony) taxa and their fatty acid composition. Ind Crops Prod 49:240–246. https://doi.org/10.1016/j.indcrop.2013.05.001
Su J, Ma C, Liu C et al (2016) Hypolipidemic activity of peony seed oil rich in α-linolenic, is mediated through inhibition of lipogenesis and upregulation of fatty acid β-oxidation. J Food Sci 81:H1001-1009. https://doi.org/10.1111/1750-3841.13252
Zheng Z, Han J, Mao Y et al (2017) Health benefits of dietary tree peony seed oil in a high fat diet hamster model. Funct Foods Health Dis 7:135–148. https://doi.org/10.31989/ffhd.v7i2.313
Zhu H, Chen J, He Z et al (2019) Soybean germ oil reduces blood cholesterol by inhibiting cholesterol absorption and enhancing bile acid excretion. Food Funct 10:1836–1845. https://doi.org/10.1039/c8fo02585a
Si W, Liang Y, Ma KY et al (2012) Antioxidant activity of capsaicinoid in canola oil. J Agric Food Chem 60:6230–6234. https://doi.org/10.1021/jf301744q
Lei L, Chen J, Liu Y et al (2018) Dietary wheat bran oil is equally as effective as rice bran oil in reducing plasma cholesterol. J Agric Food Chem 66:2765–2774. https://doi.org/10.1021/acs.jafc.7b06093
Liu J, Hao W, He Z et al (2019) Beneficial effects of tea water extracts on the body weight and gut microbiota in C57BL/6J mice fed with a high-fat diet. Food Funct 10:2847–2860. https://doi.org/10.1039/C8FO02051E
Hao W, Zhu H, Chen J et al (2020) Wild melon seed oil reduces plasma cholesterol and modulates gut microbiota in hypercholesterolemic hamsters. J Agric Food Chem 68:2071–2081. https://doi.org/10.1021/acs.jafc.9b07302
Rafieian-Kopaei M, Setorki M, Doudi M et al (2014) Atherosclerosis: process, indicators, risk factors and new hopes. Int J Prev Med 5:927–946
Bertani B, Ruiz N (2018) Function and biogenesis of lipopolysaccharides. EcoSal Plus. https://doi.org/10.1128/ecosalplus.ESP-0001-2018.10.1128/ecosalplus.ESP-0001-2018
Janel N, Noll C (2014) Chapter 51—Protection and reversal of hepatic fibrosis by polyphenols. In: Watson RR, Preedy VR, Zibadi S (eds) Polyphenols in human health and disease. Academic Press, San Diego, pp 665–679
de la Cuesta-Zuluaga J, Mueller NT, Álvarez-Quintero R et al (2018) Higher fecal short-chain fatty acid levels are associated with gut microbiome dysbiosis, obesity, hypertension and cardiometabolic disease risk factors. Nutrients 11:E51. https://doi.org/10.3390/nu11010051
Ander BP, Dupasquier CM, Prociuk MA, Pierce GN (2003) Polyunsaturated fatty acids and their effects on cardiovascular disease. Exp Clin Cardiol 8:164–172
DeBose-Boyd RA (2008) Feedback regulation of cholesterol synthesis: sterol-accelerated ubiquitination and degradation of HMG CoA reductase. Cell Res 18:609–621. https://doi.org/10.1038/cr.2008.61
Edwards PA, Kast-Woelbern HR, Kennedy MA (2003) Chapter 170—Cholesterol signaling. In: Bradshaw RA, Dennis EA (eds) Handbook of cell signaling. Academic Press, Burlington, pp 287–290
Vogel C, Marcotte EM (2012) Insights into the regulation of protein abundance from proteomic and transcriptomic analyses. Nat Rev Genet 13:227–232. https://doi.org/10.1038/nrg3185
Maier T, Güell M, Serrano L (2009) Correlation of mRNA and protein in complex biological samples. FEBS Lett 583:3966–3973. https://doi.org/10.1016/j.febslet.2009.10.036
Danielsson H (1960) On the origin of the neutral fecal sterols and their relation to cholesterol metabolism in the rat: bile acids and steroids 92. Acta Physiol Scand 48:364–372. https://doi.org/10.1111/j.1748-1716.1960.tb01869.x
Afonso MS, Machado RM, Lavrador MS et al (2018) Molecular pathways underlying cholesterol homeostasis. Nutrients. https://doi.org/10.3390/nu10060760
Betters JL, Yu L (2010) NPC1L1 and cholesterol transport. FEBS Lett 584:2740–2747. https://doi.org/10.1016/j.febslet.2010.03.030
Iqbal J, Rudel LL, Hussain MM (2008) Microsomal triglyceride transfer protein enhances cellular cholesteryl esterification by relieving product inhibition*. J Biol Chem 283:19967–19980. https://doi.org/10.1074/jbc.M800398200
Nguyen TM, Sawyer JK, Kelley KL et al (2012) ACAT2 and ABCG5/G8 are both required for efficient cholesterol absorption in mice: evidence from thoracic lymph duct cannulation. J Lipid Res 53:1598–1609. https://doi.org/10.1194/jlr.M026823
Kazemian N, Mahmoudi M, Halperin F et al (2020) Gut microbiota and cardiovascular disease: opportunities and challenges. Microbiome 8:36. https://doi.org/10.1186/s40168-020-00821-0
Martínez I, Perdicaro DJ, Brown AW et al (2013) Diet-induced alterations of host cholesterol metabolism are likely to affect the gut microbiota composition in hamsters. Appl Environ Microbiol 79:516–524. https://doi.org/10.1128/AEM.03046-12
Claus SP, Ellero SL, Berger B et al (2011) Colonization-induced host-gut microbial metabolic interaction. MBio. https://doi.org/10.1128/mBio.00271-10
Martínez I, Wallace G, Zhang C et al (2009) Diet-induced metabolic improvements in a hamster model of hypercholesterolemia are strongly linked to alterations of the gut microbiota. Appl Environ Microbiol 75:4175–4184. https://doi.org/10.1128/AEM.00380-09
Spencer MD, Hamp TJ, Reid RW et al (2011) Association between composition of the human gastrointestinal microbiome and development of fatty liver with choline deficiency. Gastroenterology 140:976–986. https://doi.org/10.1053/j.gastro.2010.11.049
Kang Y, Li Y, Du Y et al (2019) Konjaku flour reduces obesity in mice by modulating the composition of the gut microbiota. Int J Obes 43:1631–1643. https://doi.org/10.1038/s41366-018-0187-x
Staley C, Weingarden AR, Khoruts A, Sadowsky MJ (2017) Interaction of gut microbiota with bile acid metabolism and its influence on disease states. Appl Microbiol Biotechnol 101:47–64. https://doi.org/10.1007/s00253-016-8006-6
Ryan PM, Stanton C, Caplice NM (2017) Bile acids at the cross-roads of gut microbiome–host cardiometabolic interactions. Diabetol Metab Syndr 9:102. https://doi.org/10.1186/s13098-017-0299-9
Wang B, Tontonoz P (2018) Liver X receptors in lipid signalling and membrane homeostasis. Nat Rev Endocrinol 14:452–463. https://doi.org/10.1038/s41574-018-0037-x
Jia W, Xie G, Jia W (2018) Bile acid–microbiota crosstalk in gastrointestinal inflammation and carcinogenesis. Nat Rev Gastroenterol Hepatol 15:111–128. https://doi.org/10.1038/nrgastro.2017.119
Alnouti Y (2009) Bile acid sulfation: a pathway of bile acid elimination and detoxification. Toxicol Sci 108:225–246. https://doi.org/10.1093/toxsci/kfn268
Gérard P (2013) Metabolism of cholesterol and bile acids by the gut microbiota. Pathogens 3:14–24. https://doi.org/10.3390/pathogens3010014
Woting A, Blaut M (2016) The intestinal microbiota in metabolic disease. Nutrients. https://doi.org/10.3390/nu8040202
Chang NW, Huang PC (1998) Effects of the ratio of polyunsaturated and monounsaturated fatty acid to saturated fatty acid on rat plasma and liver lipid concentrations. Lipids 33:481–487. https://doi.org/10.1007/s11745-998-0231-9
Hayes KC (2002) Dietary fat and heart health: in search of the ideal fat. Asia Pac J Clin Nutr 11:S394–S400. https://doi.org/10.1046/j.1440-6047.11.s.7.13.x
Mani V, Hollis JH, Gabler NK (2013) Dietary oil composition differentially modulates intestinal endotoxin transport and postprandial endotoxemia. Nutr Metab 10:6. https://doi.org/10.1186/1743-7075-10-6
Haro C, Garcia-Carpintero S, Alcala-Diaz JF et al (2016) The gut microbial community in metabolic syndrome patients is modified by diet. J Nutr Biochem 27:27–31. https://doi.org/10.1016/j.jnutbio.2015.08.011
Li H, Zhu Y, Zhao F et al (2017) Fish oil, lard and soybean oil differentially shape gut microbiota of middle-aged rats. Sci Rep 7:826. https://doi.org/10.1038/s41598-017-00969-0
Miyamoto J, Igarashi M, Watanabe K et al (2019) Gut microbiota confers host resistance to obesity by metabolizing dietary polyunsaturated fatty acids. Nat Commun 10:4007. https://doi.org/10.1038/s41467-019-11978-0
Tindall AM, McLimans CJ, Petersen KS et al (2020) Walnuts and vegetable oils containing oleic acid differentially affect the gut microbiota and associations with cardiovascular risk factors: follow-up of a randomized, controlled, feeding trial in adults at risk for cardiovascular disease. J Nutr 150:806–817. https://doi.org/10.1093/jn/nxz289
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest with regards to the content of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kwek, E., Zhu, H., Ding, H. et al. Peony seed oil decreases plasma cholesterol and favorably modulates gut microbiota in hypercholesterolemic hamsters. Eur J Nutr 61, 2341–2356 (2022). https://doi.org/10.1007/s00394-021-02785-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02785-9