Abstract
Purpose
Pomegranate peels are rich in anthocyanins. The present study aimed to explore the beneficial effects of pomegranate peel anthocyanins (PPA) on obesity and gut microbiota in mice with high-fat diet (HFD)-induced obesity.
Methods
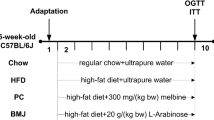
Specific pathogen-free (SPF) male C57BL/6 J mice were randomly divided into three groups and fed with low-fat diet (LFD, 10% fat energy), HFD (45% fat energy), or HFD supplemented with PPA by intragastric administration for 15 weeks. Body weight and food intake were monitored weekly. The obesity-related biochemical indexes and hepatic gene expression levels were determined. The compositions of the gut microbiota were analyzed by 16S rRNA sequencing, and the association between the gut microbiota and obesity-related indicators was investigated by Spearman correlation analysis.
Results
The results showed that the body weight gain, steatosis scores and insulin resistance index in the PPA group decreased by 27.46%, 56.25%, and 46.07%, respectively, compared to the HFD group. Gene expression analysis indicated that PPA supplement improved the genes expression profiles involved in glucose and lipid metabolism compared with the mice fed HFD alone. Meanwhile, PPA significantly changed the composition of the gut microbiota, which were closely correlated with the obesity-related biomarkers.
Conclusion
This study suggested that PPA could be a beneficial treatment option for alleviating HFD-induced obesity and related metabolic disorders by targeting microbiota and lipid metabolism.




Similar content being viewed by others
References
Despres JP, Lemieux I (2006) Abdominal obesity and metabolic syndrome. Nature 444(7121):881–887. https://doi.org/10.1038/nature05488
Authors N (2013) Obesity and food science being part of the solution. J Food Sci. https://doi.org/10.1111/1750-3841.12261
Yun JW (2010) Possible anti-obesity therapeutics from nature—a review. Phytochemistry 71(14–15):1625–1641. https://doi.org/10.1016/j.phytochem.2010.07.011
Powell TM, Khera A (2010) Therapeutic approaches to obesity. Curr Treat Options Cardiovasc Med 12(4):381–395. https://doi.org/10.1007/s11936-010-0080-y
Wang Q, Jiao L, He C, Sun H, Cai Q, Han T, Hu H (2017) Alteration of gut microbiota in association with cholesterol gallstone formation in mice. BMC Gastroenterol 17(1):74. https://doi.org/10.1186/s12876-017-0629-2
Canfora EE, Meex RCR, Venema K, Blaak EE (2019) Gut microbial metabolites in obesity, NAFLD and T2DM. Nat Rev Endocrinol 15(5):261–273. https://doi.org/10.1038/s41574-019-0156-z
Qiu X, Macchietto MG, Liu X, Lu Y, Ma Y, Guo H, Saqui-Salces M, Bernlohr DA, Chen C, Shen S, Chen X (2021) Identification of gut microbiota and microbial metabolites regulated by an antimicrobial peptide lipocalin 2 in high fat diet-induced obesity. Int J Obesity 45(1):143–154. https://doi.org/10.1038/s41366-020-00712-2
Crovesy L, Masterson D, Rosado EL (2020) Profile of the gut microbiota of adults with obesity: a systematic review. Eur J Clin Nutr 74(9):1251–1262. https://doi.org/10.1038/s41430-020-0607-6
Delzenne NM, Rodriguez J, Olivares M, Neyrinck AM (2020) Microbiome response to diet: focus on obesity and related diseases. Rev Endocr Metab Dis 21(3):369–380. https://doi.org/10.1007/s11154-020-09572-7
Hou D, Zhao Q, Yousaf L, Xue Y, Shen Q (2021) Beneficial effects of mung bean seed coat on the prevention of high-fat diet-induced obesity and the modulation of gut microbiota in mice. Eur J Nutr 60(4):2029–2045. https://doi.org/10.1007/s00394-020-02395-x
Chen J, He X, Huang J (2014) Diet effects in gut microbiome and obesity. J Food Sci 79(4):R442-451. https://doi.org/10.1111/1750-3841.12397
Sonnenburg JL, Bäckhed F (2016) Diet–microbiota interactions as moderators of human metabolism. Nature 535(7610):56–64. https://doi.org/10.1038/nature18846
Portune KJ, Benítez-Páez A, Del Pulgar EMG, Cerrudo V, Sanz Y (2017) Gut microbiota, diet, and obesity-related disorders—the good, the bad, and the future challenges. Mol Nutri Food Res 61(1):1600252. https://doi.org/10.1002/mnfr.201600252
Fu C, Jiang Y, Guo J, Su Z (2016) Natural products with anti-obesity effects and different mechanisms of action. J Agric Food Chem 64(51):9571–9585. https://doi.org/10.1021/acs.jafc.6b04468
Salehi B, Sharifi-Rad J, Cappellini F, Reiner Z, Zorzan D, Imran M, Sener B, Kilic M, El-Shazly M, Fahmy NM, Al-Sayed E, Martorell M, Tonelli C, Petroni K, Docea AO, Calina D, Maroyi A (2020) The therapeutic potential of anthocyanins: current approaches based on their molecular mechanism of action. Front Pharmacol 11:1300. https://doi.org/10.3389/fphar.2020.01300
Johanningsmeier SD, Harris GK (2011) Pomegranate as a functional food and nutraceutical source. Annu Rev Food Sci Technol 2(1):181–201. https://doi.org/10.1146/annurev-food-030810-153709
Magangana TP, Makunga NP, Fawole OA, Opara UL (2020) Processing factors affecting the phytochemical and nutritional properties of pomegranate (Punica granatum L.) peel waste: a review. Molecules 25(20):4690
Huang TH-W, Peng G, Kota BP, Li GQ, Yamahara J, Roufogalis BD, Li Y (2005) Pomegranate flower improves cardiac lipid metabolism in a diabetic rat model: role of lowering circulating lipids. Br J Pharmacol 145(6):767–774. https://doi.org/10.1038/sj.bjp.0706245
Lei F, Zhang XN, Wang W, Xing DM, Xie WD, Su H, Du LJ (2007) Evidence of anti-obesity effects of the pomegranate leaf extract in high-fat diet induced obese mice. Int J Obes 31(6):1023–1029. https://doi.org/10.1038/sj.ijo.0803502
Raffaele M, Licari M, Amin S, Alex R, Shen H-h, Singh SP, Vanella L, Rezzani R, Bonomini F, Peterson SJ, Stec DE, Abraham NG (2020) Cold press pomegranate seed oil attenuates dietary-obesity induced hepatic steatosis and fibrosis through antioxidant and mitochondrial pathways in obese mice. Int J Mol Sci 21(15):5469
Zhao R, Long X, Yang J, Du L, Zhang X, Li J, Hou C (2019) Pomegranate peel polyphenols reduce chronic low-grade inflammatory responses by modulating gut microbiota and decreasing colonic tissue damage in rats fed a high-fat diet. Food Funct 10(12):8273–8285. https://doi.org/10.1039/C9FO02077B
Song H, Chu Q, Xu D, Xu Y, Zheng X (2016) Purified betacyanins from hylocereus undatus peel ameliorate obesity and insulin resistance in high-fat-diet-fed mice. J Agric Food Chem 64(1):236–244. https://doi.org/10.1021/acs.jafc.5b05177
Folch J, Lees M, Stanley GHS (1957) A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem 226(1):497–509. https://doi.org/10.1016/S0021-9258(18)64849-5
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(–Delta Delta C(T)) method. Methods 25(4):402–408. https://doi.org/10.1006/meth.2001.1262
Basu A, Penugonda K (2009) Pomegranate juice: a heart-healthy fruit juice. Nutr Rev 67(1):49–56. https://doi.org/10.1111/j.1753-4887.2008.00133.x
Panichayupakaranant P, Tewtrakul S, Yuenyongsawad S (2010) Antibacterial, anti-inflammatory and anti-allergic activities of standardised pomegranate rind extract. Food Chem 123:400–403. https://doi.org/10.1016/j.foodchem.2010.04.054
Fischer UA, Carle R, Kammerer DR (2011) Identification and quantification of phenolic compounds from pomegranate (Punica granatum L.) peel, mesocarp, aril and differently produced juices by HPLC-DAD–ESI/MSn. Food Chem 127(2):807–821. https://doi.org/10.1016/j.foodchem.2010.12.156
El-Sayyad HIH (2015) Cholesterol overload impairing cerebellar function: the promise of natural products. Nutrition 31(5):621–630. https://doi.org/10.1016/j.nut.2014.10.017
Spilmont M, Léotoing L, Davicco M-J, Lebecque P, Mercier S, Miot-Noirault E, Pilet P, Rios L, Wittrant Y, Coxam V (2014) Pomegranate and its derivatives can improve bone health through decreased inflammation and oxidative stress in an animal model of postmenopausal osteoporosis. Eur J Nutr 53(5):1155–1164. https://doi.org/10.1007/s00394-013-0615-6
Esmaillzadeh A, Tahbaz F, Gaieni I, Alavi-Majd H, Azadbakht L (2004) Concentrated pomegranate juice improves lipid profiles in diabetic patients with hyperlipidemia. J Med Food 7(3):305–308. https://doi.org/10.1089/jmf.2004.7.305
Esmaillzadeh A, Tahbaz F, Gaieni I, Alavi-Majd H, Azadbakht L (2006) Cholesterol-lowering effect of concentrated pomegranate juice consumption in type II diabetic patients with hyperlipidemia. Int J Vitam Nutr Res 76(3):147–151. https://doi.org/10.1024/0300-9831.76.3.147
Xi Y, Li H (2020) Role of farnesoid X receptor in hepatic steatosis in nonalcoholic fatty liver disease. Biomed Pharmacother 121:109609. https://doi.org/10.1016/j.biopha.2019.109609
Longato L, Tong M, Wands JR, de la Monte SM (2012) High fat diet induced hepatic steatosis and insulin resistance: role of dysregulated ceramide metabolism. Hepatol Res 42(4):412–427. https://doi.org/10.1111/j.1872-034X.2011.00934.x
Garcia-Serrano AM, Duarte JMN (2020) Brain metabolism alterations in type 2 diabetes: what did we learn from diet-induced diabetes models? Front Neurosci. https://doi.org/10.3389/fnins.2020.00229
Harzallah A, Hammami M, Kępczyńska MA, Hislop DC, Arch JRS, Cawthorne MA, Zaibi MS (2016) Comparison of potential preventive effects of pomegranate flower, peel and seed oil on insulin resistance and inflammation in high-fat and high-sucrose diet-induced obesity mice model. Arch Physiol Biochem 122(2):75–87. https://doi.org/10.3109/13813455.2016.1148053
Esmaeilinezhad Z, Babajafari S, Sohrabi Z, Eskandari MH, Amooee S, Barati-Boldaji R (2019) Effect of synbiotic pomegranate juice on glycemic, sex hormone profile and anthropometric indices in PCOS: a randomized, triple blind, controlled trial. Nutr Metab Cardiovasc Dis 29(2):201–208. https://doi.org/10.1016/j.numecd.2018.07.002
Huang H, Liao D, Chen G, Chen H, Zhu Y (2017) Lack of efficacy of pomegranate supplementation for glucose management, insulin levels and sensitivity: evidence from a systematic review and meta-analysis. Nutr J 16(1):67. https://doi.org/10.1186/s12937-017-0290-1
Ilyas Z, Perna S, Al-Thawadi S, Alalwan TA, Riva A, Petrangolini G, Gasparri C, Infantino V, Peroni G, Rondanelli M (2020) The effect of Berberine on weight loss in order to prevent obesity: a systematic review. Biomed Pharmacother 127:110137. https://doi.org/10.1016/j.biopha.2020.110137
Gautier-Stein A, Soty M, Chilloux J, Zitoun C, Rajas F, Mithieux G (2012) Glucotoxicity induces glucose-6-phosphatase catalytic unit expression by acting on the interaction of HIF-1α with CREB-binding protein. Diabetes 61(10):2451. https://doi.org/10.2337/db11-0986
Krause C, Geißler C, Tackenberg H, El Gammal AT, Wolter S, Spranger J, Mann O, Lehnert H, Kirchner H (2020) Multi-layered epigenetic regulation of IRS2 expression in the liver of obese individuals with type 2 diabetes. Diabetologia 63(10):2182–2193. https://doi.org/10.1007/s00125-020-05212-6
Illiano P, Brambilla R, Parolini C (2020) The mutual interplay of gut microbiota, diet and human disease. FEBS J 287(5):833–855. https://doi.org/10.1111/febs.15217
Fang J (2014) Bioavailability of anthocyanins. Drug Metab Rev 46(4):508–520. https://doi.org/10.3109/03602532.2014.978080
Hidalgo M, Oruna-Concha MJ, Kolida S, Walton GE, Kallithraka S, Spencer JPE, Gibson GR, de Pascual-Teresa S (2012) Metabolism of anthocyanins by human gut microflora and their influence on gut bacterial growth. J Agr Food Chem 60(15):3882–3890. https://doi.org/10.1021/jf3002153
Singer-Englar T, Barlow G, Mathur R (2019) Obesity, diabetes, and the gut microbiome: an updated review. Expert Rev Gastroenterol Hepatol 13(1):3–15. https://doi.org/10.1080/17474124.2019.1543023
Shin NR, Whon TW, Bae JW (2015) Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trends Biotechnol 33(9):496–503. https://doi.org/10.1016/j.tibtech.2015.06.011
Zhou K (2017) Strategies to promote abundance of Akkermansia muciniphila, an emerging probiotics in the gut, evidence from dietary intervention studies. J Funct Foods 33:194–201. https://doi.org/10.1016/j.jff.2017.03.045
Li Z, Henning SM, Lee RP, Lu QY, Summanen PH, Thames G, Corbett K, Downes J, Tseng CH, Finegold SM, Heber D (2015) Pomegranate extract induces ellagitannin metabolite formation and changes stool microbiota in healthy volunteers. Food Funct 6(8):2487–2495. https://doi.org/10.1039/c5fo00669d
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto JM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490(7418):55–60. https://doi.org/10.1038/nature11450
Louis S, Tappu RM, Damms-Machado A, Huson DH, Bischoff SC (2016) Characterization of the gut microbial community of obese patients following a weight-loss intervention using whole metagenome shotgun sequencing. PLoS One 11(2):e0149564. https://doi.org/10.1371/journal.pone.0149564
Zeng Q, Li D, He Y, Li Y, Yang Z, Zhao X, Liu Y, Wang Y, Sun J, Feng X, Wang F, Chen J, Zheng Y, Yang Y, Sun X, Xu X, Wang D, Kenney T, Jiang Y, Gu H, Li Y, Zhou K, Li S, Dai W (2019) Discrepant gut microbiota markers for the classification of obesity-related metabolic abnormalities. Sci Rep 9(1):13424. https://doi.org/10.1038/s41598-019-49462-w
Oddi S, Huber P, Rocha Faria Duque AL, Vinderola G, Sivieri K (2020) Breast-milk derived potential probiotics as strategy for the management of childhood obesity. Food Res Int 137:109673. https://doi.org/10.1016/j.foodres.2020.109673
Acknowledgements
This study was supported by the National Natural Science Foundation of China (32072221, 31701031) and China Postdoctoral Science Foundation (2016M601006).
Author information
Authors and Affiliations
Contributions
HS: designed the research, analyzed the data, and wrote the paper; XS: analyzed the data and wrote the paper; RD, QC: conducted the experiments and collected the data; XZ: provided essential materials and reviewed the manuscript; and all authors: read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared no conflict of interest.
Ethical approval
Compliance with ethical standards.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Song, H., Shen, X., Deng, R. et al. Pomegranate peel anthocyanins prevent diet-induced obesity and insulin resistance in association with modulation of the gut microbiota in mice. Eur J Nutr 61, 1837–1847 (2022). https://doi.org/10.1007/s00394-021-02771-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02771-1