Abstract
Purpose
Despite longstanding voluntary salt iodisation in Switzerland, data suggest inadequate iodine intake in vulnerable population groups. In response, the salt iodine concentration was increased from 20 to 25 mg/kg and we assessed the impact on iodine status.
Methods
We conducted a cross-sectional national study in school-age children (n = 731), women of reproductive age (n = 353) and pregnant women (n = 363). We measured urinary iodine concentration (UIC) and urinary sodium concentration (UNaC) in spot urine samples. The current median UIC was compared with national data from 1999, 2004 and 2009. We measured TSH, total T4 and thyroglobulin (Tg) on dried blood spot samples collected in women.
Results
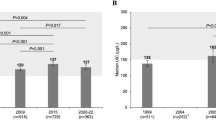
The median UIC (bootstrapped 95% CI) was 137 µg/L (131, 143 µg/L) in school children, 88 µg/L (72, 103 µg/L) in women of reproductive age and 140 µg/L (124, 159 µg/L) in pregnant women. Compared to 2009, the median UIC increased modestly in school children (P < 0.001), but did not significantly change in pregnant women (P = 0.417). Estimated sodium intake exceeded the recommendations in all population groups. The prevalence of thyroid disorders in women was low, but Tg was elevated in 13% of the pregnant women.
Conclusion
Iodine intake is overall adequate in Swiss school-age children, but only borderline sufficient in pregnant and non-pregnant women, despite high salt intakes and satisfactory household coverage with iodized salt. Our findings suggest increasing the concentration of iodine in salt may not improve iodine intakes in women if iodised salt is not widely used in processed foods.
Registration
This trial was registered at clinicaltrials.gov as NCT02312466.


Similar content being viewed by others
Abbreviations
- DBS:
-
Dried blood spot
- EAR:
-
Estimated average requirement
- Tg:
-
Thyroglobulin
- TSH:
-
Thyroid stimulating hormone
- TT4:
-
Total thyroxine
- UCC:
-
Urinary creatinine concentration
- UIC:
-
Urinary iodine concentration
- UIE:
-
Urinary iodine excretion
- UNaC:
-
Urinary sodium concentration
- UL:
-
Upper level
References
WHO, UNICEF, ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers, 3rd edn. World Health Organization, Geneva
Aburto N, Abudou M, Candeias V, Wu T (2014) Effect and safety of salt iodization to prevent iodine deficiency disorders: a systematic review with meta-analyses. WHO eLibrary of Evidence for Nutrition Actions (eLENA). World Health Organization, Geneva
Dold S, Zimmermann MB, Jukic T, Kusic Z, Jia Q, Sang Z, Quirino A, San Luis TOL, Fingerhut R, Kupka R, Timmer A, Garrett GG, Andersson M (2018) Universal salt iodization provides sufficient dietary iodine to achieve adequate iodine nutrition during the first 1000 days: a cross-sectional multicenter study. J Nutr 148(4):587–598
Bürgi H, Supersaxo Z, Selz B (1990) Iodine deficiency diseases in Switzerland one hundred years after Theodor Kocher’s survey: a historical review with some new goitre prevalence data. Acta Endocrinol (Copenh) 123(6):577–590
Zimmermann MB (2008) Research on iodine deficiency and goiter in the 19th and early 20th centuries. J Nutr 138(11):2060–2063
Bürgi H, Andersson M (2013) History and current epidemiology of iodine nutrition in Switzerland. In: Federal Commission for Nutrition. Iodine supply in Switzerland: current status and recommendations. Expert report of the FCN. Federal Office of Public Health, Zurich. https://www.eek.admin.ch/eek/en/home/pub/jodversorgung-in-der-schweiz-.html. Accessed 9 Oct 2018
Hess SY, Zimmermann MB, Torresani T, Burgi H, Hurrell RF (2001) Monitoring the adequacy of salt iodization in Switzerland: a national study of school children and pregnant women. Eur J Clin Nutr 55(3):162–166
EDI (2018) Verordnung des EDI über den Zusatz von Vitaminen, Mineralstoffen und sonstigen Stoffen. In: Lebensmitteln (817.022.32) (in German), vom 16. Dezember 2016 (Stand am 6. Februar 2018). Eidgenössisches Department des Innern (EDI) (Federal Department of Home Affairs), Bern
Zimmermann MB, Aeberli I, Torresani T, Burgi H (2005) Increasing the iodine concentration in the Swiss iodized salt program markedly improved iodine status in pregnant women and children: a 5-y prospective national study. Am J Clin Nutr 82(2):388–392
Andersson M, Aeberli I, Wust N, Piacenza AM, Bucher T, Henschen I, Haldimann M, Zimmermann MB (2010) The Swiss iodized salt program provides adequate iodine for school children and pregnant women, but weaning infants not receiving iodine-containing complementary foods as well as their mothers are iodine deficient. J Clin Endocrinol Metab 95(12):5217–5224
Zimmermann MB, Andersson M (2012) Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev 70(10):553–570
Haldimann M, Bochud M, Burnier M, Paccaud F, Dudler V (2015) Prevalence of iodine inadequacy in Switzerland assessed by the estimated average requirement cut-point method in relation to the impact of iodized salt. Public Health Nutr 18(8):1333–1342
Dorey CM, Zimmermann MB (2008) Reference values for spot urinary iodine concentrations in iodine-sufficient newborns using a new pad collection method. Thyroid 18(3):347–352
Gizak M, Gorstein J, Andersson M (2017) Epidemiology of iodine deficiency. In: Pearce E (ed) Iodine deficiency disorders and their eradication. Springer, New York, pp 29–43
IGN (2017) Global scorecard of iodine nutrition in 2017 in the general population and in pregnant women. Iodine Global Network. http://www.ign.org/cm_data/IGN_Global_Scorecard_AllPop_and_PW_May2017.pdf. Accessed 24 Aug 2018
Zimmermann MB, Gizak M, Abbott K, Andersson M, Lazarus JH (2015) Iodine deficiency in pregnant women in Europe. Lancet Diabetes Endocrinol 3(9):672–674
Hess SY, Zimmermann MB (2000) Thyroid volumes in a national sample of iodine-sufficient swiss school children: comparison with the World Health Organization/International Council for the control of iodine deficiency disorders normative thyroid volume criteria. Eur J Endocrinol 142(6):599–603
Fraser CG, Harris EK (1989) Generation and application of data on biological variation in clinical-chemistry. Crit Rev Cl Lab Sci 27(5):409–437
König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB (2011) Ten repeat collections for urinary iodine from spot samples or 24-h samples are needed to reliably estimate individual iodine status in women. J Nutr 141(11):2049–2054
WHO (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO expert committee. World Health Organization, Geneva
Pino S, Fang SL, Braverman LE (1998) Ammonium persulfate: a new and safe method for measuring urinary iodine by ammonium persulfate oxidation. Exp Clin Endocrinol Diabetes 106(Suppl 3):S22–S27
Vasiliades J (1976) Reaction of alkaline sodium picrate with creatinine: I. Kinetics and mechanism of formation of the mono-creatinine picric acid complex. Clin Chem 22(10):1664–1671
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, Grobman WA, Laurberg P, Lazarus JH, Mandel SJ, Peeters RP, Sullivan S (2017) 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27(3):315–389
Weeke J, Dybkjaer L, Granlie K, Jensen SE, Kjaerulff E, Laurberg P, Magnusson B (1982) A longitudinal study of serum TSH, and total and free iodothyronines during normal pregnancy. Acta Endocrinol (Copenh) 101(4):531–537
Stinca S, Andersson M, Erhardt J, Zimmermann MB (2015) Development and validation of a new low-cost enzyme-linked immunoassay for serum and dried blood spot thyroglobulin. Thyroid 25(12):1297–1305
Zimmermann MB, de Benoist B, Corigliano S, Jooste PL, Molinari L, Moosa K, Pretell EA, Al-Dallal ZS, Wei Y, Zu-Pei C, Torresani T (2006) Assessment of iodine status using dried blood spot thyroglobulin: development of reference material and establishment of an international reference range in iodine-sufficient children. J Clin Endocrinol Metab 91(12):4881–4887
Stinca S, Andersson M, Weibel S, Herter-Aeberli I, Fingerhut R, Gowachirapant S, Hess SY, Jaiswal N, Jukic T, Kusic Z, Mabapa NS, Nepal AK, San Luis TO, Zhen JQ, Zimmermann MB (2017) Dried blood spot thyroglobulin as a biomarker of iodine status in pregnant women. J Clin Endocrinol Metab 102(1):23–32
Montenegro-Bethancourt G, Johner SA, Stehle P, Neubert A, Remer T (2015) Iodine status assessment in children: Spot urine iodine concentration reasonably reflects true twenty-four-hour iodine excretion only when scaled to creatinine. Thyroid 25(6):688–697
Remer T, Neubert A, Maser-Gluth C (2002) Anthropometry-based reference values for 24-h urinary creatinine excretion during growth and their use in endocrine and nutritional research. Am J Clin Nutr 75(3):561–569
Kesteloot H, Joossens JV (1996) On the determinants of the creatinine clearance: a population study. J Hum Hypertens 10(4):245–249
Jahreis G, Hausmann W, Kiessling G, Franke K, Leiterer M (2001) Bioavailability of iodine from normal diets rich in dairy products–results of balance studies in women. Exp Clin Endocrinol Diabetes 109(3):163–167
Food, Board N, Institute of Medicine (2001) Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium and zinc. National Academy Press, Washington DC
Carriquiry AL (1999) Assessing the prevalence of nutrient inadequacy. Public Health Nutr 2(1):23–33
Food, Board N, Institute of Medicine (2000) Dietary reference intakes: applications in dietary assessment. National Academy Press, Washington DC
Dodd KW (1996) A User’s guide to C-SIDE: software for intake distribution estimation version 1.0. CARD Technical Report 96–TR31. Ames (IA): Center for Agricultural and Rural Development, Iowa State University
Dodd KW (1996) A technical guide to C-SIDE. Dietary assessment research series report 9. CARD technical report 96-TR32. Ames (IA): Center for Agricultural and Rural Development, Iowa State University
Guenther PM, Kott PS, Carriquiry AL (1997) Development of an approach for estimating usual nutrient intake distributions at the population level. J Nutr 127(6):1106–1112
Pearce EN, Lazarus JH, Smyth PP, He X, Smith DF, Pino S, Braverman LE (2009) Urine test strips as a source of iodine contamination. Thyroid 19(8):919
World Health Organization, United Nations Children’s Fund, International Council for the Control of Iodine Deficiency Disorders (2007) Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers, 3rd edn. World Health Organization, Geneva
Delange F, Benker G, Caron P, Eber O, Ott W, Peter F, Podoba J, Simescu M, Szybinsky Z, Vertongen F, Vitti P, Wiersinga W, Zamrazil V (1997) Thyroid volume and urinary iodine in European schoolchildren: standardization of values for assessment of iodine deficiency. Eur J Endocrinol 136(2):180–187
Ascoli W, Arroyave G (1970) Epidemiologia el bocio ende´mico en Centro Ame´rica. Relacio´n entre prevalencia y excrecio´n urinaria de yodo (Epidemiology of endemic goiter in Central America. Association between prevalence and urinary iodine excretion). Archives of Latinoamer Nutrition 20:309–320
Langer P (1980) Eastern and southeastern Europe. In: Stanbury JB, Hetzel BS (eds) Endemic goiter and endemic cretinism. Wiley, New York, pp 141–153
Brown IJ, Tzoulaki I, Candeias V, Elliott P (2009) Salt intakes around the world: implications for public health. Int J Epidemiol 38(3):791–813
The EUthyroid Consortium (2018) The Krakow declaration on iodine. Tasks and responsibilities for prevention programs targeting iodine deficiency disorders. Eur Thyroid J 7(4):201–204
Strohm D, Bechthold A, Ellinger S, Leschik-Bonnet E, Stehle P, Heseker H, German Nutr Soc DGE (2018) Revised reference values for the intake of sodium and chloride. Ann Nutr Metab 72(1):12–17
WHO (2012) Guideline: sodium intake for adults and children. World Health Organization, Geneva
Chappuis A, Bochud M, Glatz N, Vuistiner P, Paccaud F, Burnier M (2011) Swiss survey on salt intake: main results. Centre Hospitalier Universitaire Vaudois (CHUV), Lausanne, Suisse, Lausanne
Rios-Leyvraz M, Bovet P, Bochud M, Genin B, Russo M, Rossier MF, Tabin R, Chiolero A (2018) Estimation of salt intake and excretion in children in one region of Switzerland: a cross-sectional study. Eur J Nutr. https://doi.org/10.1007/s00394-018-1845-4
Federal Department of Home Affairs (2017) Swiss nutrition policy 2017–2024. Federal Food Safety and Veterinary Office, Bern
WHO (2014) Salt reduction and iodine fortification strategies in public health: Report of a joint technical meeting. World Health Organization, Geneva
Webster J, Land MA, Christoforou A, Eastman CJ, Zimmerman M, Campbell NR, Neal BC (2014) Reducing dietary salt intake and preventing iodine deficiency: towards a common public health agenda. Med J Aust 201(9):507–508
van der Reijden OL, Zimmermann MB, Galetti V (2017) Iodine in dairy milk: Sources, concentrations and importance to human health. Best Pract Res Clin Endocrinol Metab 31(4):385–395
van der Reijden OL, Galetti V, Hulmann M, Krzystek A, Haldimann M, Schlegel P, Manzocchi E, Berard J, Kreuzer M, Zimmermann MB, Herter-Aeberli I (2018) The main determinants of iodine in cows’ milk in Switzerland are farm type, season and teat dipping. Br J Nutr 119(5):559–569
Schupbach R, Wegmuller R, Berguerand C, Bui M, Herter-Aeberli I (2017) Micronutrient status and intake in omnivores, vegetarians and vegans in Switzerland. Eur J Nutr 56(1):283–293
Zimmermann MB, Aeberli I, Andersson M, Assey V, Yorg JA, Jooste P, Jukic T, Kartono D, Kusic Z, Pretell E, San Luis TO Jr, Untoro J, Timmer A (2013) Thyroglobulin is a sensitive measure of both deficient and excess iodine intakes in children and indicates no adverse effects on thyroid function in the UIC range of 100–299 mug/L: a UNICEF/ICCIDD study group report. J Clin Endocrinol Metab 98(3):1271–1280
Ma ZF, Skeaff SA (2014) Thyroglobulin as a biomarker of iodine deficiency: a review. Thyroid 24(8):1195–1209
Laurberg P, Cerqueira C, Ovesen L, Rasmussen LB, Perrild H, Andersen S, Pedersen IB, Carle A (2010) Iodine intake as a determinant of thyroid disorders in populations. Best Pract Res Clin Endocrinol Metab 24(1):13–27
Zimmermann MB, Boelaert K (2015) Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 3(4):286–295
De Leo S, Lee SY, Braverman LE (2016) Hyperthyroidism Lancet 388(10047):906–918
Baltisberger BL, Minder CE, Burgi H (1995) Decrease of incidence of toxic nodular goitre in a region of Switzerland after full correction of mild iodine deficiency. Eur J Endocrinol 132(5):546–549
Petersen M, Knudsen N, Carle A, Andersen S, Jorgensen T, Perrild H, Ovesen L, Rasmussen LB, Thuesen BH, Pedersen IB (2018) Thyrotoxicosis after iodine fortification. A 21-year Danish population-based study. Clin Endocrinol (Oxf) 89(3):360–366
Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, Okosieme OE (2018) Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol 14(5):301–316
Burgi H, Kohler M, Morselli B (1998) Thyrotoxicosis incidence in Switzerland and benefit of improved iodine supply. Lancet 352(9133):1034
Pedersen IB, Knudsen N, Carle A, Vejbjerg P, Jorgensen T, Perrild H, Ovesen L, Rasmussen LB, Laurberg P (2011) A cautious iodization programme bringing iodine intake to a low recommended level is associated with an increase in the prevalence of thyroid autoantibodies in the population. Clin Endocrinol (Oxf) 75(1):120–126
Petersen M, Knudsen N, Carle A, Andersen S, Jorgensen T, Perrild H, Ovesen L, Rasmussen LB, Thuesen BH, Pedersen IB (2018) Increased incidence rate of hypothyroidism after iodine fortification in Denmark. A 20 year prospective population-based study. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2018-01993
Farebrother J, Zimmermann MB, Andersson M (2019) Excessive iodine intake: sources, assessment and effects on thyroid function. Ann NY Acad Sci. https://doi.org/10.1111/nyas.14041
National Health and Medical Research Council (NHMRC) (2010) Iodine supplementation for pregnant and breastfeeding women. In: NHMRC Public Statement, January 2010
Lazarus J, Brown RS, Daumerie C, Hubalewska-Dydejczyk A, Negro R, Vaidya B (2014) 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J 3(2):76–94
Andersson M, de Benoist B, Delange F, Zupan J (2007) Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr 10(12A):1606–1611
Lee SY, Stagnaro-Green A, MacKay D, Wong AW, Pearce EN (2017) Iodine contents in prenatal vitamins in the United States. Thyroid 27(8):1101–1102
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB (2016) Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr 104(Suppl 3):918S–923S
Harding KB, Peña-Rosas JP, Webster AC, Yap CMY, Payne BA, Ota E, De-Regil LM (2017) Iodine supplementation for women during the preconception, pregnancy and postpartum period. Cochrane Database Systematic Rev 3:CD011761
Gowachirapant S, Jaiswal N, Melse-Boonstra A, Galetti V, Stinca S, Mackenzie I, Thomas S, Thomas T, Winichagoon P, Srinivasan K, Zimmermann MB (2017) Effect of iodine supplementation in pregnant women on child neurodevelopment: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 5(11):853–863
Acknowledgements
The study was funded by the Federal Food Safety and Veterinary Office (FSVO), Bern, Switzerland, and ETH Zurich, Zurich, Switzerland. We would like to thank the subjects for their participation and, teachers, doctors and nurses for assistance with subject recruitment and sample collection. We thank ETH students Leonie Arns, Friederike Becker, Matthias Buchli, Simon Hartung, Lisa Mazzolini, Laura Salvioni, Elisabeth Schlunke, Sara Stinca, Alexandra Thoma and Lea Wildeisen for assistance with the study and support with laboratory analysis. We also thank Leonie Arns for conducting the statistical analysis of the prevalence of inadequate iodine intake and Stefan Trachsel for providing salt sales data from the Swiss Saltworks AG.
Author information
Authors and Affiliations
Contributions
The author’s responsibilities were as follows—MA, IHA, MBZ: designed the research and wrote the study protocol; MA, IHA: supervised the study; SH: assisted with study coordination and conducted biochemical analysis of TSH, TT4 and Tg; RF: supervised the measurement of TSH and TT4; MA: conducted the statistical analysis and wrote the paper. MA had primary responsibility for final content. All authors read, edited, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest statement.
Rights and permissions
About this article
Cite this article
Andersson, M., Hunziker, S., Fingerhut, R. et al. Effectiveness of increased salt iodine concentration on iodine status: trend analysis of cross-sectional national studies in Switzerland. Eur J Nutr 59, 581–593 (2020). https://doi.org/10.1007/s00394-019-01927-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-019-01927-4