Abstract
Purposes
To compare the risk of anastomotic leak (AL) between Ethicon manual circular staplers (two-row) versus Medtronic EEA™ circular stapler with Tri-Staple™ technology (three-row) and between Medtronic EEA™ circular stapler with DST™ Series technology (two-row) versus Tri-Staple™ technology.
Methods
A retrospective cohort study was conducted in adult patients who underwent a left-sided colorectal surgery 2019–2022 in U.S. Premier Healthcare Database to assess the risk of AL within 30 days post-index procedure. The study devices were Ethicon manual circular staplers, Medtronic EEA™ circular stapler with DST™ technology, and Medtronic EEA™ circular stapler with Tri-Staple™ technology.
Results
Across 447 hospitals, the cumulative incidences (95% confidence intervals [CI]) of AL within 30 days post-index procedure were 7.78% (6.91–8.74%) among 8337 patients in the Ethicon manual circular stapler cohort, 7.54% (6.87–8.27%) among 7928 patients in the Medtronic EEA™ circular stapler with DST™ technology cohort, and 8.19% (6.57–10.07%) among 1306 patients in the Medtronic EEA™ circular stapler with Tri-Staple™ technology cohort. Comparative analyses revealed no difference comparing Ethicon manual circular staplers with Medtronic EEA™ circular staplers with Tri-Staple™ technology (risk ratio [RR], 0.72; 95% CI, 0.52–1.01) or comparing Medtronic EEA™ circular staplers with DST™ technology to Tri-Staple™ technology (RR, 0.75; 95% CI, 0.53–1.06).
Conclusion
In this analysis of a large cohort of patients undergoing a left-sided colorectal surgery from a U.S. hospital database, the risk of AL observed with manual two-row circular staplers was similar to that seen with three-row devices. This study affirms the safety of manual two-row circular staplers in colorectal anastomosis.
Similar content being viewed by others
Introduction
Prevention of anastomotic leak (AL) is an important goal in colorectal anastomosis [1, 2]. AL causes significant morbidity and mortality [3,4,5,6]. Several patient-related factors have been identified as risk factors for AL, including male sex, low anterior resection (more distal position of anastomosis), malnutrition, obesity, and diabetes [7,8,9,10].
With the development of novel circular stapling devices to facilitate colorectal anastomosis, there has been increased interest in specific device mechanics and their impact on AL risks. The primary variations in the stapling mechanics of commonly used circular staplers include closed height of staples, mechanical vs. powered mechanism for firing staples, shape of final staple form, and number of rows of staples. Various preclinical and clinical studies have demonstrated the safety and efficacy of these devices [11,12,13,14,15,16], but there are relatively few head-to-head studies of different devices and no prospective trials.
A retrospective single-center study by Mazaki et al. compared the Medtronic EEA™ circular stapler with Tri-Staple™ technology (a manual three-row circular stapler) to an unspecified two-row circular stapler in 256 patients with left-sided colon cancer resections and found risks of AL in the two-row and three-row groups of 7.7% and 2.7%, respectively (p = 0.23) [17]. A subsequent analyses added 29 patients without cancer and found a significantly higher AL risk in the two-row stapling group than the three-row group after propensity score matching (11.6% vs. 1.8%; p = 0.04) [18].
In another single-center head-to-head circular stapler comparison, Quero et al. [10] reported a lower overall AL risk after 375 rectal cancer resections in the Medtronic EEA™ circular stapler with Tri-Staple™ technology group (6/178, 3.4%) than the two-row stapler group (unspecified combination of Medtronic EEA™ circular stapler with DST™ Series technology and Ethicon™ circular stapler, 19/197, 9.6%) (p = 0.01). However, the risk of ISREC grade C AL [19], a severe form of AL leading to re-operation, did not differ between the two groups (2.5% in the two-row vs. 2.2% in the three-row circular stapler group).
These single-center retrospective studies not only have the potential for strong confounding due to within-institution treatment selection forces [20] but also can lack generalizability of AL risk due to small sample size and idiosyncratic regional, institutional, and patient characteristics. The Italian ColoRectal Anastomotic Leakage Study analyzed 2799 patients from 78 centers after elective left-sided colorectal resections (5.5% with open surgery) and reported a 5.0% AL risk in the overall study population [21]. After propensity score matching, only 850 patients were retained in the comparative analysis, showing the Medtronic EEA™ circular stapler with Tri-Staple™ technology (9/425, 2.1%) had a lower AL risk than the two-row stapler group (26/425, 6.1%) (p = 0.01). However, surgeon experience and intraoperative anastomotic testing and reinforcement were not measured in the study, which could affect the study results.
A comparative analysis of the risk of AL among two-row versus three-row manual circular staplers in colorectal anastomosis using a nationally representative database has not been conducted in the United States (U.S.). Healthcare databases can be a useful source of data for safety surveillance of medical devices and include a much larger sample size and many more hospitals than possible with single-center studies. Using data from a large U.S. hospital database, we sought to compare the risk of AL among patients who underwent left-sided colorectal surgery with anastomosis using a two-row Ethicon manual circular stapler versus the Medtronic EEA™ circular stapler with Tri-Staple™ technology. Additionally, the risk of AL among patients treated with the two-row Medtronic EEA™ circular stapler with DST™ Series technology was separately compared to those treated with the Tri-Staple™ technology.
Methods
Study design
A retrospective cohort study was conducted using electronic healthcare data from the Premier Healthcare Database (PHD). The PHD is a large, U.S. hospital-based, service-level, all-payer database that contains information on inpatient discharges from geographically diverse hospitals, including nonprofit, nongovernmental, community, and teaching hospitals in both rural and urban areas. More than 1000 hospitals have contributed data, including records for > 10 million visits per year [20]. The PHD consists of de-identified healthcare records. In the U.S., retrospective analyses of PHD data are considered exempt from informed consent and approval by an institutional review board.
Study population
Patients meeting all of the following criteria were included in the study: those who had billing charges for a study device (Ethicon manual circular staplers, Medtronic EEA™ circular stapler with DST Series™ technology, or Medtronic EEA™ circular stapler with Tri-Staple™ technology) at the index admission (i.e., the initial admission where a study device was identified) between January 1, 2019, and November 30, 2022; who underwent a left-sided colorectal surgery (i.e., the index procedure), defined as presence of a qualifying procedure code for left-sided colorectal surgery, at the index admission; and who were ≥ 18 years at the index admission.
Patients were excluded from the study if they had any of the following: missing data on age or sex (an indicator of poor data quality), presence of a diagnosis indicating AL on admission during the index admission, and billing charges for ≥ 2 study devices of interest during the index admission.
Study devices
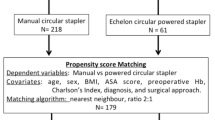
The study population was classified by device used: (1) Ethicon manual circular staplers (two-row), (2) Medtronic EEA™ circular stapler with DST™ technology (two-row), and (3) Medtronic EEA™ circular stapler with Tri-Staple™ technology (three-row). Ethicon manual circular staplers included Ethicon Legacy Curved Intraluminal Stapler, Legacy Endoscopic Intraluminal Stapler, and Ethicon™ Circular Stapler, XL Sealed. The ECHELON CIRCULAR™ Powered Stapler, which uses powered mechanism for firing staples, was not included in the study due to the different technology in comparison to manual circular staplers (fired under manual grip force). The identification of devices was based on a query of unstructured text fields in the PHD for model numbers and brand names, including variants such as misspellings and abbreviations.
Study outcome
The study outcome was AL within 30 days of the index procedure. A 30-day follow-up period was chosen as AL occurs at a median of 12 days (range, 3–30 days) after a colorectal procedure, and it is the standard post-operative follow-up period for most studies assessing AL after stapled anastomosis [22]. As there is no specific diagnosis code in the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) to assess AL, the incidence of AL was estimated via surrogate diagnoses that usually occur concomitantly with a leak. These included peritoneal abscess, peritonitis, fistula of intestine, or stoma formation post colorectal anastomosis procedure. As such, the presence of an ICD-10-CM diagnosis code for AL surrogate diagnoses (K63.2, K65.0, K65.1, K91.89, and Y83.2) either during the index admission or during a re-admission within 30 days post-index procedure or the presence of an ICD-10 procedure code indicating a diverting stoma (0D18%%4, 0D1B%%4, 0D1E%%4, 0D1H%%4, 0D1K%%4, 0D1L%%4, 0D1M%%4, 0D1N%%4) occurring within 1–30 days post-index procedure was used to define AL in the study. A similar approach has been used in studies assessing the risk of AL using electronic healthcare data, such as PHD [23] and the Nationwide Inpatient Sample database [24].
Statistical analyses
Descriptive analyses were performed to summarize the demographic, clinical, procedural, and provider characteristics at the time of the index procedure by study device. Unadjusted cumulative incidences and 95% confidence intervals (CIs) were estimated for all study cohorts and further stratified by key patient and provider characteristics.
We performed two head-to-head comparisons to estimate the risk ratio (RR) and 95% CI of AL for Ethicon manual circular staplers (two-row) compared to Medtronic EEA™ circular staplers with Tri-Staple™ technology (three-row) and to estimate the RR (95% CI) of AL for the Medtronic EEA™ circular stapler with DST™ technology compared to Tri-Staple™ technology. A propensity score weighting (PSW) method was used to control for potential confounders (i.e., demographic, clinical, procedural, and provider characteristics) by balancing the distribution of baseline characteristics between the comparison groups.
Trimmed and untrimmed PSW methods that estimate the average treatment effect on the treated were implemented and compared on the basis of covariate balance as measured by absolute standardized differences (ASD) in means and proportions, which compares difference in means or proportions in pooled standard deviation units. The PSW trimmed at the 99th percentile performed the best as measured by the fewest number of variables imbalanced (as indicated by an ASD value > 0.10) and the lowest mean ASD across all balanced covariates. One data analyst balanced the data without access to the outcome data and another data analyst performed the outcome analysis using the balanced data, thus removing the potential for bias resulting from repeated applications of covariate balancing to obtain a desired study outcome [25,26,27].
In the final PSW cohorts, covariate-balanced cumulative incidences and 95% CIs were estimated for all device cohorts. A weighted (covariate balance weights) log-binomial regression model was used with treatment as the only explanatory variable to estimate the covariate balanced RR (target group versus the comparator group for the study outcome of interest). A cluster (hospital) robust standard error approach was applied to estimate the variability in the RR estimate and to construct two-sided 95% CIs.
With the sample size available for the analysis (8000 in the 2-row manual circular stapler cohort and 1300 in the 3-row manual circular stapler cohort) and a cumulative incidence of AL of 8% in the 3-row manual circular stapler cohort, a power analysis indicated power of 0.995 (99.5%) to detect a RR of 1.5 or above in a 2-row manual circular stapler relative to a 3-row manual circular stapler at a significance level of 0.05 (or type I error of 0.05) in a two-sided test.
To evaluate the impact of an elective diverting stoma on the AL risk estimate, a secondary analysis was conducted to assess the association between the use of a two- vs. three-row circular stapler and the risk of AL among those who did not have a diverting stoma procedure prior to or on the same day as the index procedure. To minimize the potential impact of outcome misclassification resulting from loss of continuous enrollment in the PHD, a sensitivity analysis was conducted in patients from hospitals that had ≥ 30 days continuous enrollment in PHD after the patients’ index procedure.
Results
Study population
Across 447 U.S. hospitals, we identified 8337 patients who underwent a left-sided colorectal surgery with the use of Ethicon manual circular staplers, 7928 with the use of the Medtronic EEA™ circular stapler with DST™ technology, and 1306 with the use of Medtronic EEA™ circular stapler with Tri-Staple™ technology between January 1, 2019, and November 30, 2022. Most patients were white (80%), female (54%), and had a mean (SD) age of 60 (13) years. The majority of patients (64%) underwent a sigmoid colectomy based on the primary procedure code. The index procedures were predominantly performed in an inpatient setting (99%), elective (nonurgent, 84%), and in a large hospital (76%). Over 40% of patients in the two-row circular stapler cohorts underwent an open surgery, while 40% in the three-row cohort underwent a robotic-assisted surgery. Approximately 16% had a diverting stoma prior to or on the same day as the index procedure during the index admission, which was similar across the three cohorts. Among those, 99% had a diverting stoma identified on the same day as the index procedure (Table 1).
Unadjusted cumulative incidences of AL (95% CIs) were 7.78% (6.91–8.74%) in the Ethicon manual circular stapler cohort, 7.54% (6.87–8.27%) in the Medtronic EEA™ circular stapler with DST™ technology cohort, and 8.19% (6.57–10.07%) in the Medtronic EEA™ circular stapler with Tri-Staple™ technology cohort within 30 days post-index procedure (Tables 2 and 3).
Comparative risk of AL within 30 days post-index procedure
Ethicon manual circular staplers vs. Medtronic EEA™ circular stapler with Tri-Staple™ technology
Some imbalances in baseline characteristics between the Ethicon manual circular stapler and Medtronic EEA™ circular stapler with Tri-Staple™ technology cohorts were observed. Following PSW, adequate covariate balance between two cohorts was achieved (Table 4).
The comparative analysis based on the PSW cohort found that the use of the Ethicon manual circular stapler was not associated with an increased risk of AL within 30 days post-index procedure in comparison to the Medtronic EEA™ circular stapler with Tri-Staple™ technology (RR, 0.72; 95% CI, 0.52–1.01) (Table 2).
Secondary analyses revealed similar results in patients who did not have a diverting stoma procedure prior to or on the same day as the index procedure. The cumulative incidences (95% CIs) were 7.09% (6.21–8.05%) in the Ethicon manual circular stapler cohort and 7.21% (5.67–9.01%) in the Medtronic EEA™ circular stapler with Tri-Staple™ technology cohort. After PSW, the RR was 0.77 (0.50–1.18) (Table 2). Similar results were also observed in the sensitivity analysis that only included patients from hospitals with ≥ 30 days continuous enrollment in PHD after the patients’ index procedure (RR, 0.73; 95% CI, 0.52–1.01) (Table 2).
Medtronic EEA™ circular stapler with DST™ technology vs. Medtronic EEA™ circular stapler with Tri-Staple™ technology
Observed imbalances between the Medtronic EEA™ circular stapler with DST™ technology and Tri-Staple™ technology cohorts were adequately resolved with PSW (Table 5).
The comparative analysis based on the PSW cohort revealed no difference in the risk of AL within 30 days post-index procedure comparing the Medtronic EEA™ circular stapler with DST™ technology to Tri-Staple™ technology (RR, 0.75; 95% CI, 0.53–1.06) (Table 3).
Secondary and sensitivity results were consistent with those of the primary analysis (Table 3). Among patients who did not have diverting stoma prior to or on the same day as the index procedure, the RR of AL comparing Medtronic EEA™ circular stapler with DST™ technology to Tri-Staple™ technology was 0.80 (95% CI, 0.51–1.26). Among patients from hospitals with ≥ 30 days continuous enrollment in PHD after the patients’ index procedure, the RR was 0.75 (95% CI, 0.53–1.06).
Cumulative incidences of AL stratified by patient and provider characteristics
Analyses stratified by key characteristics suggest the risk of AL has remained steady since 2019, when the three-row circular staplers were introduced to the U.S. market (Table 6). The risk of AL in patients who underwent an open procedure was approximately doubled compared to patients who underwent a laparoscopic or robotic-assisted procedure (10.3% vs. 5.9%). Similar AL risk was noted across all 3 device cohorts when stratified by hospital and provider characteristics including hospital size, hospital volume, and surgeon specialty.
Discussion
We present the first large U.S.-based cohort study of left-sided colorectal resection for AL risk based on circular stapler device used, specifically comparing two- and three-row devices. Both the Ethicon and Medtronic two-row staplers had similar AL risks as the three-row stapler before and after PSW. Similar results were found for patients who did not have a diverting stoma prior to or on the same day as a left-sided colorectal surgery during the index admission.
The observed cumulative incidences of AL in this study for a two-row manual circular stapler are consistent with those reported in an observational study conducted using this same data source [23], three single-center studies [10, 17, 18] and one multicenter observational study [21] with a head-to-head comparison between two-row and three-row circular staplers.
In contrast, the estimated cumulative incidences of AL in patient procedures performed using a three-row circular stapler were below 3% in four previously published studies [10, 17, 18, 21], lower than the present study [8.2% (6.6–10.1%)], even among those who underwent a minimally invasive [5.9% (3.3–9.6%)] or robotic-assisted surgery [7.5% (5.8–9.5%)]. This difference could be partially explained by differences in outcome ascertainment. A gold standard for diagnosing AL is currently lacking. The diagnosis of an AL generally requires patient’s global clinical assessment, adjunctive laboratory data, and radiological assessment, and the decision of a diagnosis sometimes can be different depending on physicians’ clinical judgment [28, 29]. In a retrospective observational study based on the review of patient’s medical records, without an adjudication process in place, investigators’ knowledge of exposure status and study hypothesis (i.e., unblinded outcome classification) could have resulted in potential for differential misclassification of AL, particularly for less severe AL. In the Quero et al. study, less severe AL cases (i.e., ISREC grade A or B) accounted for only 1/3 of AL identified in the three-row cohort while 74% of ALs identified in the two-row population were less severe10. This could lead to an underestimation of AL risk in patient procedures using a three-row manual circular stapler in these four published studies based on review of medical records. In contrast, the ascertainment of AL in the present study was based on the identification of existing diagnosis and/or procedural codes readily available in the PHD, which were collected and maintained for billing or record-keeping purposes prior to the conduct of this study and independent of the study hypothesis.
Observational studies using real-world data such as the PHD have both strengths and limitations. Relative to four recently published studies [10, 17, 18, 21], the key strengths of this study are the large and regionally diverse sample of U.S. patients as well as the rigorous approach to addressing confounding, which improves the comparability between the two-row and three-row manual circular stapler groups. As with other studies examining colorectal AL, there are limitations related to the definition and diagnostic criteria, as there is no specific code for AL in the ICD-10-CM taxonomy and surrogate diagnoses must be used [29]. Misclassification bias would result if study patients were not categorized correctly with regard to outcome; since the AL definition was applied equally across all the three cohorts, this would be nondifferential and the impact could be a bias towards the null. PHD is not a longitudinal patient database; rather, it is a longitudinal hospital database for the duration of continuous participation in PHD from each institution. Longitudinal data are available only for follow-up encounters within the same hospital where the index procedure was performed. This could theoretically lead to underreporting of AL risks if patients were discharged and presented with new AL to a different hospital. However, we expect this underestimation to be low, as patients with surgical complications that occur within 30 days of a surgical procedure would be likely to return to the same hospital where they received the surgical procedure. Should underestimation occur, this would probably be nondifferential among study cohorts, as patient decisions to return to the same hospital unlikely depend on device used. Furthermore, a sensitivity analysis including patients from hospitals with ≥ 30-day continuous enrollment in PHD after the patients’ index procedure produced results that were consistent with those of the primary analysis suggesting that misclassification of outcome resulting from loss of institution continuous enrollment in the PHD is unlikely.
Conclusion
In conclusion, in the analysis of a large cohort of patients undergoing a left-sided colorectal surgery from a U.S. hospital database, the risk of AL observed with manual two-row circular staplers is similar to that seen with three-row devices. This study affirms the safety of manual two-row circular staplers in colorectal anastomosis.
Data availability
Data used in this analysis were extracted from the Premier Healthcare Database (owned by Premier Inc., Charlotte, NC, USA) on February 27, 2023.
References
Chiarello MM et al (2022) Anastomotic leakage in colorectal cancer surgery. Surg Oncol 40:101708
McDermott FD et al (2015) Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg 102(5):462–479
Ashraf SQ et al (2013) The economic impact of anastomotic leakage after anterior resections in English NHS hospitals: are we adequately remunerating them? Colorectal Dis 15(4):e190–e198
Frye J et al (2009) Anastomotic leakage after resection of colorectal cancer generates prodigious use of hospital resources. Colorectal Dis 11(9):917–920
Kube R et al (2010) Anastomotic leakage after colon cancer surgery: a predictor of significant morbidity and hospital mortality, and diminished tumour-free survival. Eur J Surg Oncol 36(2):120–124
Zoucas E, Lydrup ML (2014) Hospital costs associated with surgical morbidity after elective colorectal procedures: a retrospective observational cohort study in 530 patients. Patient Saf Surg 8(1):2
Asteria CR et al (2008) Anastomotic leaks after anterior resection for mid and low rectal cancer: survey of the Italian Society of Colorectal Surgery. Tech Coloproctol 12(2):103–110
Frasson M et al (2016) Risk factors for anastomotic leak and postoperative morbidity and mortality after elective right colectomy for cancer: results from a prospective, multicentric study of 1102 patients. Int J Colorectal Dis 31(1):105–114
Parthasarathy M et al (2017) Risk factors for anastomotic leakage after colorectal resection: a retrospective analysis of 17 518 patients. Colorectal Dis 19(3):288–298
Quero G et al (2022) Preliminary evaluation of two-row versus three-row circular staplers for colorectal anastomosis after rectal resection: a single-center retrospective analysis. Int J Colorectal Dis 37(12):2501–2510
Cheregi CD et al (2017) Mechanical suture in rectal cancer. Clujul Med 90(3):305–312
De Nardi P, Panzeri F, Staudacher C (2008) Prospective trial evaluating new circular and linear stapler devices for gastrointestinal anastomosis: preliminary data. Tech Coloproctol 12(1):69–72
Herzig DO et al (2020) Assessment of a circular powered stapler for creation of anastomosis in left-sided colorectal surgery: a prospective cohort study. Int J Surg 84:140–146
Nakanishi R et al (2022) Clinical impact of the triple-layered circular stapler for reducing the anastomotic leakage in rectal cancer surgery: porcine model and multicenter retrospective cohort analysis. Ann Gastroenterol Surg 6(2):256–264
Sun Q et al (2022) Short-term outcomes of tri-staple versus universal staple in laparoscopic anterior resection of rectal and distal sigmoid colonic cancer: a matched-pair analysis. World J Surg 46(11):2817–2824
Wester T, Hoehner J, Olsen L (1995) Rehbein’s anterior resection in Hirschsprung’s disease, using a circular stapler. Eur J Pediatr Surg 5(6):358–362
Mazaki J et al (2021) A novel predictive model for anastomotic leakage in colorectal cancer using auto-artificial intelligence. Anticancer Res 41(11):5821–5825
Mazaki J et al (2022) Effectiveness of a new triple-row circular stapler in reducing the risk of colorectal anastomotic leakage: a historical control and propensity score–matched study. Medicine 101(27):e29325
Rahbari NN et al (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147(3):339–351
Walker AM (2013) Matching on provider is risky. J Clin Epidemiol 66(8 Suppl):S65–68
Catarci M et al (2023) Three- versus two-rows circular staplers for left-sided colorectal anastomosis: a propensity score-matched analysis of the iCral 2 and 3 prospective cohorts. Int J Surg. Publish Ahead of Print
Jörgren F et al (2011) Anastomotic leakage after surgery for rectal cancer: a risk factor for local recurrence, distant metastasis and reduced cancer-specific survival? Colorectal Dis 13(3):272–283
Sylla P et al (2022) Outcomes associated with the use of a new powered circular stapler for left-sided colorectal reconstructions: a propensity score matching-adjusted indirect comparison with manual circular staplers. Surg Endosc 36(4):2541–2553
Kang CY et al (2013) Risk factors for anastomotic leakage after anterior resection for rectal cancer. JAMA Surg 148(1):65–71
Rubin DB (2007) The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med 26(1):20–36
Cafri G, Paxton E (2018) Mitigating reporting bias in observational studies using covariate balancing methods. Obs Studies 4:292–296
Yue LQ (2012) Regulatory considerations in the design of comparative observational studies using propensity scores. J Biopharm Stat 22(6):1272–1279
Hernandez PT, Paspulati RM, Shanmugan S (2021) Diagnosis of anastomotic leak. Clin Colon Rectal Surg 34(6):391–399
Bruce J et al (2002) Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg 88(9):1157–1168
Acknowledgements
The authors wish to acknowledge the contributions of Muskan Sethia to the data analysis and the contributions of Guy Cafri PhD to the statistical methods. The authors thank Stephen Marcello MD FACC, Guy Cafri PhD, Stephen Johnston PhD, and Joshua J Gagne PharmD, ScD, for their critical review of the manuscript.
Author information
Authors and Affiliations
Contributions
Tongtong Wang, Mordechai Sadowsky, Rebekah Blakney, Paul Coplan, William Petraiuolo, Mark Soberman, Joerg Tomaszewski, Lexi Rene, and Jennifer Wood meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. Tongtong Wang, Paul Coplan, William Petraiuolo, Mark Soberman, Joerg Tomaszewski, and Jennifer Wood conceived, designed, and/or planned the study. Rebekah Blakney and Lexi Rene conducted the data analysis. All named authors interpreted the results. Tongtong Wang and Mordechai Sadowsky drafted the manuscript. All named authors critically reviewed and/or revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study utilized a secondary source of de‐identified data—Premier Healthcare Database (PHD). In the US, retrospective analyses of the PHD data are considered exempt from informed consent and institutional review board (IRB) approval as dictated by Title 45 Code of Federal Regulations, Part 46 of the United States, specifically 45 CFR 46.101(b)(4).
Competing interests
Johnson & Johnson, which is the designer of the device, funded the study and the authors are either employees or research fellow of Johnson & Johnson or contractors funded by Johnson & Johnson at the time of the conduct of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, T., Sadowsky, M., Blakney, R. et al. Risk of anastomotic leakage with two-row versus three-row manual circular staplers in colorectal anastomosis: a U.S. cohort study. Int J Colorectal Dis 38, 264 (2023). https://doi.org/10.1007/s00384-023-04552-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04552-0