Abstract
Objective
The association between constipation and depression or suicidal ideation (SI) has not been adequately studied. This study aims to examine whether constipation is associated with depression or SI in US adults.
Method
4,562 adults aged 20 and older were selected from the National Health and Nutrition Examination Survey 2009–2010 for the sample. The Bowel Health Questionnaire provided constipation information. Clinical depression and depression severity were assessed by the validated Patient Health Questionnaide-9 (PHQ-9), and item 9 of the PHQ-9 assessed SI. Adjusted odds ratios (ORs) were calculated using multivariate logistic regression models. Stability of the results was ensured by a subgroup analysis.
Result
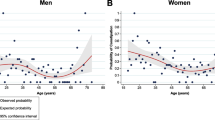
After adjusting for covariates such as demographics, risk behaviors, associated comorbidities, dietary intake, and related medications, the PHQ-9 score and clinical depression were both significantly associated with constipation, with ORs and 95%CIs of 1.13 (1.10–1.16) and 3.76 (2.65–5.34). Depression of all severities was also significantly associated with constipation. The ORs and 95%CIs of constipation with mild depression, moderate depression, and moderately severe to severe depression were 2.21 (1.54–3.16), 3.69 (2.34–5.81) and 6.84 (4.19–11.15), respectively. Subgroup analyses showed no statistically significant interactions (P > 0.05), and the association was stronger in men than in women (OR: 7.81, 95%CI: 3.67–16.61 vs OR: 3.46, 95%CI: 2.31–5.19). The association between constipation and SI was not significant (OR: 1.36, 95%CI: 0.78–2.37).
Conclusion
In conclusion, constipation was significantly associated with depression of any severity, but not with SI, suggesting that enough attention should be paid to the emotional and psychological status of patients with constipation, especially male patients.


Similar content being viewed by others
Data availability
Publicly available and de-identified data used in this analysis can be found in the CDC National Center for Health Statistics NHANES database at https://wwwn.cdc.gov/nchs/nhanes/Default.as px.
References
Schmidt FM, Santos VL (2014) Prevalence of constipation in the general adult population: an integrative review. J Wound Ostomy Continence Nurs 41:70–76; quiz E1–2. https://doi.org/10.1097/01.WON.0000438019.21229.b7
Irvine EJ, Ferrazzi S, Pare P, Thompson WG, Rance L (2002) Health-related quality of life in functional GI disorders: focus on constipation and resource utilization. Am J Gastroenterol 97:1986–1993. https://doi.org/10.1111/j.1572-0241.2002.05843.x
Sethi S, Mikami S, Leclair J, Park R, Jones M, Wadhwa V et al (2014) Inpatient burden of constipation in the United States: an analysis of national trends in the United States from 1997 to 2010. Am J Gastroenterol 109:250–256. https://doi.org/10.1038/ajg.2013.423
Mykletun A, Jacka F, Williams L, Pasco J, Henry M, Nicholson GC, Kotowicz MA, Berk M (2010) Prevalence of mood and anxiety disorder in self reported irritable bowel syndrome (IBS). An epidemiological population based study of women. BMC Gastroenterol 10:88. https://doi.org/10.1186/1471-230X-10-88
Fuller-Thomson E, Sulman J (2006) Depression and inflammatory bowel disease: findings from two nationally representative Canadian surveys. Inflamm Bowel Dis 12(8):697–707. https://doi.org/10.1097/00054725-200608000-00005
Bhandari S, Larson ME, Kumar N, Stein D (2017) Association of inflammatory bowel disease (IBD) with depressive symptoms in the United States population and independent predictors of depressive symptoms in an IBD population: a NHANES study. Gut Liver 11(4):512–519. https://doi.org/10.5009/gnl16347
Triantafillidis JK, Hyphantis T, Cheracakis P, Antoniou A, Sklavaina M (2002) Suicide as an outcome in patients with inflammatory bowel disease. Am J Gastroenterol 97:1066–1068. https://doi.org/10.1111/j.1572-0241.2002.05636.x
Miller V, Hopkins L, Whorwell PJ (2004) Suicidal ideation in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2:1064–1068. https://doi.org/10.1016/s1542-3565(04)00545-2
Guan S, Shen Y, Ge H, Xiong W, He L, Liu L, Yin C, Wei X, Gao Y (2019) Dihydromyricetin alleviates diabetic neuropathic pain and depression comorbidity symptoms by inhibiting P2X7 receptor. Front Psychiatry 10:770. https://doi.org/10.3389/fpsyt.2019.00770
Nestler EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM (2002) Neurobiology of depression. Neuron 34:13–25. https://doi.org/10.1016/s0896-6273(02)00653-0
Li RX, Ma M, Xiao XR, Xu Y, Chen XY, Li B (2016) Perimenopausal syndrome and mood disorders in perimenopause: prevalence, severity, relationships, and risk factors. Medicine (Baltimore) 95:e4466. https://doi.org/10.1097/MD.0000000000004466
Malhi GS, Mann JJ (2018) Depression. Lancet 392:2299–2312. https://doi.org/10.1016/S0140-6736(18)31948-2
Hawton K, van Heeringen K (2009) Suicide. Lancet 373:1372–1381. https://doi.org/10.1016/S0140-6736(09)60372-X
Organization WH (2014) Preventing suicide: A global imperative. World Health Organization
Merson MH, Black RE, Mills AJ (2012) Global health. third ed. Burlington, MA: Jones & Bartlett Learning
Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S (2008) Suicide and suicidal behavior. Epidemiol Rev 30:133–154. https://doi.org/10.1093/epirev/mxn002
Mann JJ, Waternaux C, Haas GL, Malone KM (1999) Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 156:181–189. https://doi.org/10.1176/ajp.156.2.181
Shirazi A, Stubbs B, Gomez L, Moore S, Gaughran F, Flanagan RJ, MacCabe JH, Lally J (2016) Prevalence and predictors of clozapine-associated constipation: a systematic review and meta-analysis. Int J Mol Sci 17:863. https://doi.org/10.3390/ijms17060863
Yang LS, Khera A, Kamm MA (2014) Outcome of behavioural treatment for idiopathic chronic constipation. Intern Med J 44:858–864. https://doi.org/10.1111/imj.12490
Müller-Lissner S, Pehl C (2012) Laxanziengebrauch und Zufriedenheit chronisch obstipierter Frauen - eine Umfrage bei Patientinnen und Gastroenterologen in Deutschland [Laxative use and satisfaction of chronically constipated women-a survey of female patients and gastroenterologists in Germany]. Z Gastroenterol 50:573–577. German. https://doi.org/10.1055/s-0031-1299133
Kim JY, Lim MH (2021) Psychological factors to predict chronic diarrhea and constipation in Korean high school students. Medicine (Baltimore) 100:e26442. https://doi.org/10.1097/MD.0000000000026442
Rajindrajith S, Ranathunga N, Jayawickrama N, van Dijk M, Benninga MA, Devanarayana NM (2020) Behavioral and emotional problems in adolescents with constipation and their association with quality of life. PLoS ONE 15:e0239092. https://doi.org/10.1371/journal.pone.0239092
Adibi P, Abdoli M, Daghaghzadeh H, Keshteli AH, Afshar H, Roohafza H, Esmaillzadeh A, Feizi A (2022) Relationship between depression and constipation: results from a large cross-sectional study in adults. Korean J Gastroenterol 80:77–84. https://doi.org/10.4166/kjg.2022.038
Andy UU, Vaughan CP, Burgio KL, Alli FM, Goode PS, Markland AD (2016) Shared risk factors for constipation, fecal incontinence, and combined symptoms in older U.S. adults. J Am Geriatr Soc 64:e183–e188. https://doi.org/10.1111/jgs.14521
Ballou S, Katon J, Singh P, Rangan V, Lee HN, McMahon C, Iturrino J, Lembo A, Nee J (2019) Chronic diarrhea and constipation are more common in depressed individuals. Clin Gastroenterol Hepatol 17:2696–2703. https://doi.org/10.1016/j.cgh.2019.03.046
CDC (2009) Centers for Disease Control and Preventions National Health and Nutrition Examination Survey: questionnaires, datasets, and related documentation
Li Y, Tong WD, Qian Y (2021) Effect of physical activity on the association between dietary fiber and constipation: evidence from the national health and nutrition examination survey 2005–2010. J Neurogastroenterol Motil 27:97–107. https://doi.org/10.5056/jnm20051
Zhao X, Wang L, Quan L (2023) Association between dietary phosphorus intake and chronic constipation in adults: evidence from the National Health and Nutrition Examination Survey. BMC Gastroenterol 23:24. https://doi.org/10.1186/s12876-022-02629-8
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kroenke K (2012) Enhancing the clinical utility of depression screening. CMAJ 184:281–282. https://doi.org/10.1503/cmaj.112004
Li L, Sun W, Luo J, Huang H (2022) Associations between education levels and prevalence of depressive symptoms: NHANES (2005–2018). J Affect Disord 301:360–367. https://doi.org/10.1016/j.jad.2022.01.010
Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, Ludman EJ (2013) Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv 64:1195–1202. https://doi.org/10.1176/appi.ps.201200587
Moazzami K, Dolmatova EV, Feurdean M (2018) Suicidal ideation among adults with cardiovascular disease: The National Health and Nutrition Examination Survey. Gen Hosp Psychiatry 51:5–9. https://doi.org/10.1016/j.genhosppsych.2017.12.001
Tektonidou MG, Dasgupta A, Ward MM (2011) Suicidal ideation among adults with arthritis: prevalence and subgroups at highest risk. Data from the 2007–2008 National Health and Nutrition Examination Survey. Arthritis Care Res (Hoboken) 63:1322–1333. https://doi.org/10.1002/acr.20516
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH (2009) The PHQ-8 as a measure of current depression in the general population. J Affect Disord 114:163–173. https://doi.org/10.1016/j.jad.2008.06.026
Ranasinghe N, Devanarayana NM, Benninga MA, van Dijk M, Rajindrajith S (2017) Psychological maladjustment and quality of life in adolescents with constipation. Arch Dis Child 102:268–273. https://doi.org/10.1136/archdischild-2016-310694
Dimidi E, Christodoulides S, Scott SM, Whelan K (2017) Mechanisms of action of probiotics and the gastrointestinal microbiota on gut motility and constipation. Adv Nutr 8:484–494. https://doi.org/10.3945/an.116.014407
Jacobsen JP, Medvedev IO, Caron MG (2012) The 5-HT deficiency theory of depression: perspectives from a naturalistic 5-HT deficiency model, the tryptophan hydroxylase 2Arg439His knockin mouse. Philos Trans R Soc Lond B Biol Sci 367:2444–2459. https://doi.org/10.1098/rstb.2012.0109
O’Reardon JP, Chopra MP, Bergan A, Gallop R, DeRubeis RJ, Crits-Christoph P (2004) Response to tryptophan depletion in major depression treated with either cognitive therapy or selective serotonin reuptake inhibitor antidepressants. Biol Psychiatry 55:957–959. https://doi.org/10.1016/j.biopsych.2003.12.020
Haynes PL, McQuaid JR, Kelsoe J, Rapaport M, Gillin JC (2004) Affective state and EEG sleep profile in response to rapid tryptophan depletion in recently recovered nonmedicated depressed individuals. J Affect Disord 83:253–262. https://doi.org/10.1016/j.jad.2004.05.010
Mönnikes H, Tebbe JJ, Hildebrandt M, Arck P, Osmanoglou E, Rose M, Klapp B, Wiedenmann B, Heymann-Mönnikes I (2001) Role of stress in functional gastrointestinal disorders. Evidence for stress-induced alterations in gastrointestinal motility and sensitivity. Dig Dis 19:201–211. https://doi.org/10.1159/000050681
Taché Y, Martinez V, Million M, Wang L (2001) Stress and the gastrointestinal tract III. Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptors. Am J Physiol Gastrointest Liver Physiol 280:G173–G177. https://doi.org/10.1152/ajpgi.2001.280.2.G173
Mayer EA, Naliboff BD, Chang L, Coutinho SVV (2001) Stress and irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol 280:G519–G524. https://doi.org/10.1152/ajpgi.2001.280.4.G519
Arborelius L, Owens MJ, Plotsky PM, Nemeroff CB (1999) The role of corticotropin-releasing factor in depression and anxiety disorders. J Endocrinol 160:1–12. https://doi.org/10.1677/joe.0.1600001
Kehne JH (2007) The CRF1 receptor, a novel target for the treatment of depression, anxiety, and stress-related disorders. CNS Neurol Disord Drug Targets 6:163–182. https://doi.org/10.2174/187152707780619344
Taché Y, Kiank C, Stengel A (2009) A role for corticotropin-releasing factor in functional gastrointestinal disorders. Curr Gastroenterol Rep 11:270–277. https://doi.org/10.1007/s11894-009-0040-4
Ohara T, Suzutani T (2018) Efficacy of fecal microbiota transplantation in a patient with chronic intractable constipation. Clin Case Rep 6:2029–2032. https://doi.org/10.1002/ccr3.1798
Macfarlane GT, Macfarlane S, Gibson GR (1998) Validation of a three-stage compound continuous culture system for investigating the effect of retention time on the ecology and metabolism of bacteria in the human colon. Microb Ecol 35:180–187. https://doi.org/10.1007/s002489900072
Jiang D, Zhang J, Lin S, Wang Y, Chen Y, Fan J (2021) Prolyl endopeptidase gene disruption improves gut dysbiosis and non-alcoholic fatty liver disease in mice induced by a high-fat diet. Front Cell Dev Biol 9:628143. https://doi.org/10.3389/fcell.2021.628143
Tian B, Zhao J, Xie X, Chen T, Yin Y, Zhai R, Wang X, An W, Li J (2021) Anthocyanins from the fruits of Lycium ruthenicum Murray improve high-fat diet-induced insulin resistance by ameliorating inflammation and oxidative stress in mice. Food Funct 12:3855–3871. https://doi.org/10.1039/d0fo02936j
Janeiro MH, Ramírez MJ, Milagro FI, Martínez JA, Solas M (2018) Implication of trimethylamine N-oxide (TMAO) in disease: potential biomarker or new therapeutic target. Nutrients 10:1398. https://doi.org/10.3390/nu10101398
Ghosh SS, Wang J, Yannie PJ, Ghosh S (2020) Intestinal barrier dysfunction, LPS translocation, and disease development. J Endocr Soc. 4:bvz039. https://doi.org/10.1210/jendso/bvz039
Pandolfi F, Franza L, Carusi V, Altamura S, Andriollo G, Nucera E (2020) Interleukin-6 in rheumatoid arthritis. Int J Mol Sci 21:5238. https://doi.org/10.3390/ijms21155238
Qi T, Jing R, Wen C, Hu C, Wang Y, Pei C, Ma B (2020) Interleukin-6 promotes migration and extracellular matrix synthesis in retinal pigment epithelial cells. Histochem Cell Biol 154:629–638. https://doi.org/10.1007/s00418-020-01923-4
Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, Mariat D, Corthier G, Doré J, Henegar C, Rizkalla S, Clément K (2010) Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes 59:3049–3057. https://doi.org/10.2337/db10-0253
Rohrmann S, Linseisen J, Allenspach M, von Eckardstein A, Müller D (2016) Plasma concentrations of trimethylamine-N-oxide are directly associated with dairy food consumption and low-grade inflammation in a German adult population. J Nutr 146:283–289. https://doi.org/10.3945/jn.115.220103
Leonard BE (2018) Inflammation and depression: a causal or coincidental link to the pathophysiology? Acta Neuropsychiatr 30:1–16. https://doi.org/10.1017/neu.2016.69
Liu JJ, Wei YB, Strawbridge R, Bao Y, Chang S, Shi L, Que J, Gadad BS, Trivedi MH, Kelsoe JR, Lu L (2020) Peripheral cytokine levels and response to antidepressant treatment in depression: a systematic review and meta-analysis. Mol Psychiatry 25:339–350. https://doi.org/10.1038/s41380-019-0474-5
Cryan JF, O’Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O’Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG (2019) The microbiota-gut-brain axis. Physiol Rev 99:1877–2013. https://doi.org/10.1152/physrev.00018.2018
Baile MG, Guiney EL, Sanford EJ, MacGurn JA, Smolka MB, Emr SD (2019) Activity of a ubiquitin ligase adaptor is regulated by disordered insertions in its arrestin domain. Mol Biol Cell 30:3057–3072. https://doi.org/10.1091/mbc.E19-08-0451
Miller AH, Maletic V, Raison CL (2009) Inflammation and its discontents: the role of cytokines in the pathophysiology of major depression. Biol Psychiatry 65:732–741. https://doi.org/10.1016/j.biopsych.2008.11.029
Seo JS, Wei J, Qin L, Kim Y, Yan Z, Greengard P (2017) Cellular and molecular basis for stress-induced depression. Mol Psychiatry 22:1440–1447. https://doi.org/10.1038/mp.2016.118
Acknowledgements
We thank Dr. Liu Jie (People’s Liberation Army of China General Hospital,Beijing, China) and Dr.Yang Qilin (The Second Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China) for helping in this revision.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows—Pengfei Wang, Xia Shen, Yan Wang: contributed to study planning, data analyses and drafting of the manuscript; Pengfei Wang, Yan Wang: contributed to study planning and manuscript development; All authors: read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics statement
Institutional Research Ethics Review Board of the CDC approved the protocol for the NHANES survey. The protocol was approved by the NCHS Ethics Review Board with informed consent from all participants.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Shen, X. & Wang, P. Constipation is associated with depression of any severity, but not with suicidal ideation: insights from a large cross-sectional study. Int J Colorectal Dis 38, 231 (2023). https://doi.org/10.1007/s00384-023-04520-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04520-8