Abstract
Purpose
The aim of this review was to examine if diverticulitis increases the long-term risk (> 6 months) of developing colon cancer.
Methods
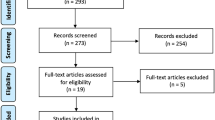
A systematic search was conducted in PubMed, Embase, and Cochrane CENTRAL. Google Scholar was also searched. We included studies with human adults of 18 years of age and above. Studies that included only patients with diverticulitis as well as studies comparing groups with and without diverticulitis were included. The primary outcome was the incidence of colon cancer 6 months or more after an episode of diverticulitis.
Results
Twelve records were included with 38,621 patients with diverticulitis. The crude rate of colon cancer among the prospectively followed populations with diverticulitis was by meta-analysis found to be 0.6% (95% CI 0.5–0.6%). The limitations of this review include heterogeneous reporting of outcomes across studies, specifically regarding population and outcome as well as variations in the design and reporting of the studies.
Conclusion
We found that the long-term risk of colon cancer after diverticulitis is not increased. The results of our review support current practice on follow-up after an episode of diverticulitis with short-term follow-up being the primary focus.



Similar content being viewed by others
References
Peery AF, Crockett SD, Murphy CC et al (2019) Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 156:254–72.e11. https://doi.org/10.1053/j.gastro.2018.08.063
Peery AF, Keku TO, Martin CF et al (2016) Distribution and characteristics of colonic diverticula in a United States screening population. Clin Gastroenterol Hepatol 14:980–5.e1. https://doi.org/10.1016/j.cgh.2016.01.020
Rawla P, Sunkara T, Barsouk A (2019) Epidemiology of colorectal cancer: incidence, mortality, survival, and risk factors. Prz Gastroenterol 14:89–103. https://doi.org/10.5114/pg.2018.81072
Murata M (2018) Inflammation and cancer. Environ Health Prev Med 23:50. https://doi.org/10.1186/s12199-018-0740-1
Hussain SP, Harris CC (2007) Inflammation and cancer: an ancient link with novel potentials. Int J Cancer 121:2373–2380. https://doi.org/10.1002/ijc.23173
Freeman HJ (2008) Colorectal cancer risk in Crohn’s disease. World J Gastroenterol 14:1810–1811. https://doi.org/10.3748/wjg.14.1810
Stidham RW, Higgins PDR (2018) Colorectal cancer in inflammatory bowel disease. Clin Colon Rectal Surg 31:168–178. https://doi.org/10.1055/s-0037-1602237
Eaden JA, Abrams KR, Mayberry JF (2001) The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut 48:526–535. https://doi.org/10.1136/gut.48.4.526
Axelrad JE, Lichtiger S, Yajnik V (2016) Inflammatory bowel disease and cancer: the role of inflammation, immunosuppression, and cancer treatment. World J Gastroenterol 22:4794–4801. https://doi.org/10.3748/wjg.v22.i20.4794
Stefánsson T, Ekbom A, Sparèn P, Påhlman L (1993) Increased risk of left sided colon cancer in patients with diverticular disease. Gut 34:499–502. https://doi.org/10.1136/gut.34.4.499
Lau KC, Spilsbury K, Farooque Y et al (2011) Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: can colorectal cancer be confidently excluded? Dis Colon Rectum 54:1265–1270. https://doi.org/10.1097/DCR.0b013e31822899a2
Mortensen LQ, Burcharth J, Andresen K, Pommergaard HC, Rosenberg J (2017) An 18-year nationwide cohort study on the association between diverticulitis and colon cancer. Ann Surg 265:954–959. https://doi.org/10.1097/SLA.0000000000001794
Ng ZQ, Moe KS, Wijesuriya R (2019) Routine colonoscopy after acute diverticulitis: is it warranted? Surg Laparosc Endosc Percutan Tech 29:462–466. https://doi.org/10.1097/SLE.0000000000000680
Asaad P, Hajibandeh S, Rahm M, Johnston T, Chowdhury S, Bronder C (2019) Should a colonoscopy be offered routinely to patients with CT proven acute diverticulitis? A retrospective cohort study and meta-analysis of best available evidence. World J Gastrointest Endosc 11:427–437. https://doi.org/10.4253/wjge.v11.i7.427
Suhardja TS, Norhadi S, Seah EZ, Rodgers-Wilson S (2017) Is early colonoscopy after CT-diagnosed diverticulitis still necessary? Int J Colorectal Dis 32:485–489. https://doi.org/10.1007/s00384-016-2749-5
Grahnat CJ, Hérard S, Ackzell A, Andersson RE (2016) High probability of an underlying colorectal cancer among patients treated for acute diverticulitis. A population-based cohort follow-up study. World J Surg 40:2283–2288. https://doi.org/10.1007/s00268-016-3480-7
Andrade P, Ribeiro A, Ramalho R, Lopes S, Macedo G (2017) Routine colonoscopy after acute uncomplicated diverticulitis - challenging a putative indication. Dig Surg 34:197–202. https://doi.org/10.1159/000449259
Mortensen LQ, Buciek J, Andresen K, Rosenberg J (2020) Diverticulitis does not increase the long-term risk of developing colon cancer – a systematic review and meta-analysis. PROSPERO. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020191055. Accessed 5 July 2022.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ339:b2535. https://doi.org/10.1136/bmj.b2535
Greenhalgh T, Peacock R (2005) Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 331:1064–1065. https://doi.org/10.1136/bmj.38636.593461.68
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Wasvary H, Turfah F, Kadro O, Beauregard W (1999) Same hospitalization resection for acute diverticulitis. Am Surg 65:632–635
Stefánsson T, Ekbom A, Sparèn P, Påhlman L (2004) Association between sigmoid diverticulitis and left-sided colon cancer: a nested, population-based, case control study. Scand J Gastroenterol 39:743–747. https://doi.org/10.1080/00365520410003272
Wells G, Shea B, O’Connell D et al (2021) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 5 July 2022.
Granlund J, Svensson T, Granath F et al (2011) Diverticular disease and the risk of colon cancer - a population-based case-control study. Aliment Pharmacol Ther 34:675–681. https://doi.org/10.1111/j.1365-2036.2011.04782.x
Diaz JJT, Asenjo BA, Soriano MR, Fernández CJ, Aurusa JOS, Rentería JPBH (2020) Efficacy of colonoscopy after an episode of acute diverticulitis and risk of colorectal cancer. Ann Gastroenterol 33:68–72. https://doi.org/10.20524/aog.2019.0437
Lam TJ, Meurs-Szojda MM, Gundlach L et al (2010) There is no increased risk for colorectal cancer and adenomas in patients with diverticulitis: a retrospective longitudinal study. Colorectal Dis 12:1122–1126. https://doi.org/10.1111/j.1463-1318.2009.01992.x
Elmi A, Hedgire SS, Pargaonkar V, Cao K, McDermott S, Harisinghani M (2013) Is early colonoscopy beneficial in patients with CT-diagnosed diverticulitis? Am J Roentgenol 200:1269–1274. https://doi.org/10.2214/AJR.12.9539
Schmilovitz-Weiss H, Yalunin E, Boaz M et al (2012) Does a colonoscopy after acute diverticulitis affect its management?: a single center experience. J Clin Gastroenterol 46:317–320. https://doi.org/10.1097/MCG.0b013e31823a43a1
White SI, Frenkiel B, Martin PJ (2010) A ten-year audit of perforated sigmoid diverticulitis: highlighting the outcomes of laparoscopic lavage. Dis Colon Rectum 53:1537–1541. https://doi.org/10.1007/DCR.0b013e3181f2ee2a
Huang WY, Lin CC, Jen YM et al (2014) Association between colonic diverticular disease and colorectal cancer: a nationwide population-based study. Clin Gastroenterol Hepatol 12:1288–1294. https://doi.org/10.1016/j.cgh.2013.11.039
Kim MJ, Woo YS, Kim ER et al (2014) Is colonoscopy necessary after computed tomography diagnosis of acute diverticulitis? Intest Res 12:221–228. https://doi.org/10.5217/ir.2014.12.3.221
Fenger C, Nyholm K, Amdrup E (1969) Diverticulitis of the colon. Acta Chir Scand 396:114–120
Horesh N, Saeed Y, Horesh H et al (2016) Colonoscopy after the first episode of acute diverticulitis: challenging management paradigms. Tech Coloproctol 20:383–387. https://doi.org/10.1007/s10151-016-1478-7
Mennini FS, Sciattella P, Marcellusi A, Toraldo B, Koch M (2017) Economic burden of diverticular disease: an observational analysis based on real world data from an Italian region. Dig Liver Dis 49:1003–1008. https://doi.org/10.1016/j.dld.2017.05.024
de Vries HS, Boerma D, Timmer R, van Ramshorst B, Dieleman LA, van Westreenen HL (2014) Routine colonoscopy is not required in uncomplicated diverticulitis: a systematic review. Surg Endosc 28:2039–2047. https://doi.org/10.1007/s00464-014-3447-4
Sharma PV, Eglinton T, Hider P, Frizelle F (2014) Systematic review and meta-analysis of the role of routine colonic evaluation after radiologically confirmed acute diverticulitis. Ann Surg 259:263–272. https://doi.org/10.1097/SLA.0000000000000294
Rottier SJ, van Dijk ST, van Geloven AAW et al (2019) Meta-analysis of the role of colonoscopy after an episode of left-sided acute diverticulitis. Br J Surg 106:988–997. https://doi.org/10.1002/bjs.11191
Almadi MA, Alharbi O, Azzam N, Wadera J, Sadaf N, Aljebreen AM (2014) Prevalence and characteristics of colonic polyps and adenomas in 2654 colonoscopies in Saudi Arabia. Saudi J Gastroenterol 20:154–161. https://doi.org/10.4103/1319-3767.132986
Siripongpreeda B, Mahidol C, Dusitanond N et al (2016) High prevalence of advanced colorectal neoplasia in the Thai population: a prospective screening colonoscopy of 1,404 cases. BMC Gastroenterol 16:101. https://doi.org/10.1186/s12876-016-0526-0
Jackson CS, Vega KJ (2015) Higher prevalence of proximal colon polyps and villous histology in African-Americans undergoing colonoscopy at a single equal access center. J Gastrointest Oncol 6:638–643. https://doi.org/10.3978/j.issn.2078-6891.2015.096
Galetin T, Galetin A, Vestweber KH, Rink AD (2018) Systematic review and comparison of national and international guidelines on diverticular disease. Int J Colorectal Dis 33:261–272. https://doi.org/10.1007/s00384-017-2960-z
Nagata N, Ishii N, Manabe N et al (2019) Guidelines for colonic diverticular bleeding and colonic diverticulitis: Japan Gastroenterological Association. Digestion 99(Suppl 1):1–26. https://doi.org/10.1159/000495282
Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, Støvring J, Danish Surgical Society (2012) Danish national guidelines for treatment of diverticular disease. Dan Med J59:C4453
Stollman N, Smalley W, Hirano I, Institute Clinical Guidelines Committee AGA (2015) American Gastroenterological Association Institute guideline on the management of acute diverticulitis. Gastroenterology 149:1944–1949. https://doi.org/10.1053/j.gastro.2015.10.003
Acknowledgements
We want to thank Dr. Nir Horesh for providing additional information from his research, making it possible to include his article in this review.
Funding
LQM received funding for this study from Knud & Edith Eriksen’s Mindefond (grant number 62786–2020), A.P. Møller Fonden (grant number 20-L-0200), and Aage & Johanne Louis-Hansens Fond (grant number 20-2B-7108).
Author information
Authors and Affiliations
Contributions
All authors contributed to conception and design. LQM performed the literature search. LQM and JB performed the screening of records. LQM performed data analysis. All authors contributed to the interpretation of the data. LQM made first draft of the article. All authors performed critical revision of the article for important intellectual content and have given final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The protocol for this review is published in PROSPERO (CRD42020191055).
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mortensen, L.Q., Buciek, J., Andresen, K. et al. Diverticulitis does not increase the long-term risk of developing colon cancer: a systematic review and meta-analysis. Int J Colorectal Dis 37, 1945–1952 (2022). https://doi.org/10.1007/s00384-022-04246-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04246-z