Abstract
Introduction
Intra-abdominal abscesses complicating Crohn’s disease (CD) present an additional challenge as their presence can contraindicate immunosuppressive treatment whilst emergency surgery is associated with high stoma rate and complications. Treatment options include a conservative approach, percutaneous drainage, and surgical intervention. The current multicentre study audited the short-term outcomes of patients who underwent preoperative radiological drainage of intra-abdominal abscesses up to 6 weeks prior to surgery for ileocolonic CD.
Methods
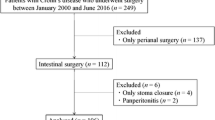
This is a retrospective, multicentre, observational study promoted by the Italian Society of Colorectal Surgery (SICCR), including all adults undergoing ileocolic resection for primary or recurrent CD from June 2018 to May 2019. The outcomes of patients who underwent radiological guided drainage prior to ileocolonic resection were compared to the patients who did not require preoperative drainage. Postoperative morbidity within 30 days of surgery was the primary endpoint. Postoperative length of hospital stay (LOS) and anastomotic leak rate were the secondary outcomes.
Results
Amongst a group of 575 included patients who had an ileocolic resection for CD, there were 36 patients (6.2%) who underwent abscess drainage prior to surgery. Postoperative morbidity (44.4%) and anastomotic leak (11.1%) were significantly higher in the group of patients who underwent preoperative drainage.
Conclusions
Patients with Crohn’s disease who require preoperative radiological guided drainage of intra-abdominal abscesses are at increased risk of postoperative morbidity and septic complications following ileocaecal or re-do ileocolic resection.
Similar content being viewed by others
Introduction
Complications of Crohn’s disease (CD) such as obstruction, fistulae, and abscesses represent a common indication for surgical treatment. Intra-abdominal abscesses in patients with CD can be intraperitoneal, retroperitoneal, or intra-mesenteric and typically result from a perforation [1, 2]. Abscesses, or collections, present an additional challenge in the management of active CD as their presence can contraindicate immunosuppressive treatment.
Treatment options in cases of intra-abdominal collections include a conservative approach with percutaneous drainage and antimicrobial therapy or surgical intervention. Nonetheless, the perioperative morbidity associated with surgical resection during the acute stage of sepsis suggests that, when possible, percutaneous drainage should be attempted first [3].
The Italian Society of Colorectal Surgery (SICCR) recently reported the results of a national multicentre study collecting benchmark data on surgical treatment of CD, highlighting significant variations in practice [4]. The current study audited the short-term outcomes of patients who underwent preoperative radiological drainage of intra-abdominal abscesses up to 6 weeks prior to surgery for ileocolonic CD.
Methods
Study settings
The SICCR promoted the snapshot study “Current Status of Crohn’s Disease Surgery”, which is a retrospective, multicentre, observational study. A steering committee developed the study protocol following the STROBE checklist [5], and this was reviewed independently by the research board of the SICCR. Ethical approval was obtained from the promoting centres and every participating hospital had a named principal investigator, liaising with the local ethics committee. Obtaining informed consent from the patients was deemed not necessary by the Ethics Committees in view of the retrospective and observational nature of the study. Participating centres were invited directly and by an open call published on the SICCR website and disseminated during a 2-month period via the society newsletter.
Eligibility criteria
All patients (aged 16 or older), undergoing elective or emergency ileocolic resection for primary or recurrent CD from 1 June 2018 to 31 May 2019, were eligible for participation in the study. Patients undergoing proctocolectomy, proctectomy, or segmental colectomy were excluded. Indication for surgery included limited terminal ileal disease, CD refractory to medical treatment, obstruction, internal fistulae, and abscesses.
Study objectives
The outcomes of patients who underwent radiological guided drainage for ileocolonic CD complicated by intra-abdominal abscess followed by ileocaecal or ileocolonic resection were extracted from the study population including all patients who underwent surgery for ileocolonic CD within the 12-month study period. Postoperative morbidity within 30 days of surgery was the primary endpoint. Postoperative length of hospital stay (LOS) and anastomotic leak rate were the secondary outcomes.
Data collection
Collected data included the following: patients’ demographics, Montreal classification, preoperative medical treatment and indication for surgery, American Society of Anaesthesiologists (ASA) grade, operative details, surgical access and conversion rate, length of hospital stay, 30-day postoperative morbidity, readmissions, and reoperations.
Postoperative morbidity was defined as any complication occurring during the hospital stay or within 30 days after surgery, whilst all readmissions were recorded up to 30 days after discharge.
Statistical analysis
Categorical variables are presented as frequency and percentages and were compared using the chi-square test or Fisher’s exact test, as appropriate. Continuous variables are presented as median (interquartile range) according to their distribution and were compared with the use of the Mann–Whitney U test. To identify variables associated with binary outcomes, uni- and multivariable logistic regression analyses were performed. Variables having a p value equal to 0.10 or less at the univariable analysis were included in the multivariable model. The odds ratio (ORs) with a 95% confidence interval (CI) was estimated as a measure of association. All reported p values were two-tailed, and p values of less than 0.05 were statistically significant. Statistical analysis was performed by using R version 3.6.1 (2019, The R Foundation for Statistical Computing).
Results
A total of 575 patients were included, and 36 patients (6.2%) underwent abscess drainage prior to surgery. Patients’ details are reported in Table 1.
Overall morbidity and anastomotic leak rate
Postoperative morbidity was 44.4% in the group of patients who underwent preoperative abscess drainage, with a wound infection rate of 8.3% and anastomotic leak rate of 11.1%. Amongst the entire study population, 142 patients had postoperative complications (24.6%), with postoperative morbidity and septic complications being significantly higher in the group of patients who underwent preoperative drainage, as shown in Table 2.
Risk factors for morbidity and anastomotic leak are evaluated in Tables 3 and 4.
LOS, readmissions, and reoperations
The median LOS was 7 days (range 3–95) and factors associated with LOS are reported in Table 5. The reoperation rate and readmission rate in the patients who underwent preoperative abscess drainage were 19.4% and 13.9%, respectively.
Longer LOS, higher readmissions, and reoperation rates were reported in patients who underwent preoperative abscess drainage.
Discussion
Patients with CD who require preoperative radiological guided drainage of intra-abdominal abscesses are at increased risk of postoperative morbidity and septic complications following ileocaecal or re-do ileocolic resection. The reason for this reported higher risk of short-term morbidity in this group of patients compared to patients with a fibro stenotic phenotype of CD is likely multifactorial. Penetrating CD poses additional challenges to the surgeons who might need to perform additional resections or repairs on the “target” organs of the fistulating disease. Secondly, the previous admission and treatment for sepsis suggest a more deconditioned patient, likely more prone to postoperative complications, in view of possible malnutrition or extensive inflammatory disease. Not surprisingly, the group of patients requiring abscess drainage prior to surgery demonstrated a higher rate of recurrent disease, penetrating disease, and need for preoperative total parenteral nutrition (TPN), implying a selection of patients with several risk factors for postoperative complications in this group.
Incomplete percutaneous drainage and non-resolution of the intra-abdominal sepsis can affect not only the risk of postoperative abscess recurrence, but also increased postoperative morbidity, and we hope our results could generate discussion on the need for repeated cross-sectional imaging post percutaneous drainage, even if our results did not provide information on the exact dimension of the abscess prior to drainage.
Patients with CD require a multidisciplinary approach [6] for an essential close and structured integration of medical and surgical management to identify the right time for surgery with the aim to prevent emergency surgery, postoperative complications, and recurrence. It is a quality requirement that patients having surgery for IBD have it undertaken by a colorectal surgeon who is a core member of the IBD multidisciplinary team [7] auditing stoma rate, complications, re-interventions, and mortality [8].
The management of intraabdominal or pelvic abscesses usually involves a combination of medical therapy with either percutaneous or surgical drainage. Medical therapy with antibiotics against enteric flora should be initiated and continued after drainage, with the duration dictated by the completeness of the drainage and the subsequent clinical response [9]. When CD patients present with an intra-abdominal abscess resulting from a contained perforation, although resection can theoretically be done as 1 stage with primary anastomosis, this is often not possible in the emergency setting, in view of the high risk of postoperative complications such as anastomotic leak, wound infection, and fistulisation. Complications are also increased when malnutrition, active disease, and/or sepsis coexist [10]. Percutaneous drainage is therefore particularly appealing as a "bridge" to elective surgical intervention allowing for stabilization and optimization with improved outcomes. Retrospective data have shown that primary percutaneous drainage is associated with significantly fewer complications, higher likelihood of successful primary anastomosis, and shorter length of stay [11, 12]. Nevertheless, our study reported a 44.4% 30-day morbidity in patients with CD undergoing surgical resection within 6 weeks of percutaneous drainage of an intra-abdominal abscess, with an 11% anastomotic leak rate and a 19% reoperation rate.
Our study did not evaluate the time gap between drainage and surgery, and no details were collected on abscess’ size. According to Feagins et al. [9], non-drainable abscesses smaller than 3 cm in size with no evidence of fistula and no steroid therapy are likely to respond to antibiotic therapy alone, despite high recurrence rates. Another limitation of our study is the retrospective design and self-reporting nature of the data collection.
Percutaneous drainage can prevent the need for surgery in up to 30% of selected CD patients with the use of anti-tumor necrosis factor agents being associated with the higher success of conservative management [13], once sepsis had resolved [14], but our study cannot provide guidance on the outcomes of patient who did not require surgery following drainage, as these have not been captured. A recent multicentre study including 335 CD patients with percutaneous drainage followed by surgery [15] reported a complication rate of 32.2%, with residual abscess, low serum albumin concentration [16], and an interval of less than 2 weeks between drainage and surgery, being associated with higher risk of complications. It is important to note that a 25% abscess persistence rate has been reported at surgery after the resolution of the acute episode with percutaneous drainage [17], and this should reiterate the need for re-imaging in patients where planned surgical treatment is avoided.
Conclusions
Percutaneous drainage is a valid treatment option as a bridge to surgery in patients with CD complicated by intra-abdominal abscess. Despite percutaneous drainage, surgical treatment maintains a high risk of morbidity and septic complications.
References
Maaser C, Sturm A, Vavricka SR, Kucharzik T, Fiorino G, Annese V, Calabrese E, Baumgart DC, Bettenworth D, Borralho Nunes P, Burisch J, Castiglione F, Eliakim R, Ellul P, González-Lama Y, Gordon H, Halligan S, Katsanos K, Kopylov U, Kotze PG, Krustinš E, Laghi A, Limdi JK, Rieder F, Rimola J, Taylor SA, Tolan D, van Rheenen P, Verstockt B, Stoker J (2019) European Crohn’s and Colitis Organisation [ECCO] and the European Society of Gastrointestinal and Abdominal Radiology [ESGAR] ECCO-ESGAR guideline for diagnostic assessment in IBD part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis 13(2):144–164. https://doi.org/10.1093/ecco-jcc/jjy113
Yamaguchi A, Matsui T, Sakurai T, Ueki T, Nakabayashi S, Yao T, Futami K, Arima S, Ono H (2004) The clinical characteristics and out- come of intraabdominal abscess in Crohn’s disease. J Gastroenterol 39:441–448. https://doi.org/10.1007/s00535-003-1409-z
He X, Lin X, Lian L, Huang J, Yao Q, Chen Z, Fan D, Wu X, Lan P (2015) Preoperative percutaneous drainage of spontaneous intra-abdominal abscess in patients with Crohn’s disease: a meta-analysis. J Clin Gastroenterol 49(9):e82-90
SICCR Current Status of Crohn’s Disease Surgery Collaborative (2020) National variations in perioperative assessment and surgical management of Crohn’s disease: a multicentre study. Colorectal Dis. Online ahead of print. https://doi.org/10.1111/codi.15334
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2008) STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–9
IBD Standards Group (2013) Standards for the healthcare of people who have inflammatory bowel disease [IBD]. 2013 update. St Albans, UK: Oyster Healthcare Communications
NICE Quality Standard [QS81]—Inflammatory bowel disease. Published 6 February 2015. Last accessed 7/1/2022 http://www.nice.org.uk/guidance/qs81/chapter/quality-statement-2-multidisciplinary-team-support
Calvet X, Panes J, Alfaro N et al (2014) Delphi consensus statement: quality indicators for inflammatory bowel disease comprehensive care units. J Crohns Colitis 8:240–251
Feagins LA, Holubar SD, Kane SV, Spechler SJ (2011) Current strategies in the management of intra-abdominal abscesses in Crohn’s disease. Clin Gastroenterol Hepatol 9:842–850. https://doi.org/10.1016/j.cgh.2011.04.023
Caiazzo A, Flashman K, Celentano V (2020) Increased postoperative use of computed tomography following emergency surgery for ileocaecal Crohn disease. Surg Laparosc Endosc Percutan Tech 30(3):214–217
Xie Y, Zhu W, Li N et al (2012) The outcome of initial percutaneous drainage versus surgical drainage for intra-abdominal abscesses in Crohn’s disease. Int J Colorectal Dis 27:199–206
Zerbib P, Koriche D, Truant S et al (2010) Pre-operative management is associated with low rate of post-operative morbidity in penetrating Crohn’s disease. Aliment Pharmacol Ther 32:459–465
Waked B, Holvoet T, Geldof J, Baert F, Pattyn P, Lobatón T, Hindryckx P (2021) Conservative management of spontaneous intra-abdominal abscess in Crohn’s disease: outcome and prognostic factors. J Dig Dis 22(5):263–270
Clancy C, Boland T, Deasy J, McNamara D, Burke JP (2016) A Meta-analysis of percutaneous drainage versus surgery as the initial treatment of Crohn’s disease-related intra-abdominal abscess. J Crohns Colitis 10(2):202–208
El-Hussuna A, Karer MLM, Uldall Nielsen NN, Mujukian A, Fleshner PR, Iesalnieks I, Horesh N, Kopylov U, Jacoby H, Al-Qaisi HM, Colombo F, Sampietro GM, Marino MV, Ellebæk M, Steenholdt C, Sørensen N, Celentano V, Ladwa N, Warusavitarne J, Pellino G, Zeb A, Di Candido F, Hurtado-Pardo L, Frasson M, Kunovsky L, Yalcinkaya A, Tatar OC, Alonso S, Pera M, Granero AG, Rodríguez CA, Minaya A, Spinelli A, Qvist N (2021) Postoperative complications and waiting time for surgical intervention after radiologically guided drainage of intra-abdominal abscess in patients with Crohn’s disease. BJS Open 5(5):zrab075. https://doi.org/10.1093/bjsopen/zrab075
Ghoneima AS, Flashman K, Dawe V, Baldwin E, Celentano V (2019) High risk of septic complications following surgery for Crohn’s disease in patients with preoperative anaemia, hypoalbuminemia and high CRP. Int J Colorectal Dis 34(12):2185–2188
Collard MK, Benoist S, Maggiori L, Zerbib P, Lefevre JH, Denost Q, Germain A, Cotte E, Beyer-Berjot L, Corté H, Desfourneaux V, Rahili A, Duffas JP, Pautrat K, Denet C, Bridoux V, Meurette G, Faucheron JL, Loriau J, Souche R, Vicaut E, Panis Y, Brouquet A (2021) A reappraisal of outcome of elective surgery after successful non-operative management of an intra-abdominal abscess complicating ileocolonic Crohn’s disease: a subgroup analysis of a nationwide prospective cohort. J Crohns Colitis 15(3):409–418
Author information
Authors and Affiliations
Consortia
Contributions
Valerio Celentano: study lead, study design, data collection, and draft manuscript. Mariano Giglio: data collection and data analysis. Gianluca Pellino: study design and manuscript review. Matteo Rottoli: data analysis and manuscript review. Gianluca Sampietro: data collection, data analysis, and manuscript review. Antonino Spinelli: study design and draft manuscript. Francesco Selvaggi: study design, data analysis, and manuscript review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authorship: all authors of the SICCR Current status of Crohn’s disease surgery Collaborative are to be listed as PubMed indexed authors as in Appendix 1. Specification of authors’ contribution is detailed in Appendix 2.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Celentano, V., Giglio, M.C., Pellino, G. et al. High complication rate in Crohn’s disease surgery following percutaneous drainage of intra-abdominal abscess: a multicentre study. Int J Colorectal Dis 37, 1421–1428 (2022). https://doi.org/10.1007/s00384-022-04183-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04183-x