Abstract
Purpose
To identify risk factors for delayed oral nutrition in infants with a congenital diaphragmatic hernia (CDH) and its impact on developmental delay at 18 months of age.
Methods
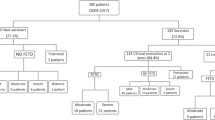
This retrospective single-center cohort study compared the clinical parameters in patients with isolated CDH born and treated at our hospital between 2006 and 2020. We evaluated clinical features significantly related to delayed oral nutrition (defined as taking ≥ 30 days from weaning from mechanical ventilation to weaning from tube feeding).
Results
Twenty-six of the 80 cases had delayed oral nutrition. Univariate analyses showed significant differences. Multivariate analyses were performed on the three items of preterm delivery, defect size (over 50% to nearly entire defect), and ventilation for ≥ 9 days. We identified the latter two items as independent risk factors. The adjusted odds ratios were 4.65 (95% confidence interval, 1.27–7.03) and 6.02 (1.65–21.90), respectively. Delayed oral nutrition was related to a significantly higher probability of developmental delay at 18 months (crude odds ratio 4.16, 1.19–14.5).
Conclusion
In patients with CDH, a large defect and ventilatory management over 9 days are independent risk factors for delayed oral nutrition, which is a potent predictor of developmental delay that requires active developmental care.
Similar content being viewed by others
Data availability
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
References
Wenstrom KD, Weiner CP, Hanson JW (1991) A five-year statewide experience with congenital diaphragmatic hernia. Am J Obstet Gynecol 165:838–842. https://doi.org/10.1016/0002-9378(91)90425-Q
Langham MR, Kays DW, Ledbetter DJ et al (1996) Congenital diaphragmatic hernia: epidemiology and outcome. Clin Perinatol 23:671–688. https://doi.org/10.1016/s0095-5108(18)30201-x
Jaillard SM, Pierrat V, Dubois A et al (2003) Outcome at 2 years of infants with congenital diaphragmatic hernia: a population-based study. Ann Thorac Surg 75:250–256. https://doi.org/10.1016/S0003-4975(02)04278-9
Muratore CS, Utter S, Jaksic T, Lund DP, Wilson JM (2001) Nutritional morbidity in survivors of congenital diaphragmatic hernia. J Pediatr Surg 36:1171–1176. https://doi.org/10.1053/jpsu.2001.25746
Cordier AG, Laup L, Letourneau A et al (2021) Prenatal stomach position predicts gastrointestinal morbidity at 2 years in fetuses with left-sided congenital diaphragmatic hernia. Ultrasound Obstet Gynecol 57:959–967. https://doi.org/10.1002/uog.22086
Krom H, de Winter JP, Kindermann A (2017) Development, prevention, and treatment of feeding tube dependency. Eur J Pediatr 176:683–688. https://doi.org/10.1007/s00431-017-2908-x
Schauster H, Dwyer J (1996) Transition from tube feedings to feedings by mouth in children: Preventing eating dysfunction. J Am Diet Assoc 96:277–281. https://doi.org/10.1016/S0002-8223(96)00081-8
Dunitz-Scheer M, Marinschek S, Beckenbach H et al (2011) Tube dependence: a reactive eating behavior disorder. Infant Child Adolesc Nutr 3:209–215. https://doi.org/10.1177/1941406411416359
Dunitz-Scheer M, Levine A, Roth Y et al (2009) Prevention and treatment of tube dependency in infancy and early childhood. Infant Child Adolesc Nutr 1:73–82. https://doi.org/10.1177/1941406409333988
Chatoor I, Ganiban J, Hirsch R, Borman-Spurrell E, Mrazek DA (2000) Maternal characteristics and toddler temperament in infantile anorexia. J Am Acad Child Adolesc Psychiatry 39:743–751. https://doi.org/10.1097/00004583-200006000-00013
Terui K, Nagata K, Kanamori Y et al (2017) Risk stratification for congenital diaphragmatic hernia by factors within 24 h after birth. J Perinatol 37:805–808. https://doi.org/10.1038/jp.2017.11
Tsao K, Lally KP (2008) The congenital diaphragmatic hernia study group: a voluntary international registry. Semin Pediatr Surg 17:90–97. https://doi.org/10.1053/j.sempedsurg.2008.02.004
Lally KP, Lasky RE, Lally PA et al (2013) Standardized reporting for congenital diaphragmatic hernia - An international consensus. J Pediatr Surg 48:2408–2415. https://doi.org/10.1016/j.jpedsurg.2013.08.014
McGahren ED, Mallik K, Rodgers BM (1997) Neurological outcome is diminished in survivors of congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation. J Pediatr Surg 32:1216–1220. https://doi.org/10.1016/s0022-3468(97)90685-0
D’Agostino JA, Bernbaum JC, Gerdes M et al (1995) Outcome for infants with congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: the first year. J Pediatr Surg 30:10–15. https://doi.org/10.1016/0022-3468(95)90598-7
Antiel RM, Lin N, Licht DJ et al (2017) Growth trajectory and neurodevelopmental outcome in infants with congenital diaphragmatic hernia. J Pediatr Surg 52:1944–1948. https://doi.org/10.1016/j.jpedsurg.2017.08.063
Bevilacqua F, Morini F, Zaccara A et al (2017) Does ventilatory time retain its validity in predicting neurodevelopmental outcome at two years of age in high-risk congenital diaphragmatic hernia survivors? Am J Perinatol 34:248–252. https://doi.org/10.1055/s-0036-1586120
Danzer E, Gerdes M, Bernbaum J et al (2010) Neurodevelopmental outcome of infants with congenital diaphragmatic hernia prospectively enrolled in an interdisciplinary follow-up program. J Pediatr Surg 45:1759–1766. https://doi.org/10.1016/j.jpedsurg.2010.03.011
Kono Y, Yonemoto N, Kusuda S et al (2016) Developmental assessment of VLBW infants at 18 months of age: a comparison study between KSPD and Bayley III. Brain Dev 38:377–385. https://doi.org/10.1016/j.braindev.2015.10.010
Benjamin JR, Gustafson KE, Smith PB et al (2013) Perinatal factors associated with poor neurocognitive outcome in early school age congenital diaphragmatic hernia survivors. J Pediatr Surg 48:730–737. https://doi.org/10.1016/j.jpedsurg.2012.09.026
Goldstein SA, Watkins KJ, Lowery RE et al (2022) Oral aversion in infants with congenital heart disease: a single-center retrospective cohort study. Pediatr Crit Care Med 23:e171–e179. https://doi.org/10.1097/PCC.0000000000002879
Levine A, Bachar L, Tsangen Z et al (2011) Screening criteria for diagnosis of infantile feeding disorders as a cause of poor feeding or food refusal. J Pediatr Gastroenterol Nutr 52:563–568. https://doi.org/10.1097/MPG.0b013e3181ff72d2
Einarson KD, Arthur HM (2003) Predictors of oral feeding difficulty in cardiac surgical infants. Pediatr Nurs 29:315–319
Kohr LM, Dargan M, Hague A et al (2003) The incidence of dysphagia in pediatric patients after open heart procedures with transesophageal echocardiography. Ann Thorac Surg 76:1450–1456. https://doi.org/10.1016/S0003-4975(03)00956-1
Kogon BE, Ramaswamy V, Todd K et al (2007) Feeding difficulty in newborns following congenital heart surgery. Congenit Heart Dis 2:332–337. https://doi.org/10.1111/j.1747-0803.2007.00121.x
Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJ (2002) Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. JAMA 288:728–737. https://doi.org/10.1001/jama.288.6.728
Spittle AJ, Orton J (2014) Cerebral palsy and developmental coordination disorder in children born preterm. Semin Fetal Neonatal Med 19:84–89. https://doi.org/10.1016/j.siny.2013.11.005
Engle WA, Tomashek KM, Wallman C, Committee on Fetus and Newborn, American Academy of Pediatrics (2007) ‘Late-preterm’ infants: a population at risk. Pediatrics 120:1390–1401. https://doi.org/10.1542/peds.2007-2952
Guglielmetti LC, Estrada AE, Phillips R et al (2020) Congenital diaphragmatic hernias: Severe defect grade predicts the need for fundoplication. Med 99:e23383. https://doi.org/10.1097/MD.0000000000023383
Wynn J, Aspelund G, Zygmunt A et al (2013) Developmental outcomes of children with congenital diaphragmatic hernia: a multicenter prospective study. J Pediatr Surg 48:1995–2004. https://doi.org/10.1016/j.jpedsurg.2013.02.041
Haliburton B, Chiang M, Marcon M et al (2016) Nutritional intake, energy expenditure, and growth of infants following congenital diaphragmatic hernia repair. J Pediatr Gastroenterol Nutr 62:474–478. https://doi.org/10.1097/MPG.0000000000001000
Terui K, Tazuke Y, Nagata K et al (2021) Weight gain velocity and adequate amount of nutrition for infants with congenital diaphragmatic hernia. Pediatr Surg Int 37:205–212. https://doi.org/10.1007/s00383-020-04785-y
Edwards S, Davis AMG, Ernst L et al (2015) Interdisciplinary strategies for treating oral aversions in children. JPEN J Parenter Enteral Nutr 39:899–909. https://doi.org/10.1177/0148607115609311
Arcos-Machancoses JV, Ruiz Hernández C, Martin De Carpi J, Pinillos Pisón S (2018) A systematic review with meta-analysis of the prevalence of gastroesophageal reflux in congenital diaphragmatic hernia pediatric survivors. Dis Esophagus. https://doi.org/10.1093/dote/dox158
Lally KP, Lally PA, Van Meurs KP et al (2006) Treatment evolution in high-risk congenital diaphragmatic hernia: ten years’ experience with diaphragmatic agenesis. Ann Surg 244:505–513. https://doi.org/10.1097/01.sla.0000239027.61651.fa
Nagata K, Usui N, Kanamori Y et al (2013) The current profile and outcome of congenital diaphragmatic hernia: a nationwide survey in Japan. J Pediatr Surg 48:738–744. https://doi.org/10.1016/j.jpedsurg.2012.12.017
Greene Z, O’Donnell CPF, Walshe M (2016) Oral stimulation for promoting oral feeding in preterm infants. Cochrane Database Syst Rev 9:CD009720. https://doi.org/10.1002/14651858.CD009720.pub2
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by all authors. The first draft of the manuscript was written by TY. The draft was reviewed and edited by Noriaki Usui, and all authors commented on the second version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamamichi, T., Imanishi, Y., Sakai, T. et al. Risk factors for and developmental relation of delayed oral nutrition in infants with congenital diaphragmatic hernia. Pediatr Surg Int 40, 2 (2024). https://doi.org/10.1007/s00383-023-05595-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05595-8