Abstract
Purpose
Postoperative adhesive bowel obstruction (ABO) is a common complication especially in complicated appendicitis. This study aimed to analyze the risk factors for ABO following appendectomy in children with complicated appendicitis, and establish a scoring model for predicting postoperative ABO and treatment option to relieve the obstruction.
Methods
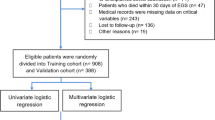
From December 2014 to January 2020, all files of consecutive patients with complicated appendicitis underwent appendectomy were reviewed. Univariate and multivariate analyses were used to screen out the risk factors of postoperative ABO, and establish a scoring model for predicting postoperative ABO and surgical relief to relieve the obstruction.
Results
Of the 780 patients, 87 (11.2%) had ABO following appendectomy, including 27 who underwent surgical relief. Age ≤ 6 years, overweight and obesity, duration of symptoms ≥ 36 h, C-reactive protein ≥ 99 mg/L, duration of operation ≥ 60 min, intraoperative peritoneal lavage, and postoperative flatus time ≥ 20 h were independent risk factors for postoperative ABO. The final scoring model for postoperative ABO included factors above, and exhibited a high degree of discrimination (area under the curve [AUC]: 0.937; 95% confidence interval [CI] 0.913–0.960) corresponding to an optimal cut-off value of 6: 82.8% sensitivity, 92.6% specificity. Furthermore, the scoring model showed a sensitivity of 74.1% and a specificity of 91.7% for patients wo underwent surgical relief to relieve obstruction with the optimal cut-off value of 9.
Conclusion
Risk factors for postoperative ABO should be taken seriously in children with complicated appendicitis. The scoring model is a novel but promising method to predict postoperative ABO and provide reference for clinical decision-making to relieve the obstruction.





Similar content being viewed by others
References
Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175:185–190. https://doi.org/10.1016/j.jss.2011.07.017
Almström M, Svensson JF, Svenningsson A, Hagel E, Wester T (2019) Population-based cohort study of the correlation between provision of care and the risk for complications after appendectomy in children. J Pediatr Surg 54:2279–2284. https://doi.org/10.1016/j.jpedsurg.2019.03.013
Ming PC, Yan TY, Tat LH (2009) Risk factors of postoperative infections in adults with complicated appendicitis. Surg Laparosc Endosc Percutan Tech 19:244–248. https://doi.org/10.1097/SLE.0b013e3181a4cda2
de Wijkerslooth EML, van den Boom AL, Wijnhoven BPL (2019) Variation in classification and postoperative management of complex appendicitis: a European survey. World J Surg 43:439–446. https://doi.org/10.1007/s00268-018-4806-4
Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T et al (2015) Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 313:2340–2348. https://doi.org/10.1001/jama.2015.6154
Duron JJ, Silva NJ, du Montcel ST, Berger A, Muscari F, Hennet H et al (2006) Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg 244:750–757. https://doi.org/10.1097/01.sla.0000225097.60142.68
Lautz TB, Raval MV, Reynolds M, Barsness KA (2011) Adhesive small bowel obstruction in children and adolescents: operative utilization and factors associated with bowel loss. J Am Coll Surg 212:855–861. https://doi.org/10.1016/j.jamcollsurg.2011.01.061
Bracho-Blanchet E, Dominguez-Muñoz A, Fernandez-Portilla E, Zalles-Vidal C, Davila-Perez R (2017) Predictive value of procalcitonin for intestinal ischemia and/or necrosis in pediatric patients with adhesive small bowel obstruction (ASBO). J Pediatr Surg 52:1616–1620. https://doi.org/10.1016/j.jpedsurg.2017.07.006
Li M, Zhu W, Li Y, Jiang J, Li J, Li N (2014) Long intestinal tube splinting prevents postoperative adhesive small-bowel obstruction in sclerosing encapsulating peritonitis. BMC Gastroenterol 14:180. https://doi.org/10.1186/1471-230X-14-180
Menzies D, Ellis H (1990) Intestinal obstruction from adhesions—how big is the problem? Ann R Coll Surg Engl 72:60–63
Vrijland WW, Jeekel J, van Geldorp HJ, Swank DJ, Bonjer HJ (2003) Abdominal adhesions: intestinal obstruction, pain, and infertility. Surg Endosc 17:1017–1022. https://doi.org/10.1007/s00464-002-9208-9
Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, Reijnen MM, Schaapveld M, Van Goor H (2000) Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg 87:467–471. https://doi.org/10.1046/j.1365-2168.2000.01394.x
Fredriksson F, Christofferson RH, Lilja HE (2006) Adhesive small bowel obstruction after laparotomy during infancy. Br J Surg 103:284–289. https://doi.org/10.1002/bjs.10072
Li Y, James C, Byl N, Sessel J, Caird MS, Farley FA et al (2020) Obese children have different forearm fracture characteristics compared with normal-weight children. J Pediatr Orthop 40:e127–e130. https://doi.org/10.1097/BPO.0000000000001402
Michailidou M, Sacco Casamassima MG, Goldstein SD, Gause C, Karim O, Salazar JH et al (2015) The impact of obesity on laparoscopic appendectomy: results from the ACS National Surgical Quality Improvement Program pediatric database. J Pediatr Surg 50:1880–1884. https://doi.org/10.1016/j.jpedsurg.2015.07.005
Feng W, Zhao XF, Li MM, Cui HL (2020) A clinical prediction model for complicated appendicitis in children younger than 5 years of age. BMC Pediatr 20:401. https://doi.org/10.1186/s12887-020-02286-4
Leung TT, Dixon E, Gill M, Mador BD, Moulton KM, Kaplan GG et al (2009) Bowel obstruction following appendectomy: what is the true incidence? Ann Surg 250:51–53. https://doi.org/10.1097/SLA.0b013e3181ad64a7
Nataraja RM, Panabokke G, Chang AD, Mennie N, Tanny ST, Keys C (2019) Does peritoneal lavage influence the rate of complications following pediatric laparoscopic appendicectomy in children with complicated appendicitis? A prospective randomized clinical trial. J Pediatr Surg 54:2524–2527. https://doi.org/10.1016/j.jpedsurg.2019.08.039
Antoniou SA, Antoniou GA, Granderath FA (2015) Risk for bowel obstruction following laparoscopic and open appendectomy. J Gastrointest Surg 19:795–796. https://doi.org/10.1007/s11605-015-2768-5
Ellis H (1982) The causes and prevention of intestinal adhesions. Br J Surg 69:241–243. https://doi.org/10.1002/bjs.1800690502
Andersson RE (2014) Short-term complications and long-term morbidity of laparoscopic and open appendicectomy in a national cohort. Br J Surg 101:1135–1142. https://doi.org/10.1002/bjs.9552
Tseng CJ, Sun DP, Lee IC, Weng SF, Chou CL (2016) Factors associated with small bowel obstruction following appendectomy: a population-based study. Medicine (Baltimore) 95:e3541. https://doi.org/10.1097/MD.0000000000003541
Andersson RE (2001) Small bowel obstruction after appendicectomy. Br J Surg 88:1387–1391. https://doi.org/10.1046/j.0007-1323.2001.01869.x
Angenete E, Jacobsson A, Gellerstedt M, Haglind E (2012) Effect of laparoscopy on the risk of small-bowel obstruction: a population-based register study. Arch Surg 147:359–365. https://doi.org/10.1001/archsurg.2012.31
Kutasy B, Puri P (2013) Appendicitis in obese children. Pediatr Surg Int 29:537–544. https://doi.org/10.1007/s00383-013-3289-5
Garey CL, Laituri CA, Little DC, Ostlie DJ, St Peter SD (2011) Outcomes of perforated appendicitis in obese and nonobese children. J Pediatr Surg 46:2346–2348. https://doi.org/10.1016/j.jpedsurg.2011.09.024
Gates NL, Rampp RD, Koontz CC, Holcombe JM, Bhattacharya SD (2019) Single-incision laparoscopic appendectomy in children and conversion to multiport appendectomy. J Surg Res 235:223–226. https://doi.org/10.1016/j.jss.2018.08.050
Litz CN, Farach SM, Danielson PD, Chandler NM (2016) Obesity and single-incision laparoscopic appendectomy in children. J Surg Res 203:283–286. https://doi.org/10.1016/j.jss.2016.03.039
Cantürk Z, Cantürk NZ, Cetinarslan B, Utkan NZ, Tarkun I (2003) Nosocomial infections and obesity in surgical patients. Obes Res 11:769–775. https://doi.org/10.1038/oby.2003.107
de Jongh RT, Serné EH, IJzerman RG, de Vries G, Stehouwer CD (2004) Impaired microvascular function in obesity: implications for obesity-associated microangiopathy, hypertension, and insulin resistance. Circulation 109:2529–2535. https://doi.org/10.1161/01.CIR.0000129772.26647.6F
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350:g7594. https://doi.org/10.1136/bmj.g7594
Tingstedt B, Isaksson J, Andersson R (2007) Long-term follow-up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br J Surg 94:743–748. https://doi.org/10.1002/bjs.5634
Funding
This study was funded by the Tianjin Science and Technology Plan Project (Grant no. 14RCGFSY00150) for data collection and language polishing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the relevant guidelines and regulations approved by the Institutional Research Ethics Board of Tianjin Children’s Hospital (IRB no. L2020-29) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feng, W., Du, XB., Zhao, XF. et al. Risk factors of postoperative adhesive bowel obstruction in children with complicated appendicitis. Pediatr Surg Int 37, 745–754 (2021). https://doi.org/10.1007/s00383-021-04862-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04862-w