Abstract
Purpose
This study aimed to investigate the clinical features and risk factors of bile duct perforation in pediatric congenital biliary dilatation (CBD) patients.
Methods
CBD patients, whose initial symptom was abdominal pain, were enrolled in this study and were divided into perforated and non-perforated groups. The clinical features of the perforated group were investigated. Moreover, the age at operation, sex, and morphologic features of the extrahepatic bile duct were compared between the groups.
Results
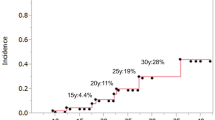
Fifteen cases of bile duct perforation (10.4%) were identified among the 144 CBD patients who had abdominal pain. Majority of bile duct perforation occurred in patients aged < 4 years. The median duration from onset of abdominal pain to bile duct perforation was 6 (4–14) days. Age at onset [< 4 years old; P = 0.02, OR 13.9, (1.663, 115.3)], shape of extrahepatic bile duct [non-cystic type; P = 0.009, OR 8.36, (1.683, 41.5)], and dilatation of the common channel [P = 0.02, OR 13.6, (1.651, 111.5)] were risk factors of bile duct perforation.
Conclusions
Emergent bile duct drainage might be planned to prevent bile duct perforation if CBD patients have the abovementioned risk factors and experience persistent abdominal pain lasting for a few days from onset.



Similar content being viewed by others
References
de Vries JS, de Vries S, Aronson DC, Bosman DK, Rauws EA, Bosma A, Heij HA, Gouma DJ, van Gulik TM (2002) Choledochal cyst: age of presentation, symptoms, and late complications related to Todani’s classification. J Pediatr Surg 37:1568–1573
Todani T, Watanabe Y, Fujii T, Uemura S (1984) Anomalous arrangement of the pancreatobiliary ductal system in patients with acholedochalcyst. Am J Surg 147:672–676
Kaneko K, Ando H, Seo T, Ono Y, Tainaka T, Sumida W (2007) Proteomic analysis of protein plugs: causative agent of symptoms in patients with choledochal cyst. Dig Dis Sci 52:1979–1986
Yamoto M, Urushihara N, Fukumoto K, Miyano G, Nouso H, Morita K, Miyake H, Kaneshiro M, Koyama M (2015) Usefulness of laparoscopic cholecystostomy in children with complicated choledochal cyst. Asian J Endosc Surg 8:153–157
Urushihara N, Todani T, Watanabe Y, Uemura S, Morotomi Y, Wang ZQ (1995) Does hyperamylasemia in choledochal cyst indicate true pancreatitis? An experimental study. Eur J Pediatr Surg 5:139–142
Ando K, Miyano T, Kohno S, Takamizawa S, Lane G (1998) Spontaneous perforation of choledochal cyst: a study of 13 cases. Eur J Pediatr Surg 8:23–25
Karnak I, Tanyel FC, Büyükpamukçu N, Hiçsönmez A (1997) Spontaneous rapture of choledochal cyst: an usual cause of acute abdomen in children. J Pediatr Surg 32:736–738
Wagholikar GD, Chetri K, Yachha SK, Sikora SS (2004) Spontaneous perforation—a rare complication of choledochal cyst. Indian J Gastroenterol 23:111–112
Ando H, Ito T, Watanabe Y, Seo T, Kaneko K, Nagaya M (1995) Spontaneous perforation of choledochal cyst. J Am Coll Surg 181:125–128
Fujishiro J, Masumoto K, Urita Y, Shinkai T, Gotoh C (2013) Pancreatic complication in pediatric choledochal cysts. J Pediatr Surg 48:1897–1902
Yasufuku M, Hisamatsu C, Nozaki N, Nishijima E (2012) A very low-birth weight infant with spontaneous perforation of a choledochal cyst and adjacent pseudocyst formation. J Pediatr Surg 47:e17–e19
Upadhyaya VD, Kumar B, Singh M, Rudramani, Jaiswal S, Lal R, Gambhir S, Rohan M (2013) Spontaneous biliary peritonitis: is bed side diagnosis possible? Afr J Pediatr Surg 10:112–116
Fumino S, Iwai N, Deguchi E, Ono S, Shimadera S, Iwabuchi T, Kinoshita H, Nishimura T (2006) Spontaneous rupture of choledochal cyst with pseudocyst formation-report on 2 cases with literature review. J Pediatr Surg 14:e19–e21
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Informed consent
For this study, informed consent was not required.
Rights and permissions
About this article
Cite this article
Fukuzawa, H., Urushihara, N., Miyakoshi, C. et al. Clinical features and risk factors of bile duct perforation associated with pediatric congenital biliary dilatation. Pediatr Surg Int 34, 1079–1086 (2018). https://doi.org/10.1007/s00383-018-4321-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4321-6