Abstract
Purpose
The optimal method of managing paediatric choledocholithiasis is controversial. Endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy are effective in adults; however, the long-term outcome in the paediatric population is unknown. We report our experience with laparoscopic common bile duct (CBD) exploration to relieve choledocholithiasis in children and propose a management algorithm.
Methods
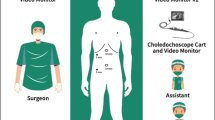
A retrospective chart review of 124 children, who underwent cholecystectomy over 5 years was conducted. Data collected included age at onset, duration of symptoms, length of stay, method of relieving choledocholithiasis and postoperative outcome.
Results
Mean age was 12.5 years (range 10–14 years). 102 cholecystectomies were performed laparoscopically. Following intraoperative cholangiogram (IOC), choledocholithiasis was identified in eight patients. In three cases, the CBD was flushed with normal saline via a 5F ureteral catheter successfully relieving the obstruction. In three cases, a Dormia basket was used to break down the stone. Two cases required postoperative ERCP and sphincterotomy to successfully extract the stones. All children were symptom-free at follow-up with no complications reported to date.
Conclusion
Laparoscopic CBD exploration with Dormia basket or saline flushes to relieve choledocholithiasis is a safe and effective alternative in children. If unsuccessful, ERCP and sphincterotomy can be performed in centres with adequate resources and expertise.


Similar content being viewed by others
References
Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M (2001) Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1, 000 patients. Ann Surg 234(2):210–214
Mah D, Wales P, Njere I, Kortan P, Masiakos P, Kim PC (2004) Management of suspected common bile duct stones in children: role of selective intraoperative cholangiogram and endoscopic retrograde cholangiopancreatography. J Pediatr Surg 39(6):808–812 (S0022346804001022[pii], discussion 808–812)
Shah RS, Blakely ML, Lobe TE (2001) The role of laparoscopy in the management of common bile duct obstruction in children. Surg Endosc 15(11):1353–1355. doi:10.1007/s004640000320
Esposito C, Alicchio F, Giurin I, Perricone F, Ascione G, Settimi A (2009) Lessons learned from the first 109 laparoscopic cholecystectomies performed in a single pediatric surgery center. World J Surg 33(9):1842–1845. doi:10.1007/s00268-009-0129-9
Issa H, Al-Haddad A, Al-Salem AH (2007) Diagnostic and therapeutic ERCP in the pediatric age group. Pediatr Surg Int 23(2):111–116. doi:10.1007/s00383-006-1832-3
Newman KD, Powell DM, Holcomb GW 3rd (1997) The management of choledocholithiasis in children in the era of laparoscopic cholecystectomy. J Pediatr Surg 32(7):1116–1119 (S0022-3468(97)90411-5[pii])
Stromberg C, Luo J, Enochsson L, Arnelo U, Nilsson M (2008) Endoscopic sphincterotomy and risk of malignancy in the bile ducts, liver, and pancreas. Clin Gastroenterol Hepatol 6(9):1049–1053. doi:10.1016/j.cgh.2008.04.016
Sugiyama M, Atomi Y (2002) Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol 97(11):2763–2767. doi:10.1111/j.1572-0241.2002.07019.x
Prasil P, Laberge JM, Barkun A, Flageole H (2001) Endoscopic retrograde cholangiopancreatography in children: a surgeon’s perspective. J Pediatr Surg 36(5):733–735. doi:10.1053/jpsu.2001.22948
Folkers MT, Disario JA, Adler DG (2009) Long-term complications of endoscopic biliary sphincterotomy for choledocholithiasis: a North-American perspective. Am J Gastroenterol 104(11):2868–2869. doi:10.1038/ajg.2009.398
Bonnard A, Seguier-Lipszyc E, Liguory C, Benkerrou M, Garel C, Malbezin S, Aigrain Y, de Lagausie P (2005) Laparoscopic approach as primary treatment of common bile duct stones in children. J Pediatr Surg 40(9):1459–1463. doi:10.1016/j.jpedsurg.2005.05.046
Riciardi R, Islam S, Canete JJ, Arcand PL, Stoker ME (2003) Effectiveness and long-term results of laparoscopic common bile duct exploration. Surg Endosc 17(1):19–22. doi:10.1007/s00464-002-8925-4
Petelin JB (2002) Surgical management of common bile duct stones. Gastrointest Endosc 56(6 Suppl):S183–S189. doi:10.1067/mge.2002.1290131
Tranter SE, Thompson MH (2003) A prospective single-blinded controlled study comparing laparoscopic ultrasound of the common bile duct with operative cholangiography. Surg Endosc 17(2):216–219. doi:10.1007/s00464-002-8911-x
Mattioli G, Pini-Prato A, Castagnetti M, Gandullia P, Toma P, Jasonni V (2007) Is perioperative cholangiography necessary in children undergoing elective laparoscopic cholecystectomy? Eur J Pediatr Surg 17(3):176–179. doi:10.1055/s-2007-965146
Kroh M, Chand B (2008) Choledocholithiasis, endoscopic retrograde cholangiopancreatography, and laparoscopic common bile duct exploration. Surg Clin North Am 88(5):1019–1031 (vii). doi:10.1016/j.suc.2008.05.004
Verbesey JE, Birkett DH (2008) Common bile duct exploration for choledocholithiasis. Surg Clin North Am 88(6):1315–1328 (ix). doi:10.1016/j.suc.2008.08.002
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menon, S., Patel, B., Saekang, E. et al. Laparoscopic exploration of the common bile duct to relieve choledocholithiasis in children. Pediatr Surg Int 27, 537–540 (2011). https://doi.org/10.1007/s00383-010-2826-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-010-2826-8