Abstract
Introduction
Pediatric intracranial aneurysms (IAs) are rare and have distinct clinical profiles compared to adult IAs. They differ in location, size, morphology, presentation, and treatment strategies. We present our experience with pediatric IAs over an 18-year period using surgical and endovascular treatments and review the literature to identify commonalities in epidemiology, treatment, and outcomes.
Methods
We identified all patients < 20 years old who underwent treatment for IAs at our institution between 2005 and 2020. Medical records and imaging were examined for demographic, clinical, and operative data. A systematic review was performed to identify studies reporting primary outcomes of surgical and endovascular treatment of pediatric IAs. Demographic information, aneurysm characteristics, treatment strategies, and outcomes were collected.
Results
Thirty-three patients underwent treatment for 37 aneurysms over 18 years. The mean age was 11.4 years, ranging from one month to 19 years. There were 21 males (63.6%) and 12 females (36.4%), yielding a male: female ratio of 1.75:1. Twenty-six (70.3%) aneurysms arose from the anterior circulation and 11 (29.7%) arose from the posterior circulation. Aneurysmal rupture occurred in 19 (57.5%) patients, of which 8 (24.2%) were categorized as Hunt-Hess grades IV or V. Aneurysm recurrence or rerupture occurred in five (15.2%) patients, and 5 patients (15.2%) died due to sequelae of their aneurysms. Twenty-one patients (63.6%) had a good outcome (modified Rankin Scale score 0–2) on last follow up. The systematic literature review yielded 48 studies which included 1,482 total aneurysms (611 with endovascular treatment; 656 treated surgically; 215 treated conservatively). Mean aneurysm recurrence rates in the literature were 12.7% and 3.9% for endovascular and surgical treatment, respectively.
Conclusions
Our study provides data on the natural history and longitudinal outcomes for children treated for IAs at a single institution, in addition to our treatment strategies for various aneurysmal morphologies. Despite the high proportion of patients presenting with rupture, good functional outcomes can be achieved for most patients.
Similar content being viewed by others
Introduction
Pediatric intracranial aneurysms (IA) are exceedingly rare lesions with potentially devastating outcomes. While they account for only 1–7% of all IAs, their unique morphologies, locations, and treatment strategies render them distinct from adult IAs [16, 27, 31]. Numerous case series have described the heterogeneity in pediatric IA morphology, with saccular, fusiform, and dissecting subtypes among the most commonly reported [14, 41]. Although some childhood IAs arise in the setting of preexisting conditions, multisystem disease, or trauma, many arise without provocation or known risk factors, leading to numerous theories regarding their pathogenesis [16].
Treatment strategies include both open surgical and endovascular techniques, and depend on the aneurysm size, type, location, patient age, physician/institutional preference and comorbidities [14, 29, 36]. Open surgical techniques such as clipping have long been the standard for aneurysm treatment, but endovascular techniques such as coiling, stent-assisted coiling, and flow diversion have become increasingly used for both adult and pediatric patients [1, 30]. Endovascular approaches have been associated with favorable short-term outcomes; however, endovascular treatment may carry an increased risk of aneurysm recurrence, an important consideration for children [31].
Long-term outcomes vary, and depend on the initial presentation, aneurysm location and treatment method. A meta-analysis by Yasin et al. reported an overall favorable outcome rate (modified Rankin score of 0, 1, or 2) of 85%. Mortality rates range from 5 to 28%, with the majority occurring because of rupture, and a Hunt & Hess grade of IV or V conferring markedly worse outcomes [1, 10, 12, 16, 27, 41].
We report our 18-year experience with pediatric IAs and the evolving approach to care at our institution. We also review the current literature regarding the management of these rare lesions and provide a foundation for future work.
Methods
Study design
We retrospectively reviewed the electronic medical record for patients age ≤ 20 years who were treated for IAs between 2003 and 2020 at Rady Children’s Hospital/University of California, San Diego. IAs associated with arteriovenous malformations (AVMs) were excluded from the study. IAs were typically detected with noninvasive imaging initially due to patient symptomatology or as incidental findings. Digital subtraction angiography (DSA) was used for further characterization when indicated. Patients with subarachnoid hemorrhage (SAH) were classified according to the Hunt & Hess scale, and their CT scans were scored using the Fisher scale. Aneurysm size was classified as small (≤ 10 mm), large (11–25 mm), or giant (≥ 25 mm). Patients were offered endovascular or open surgical treatment depending on IA characteristics and clinical condition. Data regarding perioperative complications, recurrence, retreatment, and functional outcomes were recorded. Patients were followed up at frequent intervals with surveillance imaging.
Data analysis
R v4.2.2, RStudio (The R Foundation), and the “tidyverse” package were used for statistical analysis [37, 39]. α was set at 0.05. Univariate comparisons between open and endovascular treatment groups were completed using independent-sample t test or Welch’s unpaired t-test for continuous variables, and chi-square analysis or Fisher’s exact test for categorical variables. Outcomes of interest included mortality and modified Rankin score at last follow-up. For survival analysis, patients were followed from the time of presentation until the time of their death or the point of last contact. Univariate evaluation of potential prognostic variables was performed with Kaplan-Meier curves and univariate Cox regression analysis.
Systematic literature review
A systematic review of the literature from 1991 to 2022 was performed using the PubMed, Embase, and Web of Science databases. Search terms included (“ped” OR “pipeline” OR “flow diverter” OR “flow diversion” OR “endovascular” OR “coil” OR “coiling” “OR “open surgery” OR “clip” OR “clipping”) AND “aneurysm” AND (“pediatric” OR “paediatric” OR “children” OR “child”). Prospective and retrospective studies were included if they presented primary clinical data and outcomes for pediatric IAs. Secondary data from meta-analyses or literature reviews were excluded. Studies were also excluded if they were classified as abstracts, editorials, expert opinions, or letters. Duplicate articles and data were removed. Data from included studies were collected to summarize the current pediatric IA literature. This work is in accordance with the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines.
Results
Patient characteristics
From 2003 to 2020, 33 patients were treated for 37 aneurysms (Table 1). The mean age was 11.4 years. There were 21 males and 12 females (64% vs. 36%), a male predominance of 1.75:1. Most patients were Hispanic (17, 51.5%), with the remainder being White (10, 30.3%), Asian (5, 15.2%), or Black (1, 3.0%). Aneurysmal rupture was present at initial presentation in 19 (57.6%) patients. Of patients who presented with rupture, 11 (57.9%) had Hunt & Hess grades of IV or V SAH. An external ventricular drain (EVD) was placed in 14 (42.4%) patients.
Aneurysm features: location, size, and morphology
Of the 37 aneurysms treated, 26 (70.3%) arose from the anterior circulation, and 11 (29.7%) arose from the posterior circulation; 19 (51.4%) of these aneurysms were located on the left side, and 17 (46%) were on the right, with one (3.0%) aneurysm arising in the midline from the basilar artery. The most common aneurysm morphologies were saccular (n = 13, 39%) and fusiform (n = 8, 24%), with the remainder (n = 16, 43.2%) being pseudoaneurysmal (n = 2, 6.1%), complex (n = 2, 6.1%), dissecting (n = 2, 6.1%), blister (n = 1, 3.0%), dumbbell (n = 1, 3.0%), mycotic (n = 1, 3.0%), ovoid (n = 1, 3.0%), thrombosed (n = 1, 3.0%), and tumor-associated (n = 1, 3.0%). The median aneurysm size was 10 millimeters (IQR [8, 26]), with 17 (52, four (12%) large aneurysms, and 12 (36%) giant aneurysms (Table 2).
Treatments and outcomes
25 patients (75.8%) underwent open surgery and eight (24.2%) underwent endovascular treatment as their initial intervention; of these patients, 23 (92%) had clip ligation. Initial clip ligation was accompanied by open resection, hematoma evacuation, and aneurysmal wrapping in one (4%) patient each. Finally, IPH evacuation followed by PICA-PICA bypass and open resection followed by lobectomy was performed in one (4%) patient each. Within the endovascular group, three (37.5%) patients had coil embolization, three (37.5%) had pipeline embolization device (PED) stent placements and one (12.5%) patient each had stent-assisted coil embolization and coil embolization with vessel sacrifice. Ten (30.3%) patients required more than one surgery, of which three (30%) were unplanned (one repeat clipping due to aneurysmal recurrence, one coil-assisted vessel sacrifice due to aneurysm re-rupture after stent-assisted coiling, and one balloon angioplasty due to an endoleak after placement of a PED). Two (6.1%) patients required a third intervention to adequately treat their lesions. Recurrence of a treated lesion occurred in one (3.0%) patient (originally treated via clip ligation), and frank re-rupture occurred in four (12.1%) patients (two clip ligations, one PED, and one stent-assisted coil embolization), with two of these events resulting in patient death.
Four (12.1%) patients had complications because of their interventions. All patients had undergone open intervention (although one complication was secondary to intraoperative angiogram). Intraoperative rupture occurred for one patient undergoing clip ligation and resection of a fusiform basilar tip aneurysm, resulting in death 17 days postoperatively. One patient with a giant right saccular AChA aneurysm developed an intracranial abscess after clipping which required surgical evacuation. Another patient with a small right saccular MCA aneurysm developed a CSF leak after clipping which required repair. Finally, one patient who underwent clipping of a giant left vertebral artery saccular aneurysm suffered a left femoral artery thrombus after intraoperative endovascular access and required anticoagulation.
Postoperatively, there were six (18.2%) patients with new deficits, including visual field impairment, vocal cord paralysis, and extremity/hemibody weakness. Deficits were temporary in four (12.1%) patients and permanent in two (6.0%) patients. Six (15.7%) required a permanent shunt, all of whom had undergone open surgery, three of whom had previously required EVD placement, and five of whom had initially presented with aneurysm rupture. At the time of latest follow-up, 12 (36.4%) patients had a modified Rankin score (mRs) of 0, six (18.2%) had a score of 1, three (9.1%) had a score of 2, three (9.1%) had a score of 3, four (9.1%) had a score of 4, and six (18.2%) patients were deceased (Table 2).
Survival analysis
Age, sex, aneurysm circulation (anterior vs. posterior), size, rupture status, EVD placement, and treatment modality (open vs. endovascular) were investigated using univariate chi-square tests, t-tests, Kaplan Meier survival analysis (Fig. 1). There were no factors significantly associated with mortality (Table 3). Overall, 1-year survival was 89% and 5-year survival was 78%. Univariate Cox regression survival analysis did not reveal any significant prognostic factors affecting mortality (Table 4).
A) Kaplan-Meier curve assessing mortality in all patients. B) Kaplan-Meier curve comparing mortality in patients who did or did not require an external ventricular drain (EVD). C) Kaplan-Meier curve comparing mortality in patients treated with endovascular versus open surgical methods. D) Kaplan-Meier curve comparing mortality in patients with ruptured and unruptured aneurysms
Systematic literature review
The literature search across the databases yielded 4,927 publications, of which 48 were included in our literature review summary (Fig. 2). In total, these encompassed 1482 aneurysms (mean of 31 aneurysms per study). There were 611 endovascular and 656 microsurgical procedures. The average age was 11 years old with a mean follow-up time of 3.9 years. Unweighted mean rates of aneurysm recurrence were 12.7% for those treated endovascularly and 3.9% treated microsurgically.
Discussion
While pediatric IAs share some characteristics with their adult counterparts, decades of observation and treatment have established them as distinct entities, defined by unique risk factors, treatment strategies, and prognoses. In this work, we report our experience with pediatric IAs over an 18-year period and compare our results to previously published case series and cohort studies identified in our systematic literature review. All patients were managed by the senior author in collaboration with the endovascular neurosurgery service, building on his experience treating 70 aneurysms in patients < 20 years of age prior to 2003.
Epidemiological features
Numerous studies have established the unique epidemiological and clinical characteristics of pediatric IAs. Most commonly reported is a predilection for males, with ratios in the literature ranging from 1.2:1 to 3:1 [12, 21, 22, 32]. Similarly, our cohort had a male predominance of 1.75. Several authors have also described a bimodal age distribution, in which IAs commonly become symptomatic predominantly by mass effect or SAH within the first two years of life, and again in late adolescence [3, 34]. We did not observe this pattern, although this may be due in part to the inherent rarity of these lesions as well as our limited sample size.
Aneurysm characteristics
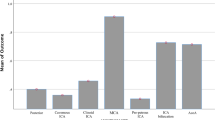
While no single parent artery was clearly predominant, the MCA and ICA were the most represented within our cohort, with 12 and 9 (28.5% and 21.4%) IAs arising from these arteries, respectively. Mehrotra et al. reported MCA/ICA incidence rates of 24.7% & 15.1% respectively; figures which are similar to those by Yasin et al., Garg et al., and others [3, 8, 12, 41].
Children lack many of the risk factors traditionally associated with aneurysm formation in adults, such as hypertension, smoking, and age, and thus many are thought be idiopathic [16]. There may however be a genetic component, as these lesions have been linked with several inherited diseases, such as polycystic kidney disease, aortic coarctation, and sickle cell anemia [26]. Vasculopathies such as Marfan syndrome and Ehlers-Danlos syndrome are implicated in approximately 10% of all pediatric IAs [7, 19]. Pediatric IAs have also been known to affect the posterior circulation at a higher rate than their adult counterparts. While reports vary, most estimates fall between 10% and 40%, consistent with our observed rate of 26.1%, compared to approximately 6% in adults [3, 6, 30].
Pediatric IAs are also structurally distinct. Saccular aneurysms, which encompassed over 90% of adult cases, account for only 30–70% in children, and represented 38.1% of aneurysms in our cohort [9, 11]. Together with fusiform aneurysms (16.7%), these classically described morphologies only comprised just over half of the observed variants in our cohort. This morphological heterogeneity is noted in the literature, many of which report ratios of atypical aneurysms ranging from 30 to 50% [8, 21, 34, 41]. To account for these unique morphologies, Lasjaunias et al. utilized a novel classification system that combined physical architecture with clinical context to classify aneurysms as saccular, fusiform, infectious (mycotic), or traumatic [15, 21]. IAs in children tend to be quite large, with giant aneurysms comprising 3–37% of IAs reported in published case series and 34.3% in our study [21, 25, 31, 33].
Presentation and radiological findings
Children with IAs commonly present with headache, ranging from 50 to 90% in the literature including patients with SAH, and 50% in our cohort [4, 12, 16]. Headaches are multifactorial, and may be caused by mass effect of large or giant aneurysms, turbulent blood flow, or SAH / hydrocephalus. We had a larger proportion of patients presenting in poor neurological condition (Hunt & Hess grade IV or V) (52.1%, 12/23 patients) than observed in other case series (0–43%) [3, 12, 16, 20, 22, 27, 31, 33, 37, 41]. This is possibly due to our institution’s status as a tertiary and quaternary referral center, routinely caring for patients from Mexico and Guam in addition to Southern California.
Treatment methods
Recent years have seen the proliferation of various endovascular techniques to treat aneurysms, including primary coiling, balloon or stent-assisted coiling, and flow diversion. Thus far, these minimally invasive methods show comparable outcomes to traditional open microsurgery for both ruptured and unruptured aneurysms, as reported by numerous meta-analyses and case series [1, 2, 13, 32, 41]. Open treatment via clipping seems to minimize the risk of recurrence, while endovascular intervention is less prone to immediate complications, and may be more suitable for more higher-risk patients with more comorbidities [2, 17, 18, 23, 25]. However, many institutions and individual surgeons/interventionalists prefer one approach, making robust comparisons amongst the literature difficult [35, 40]. In our case series, the majority of aneurysms were treated via an open approach, while the remainder were treated with endovascular methods such as coiling or flow diversion.
Flow-diverting stents are relatively recent additions to the armament of the endovascular neurosurgeon, with emerging literature on their use and long-term efficacy in the pediatric population. Navarro et al. first reported the use of flow diverters in three children to good effect, and later work by Vargas et al., among others, established that these devices, at least within the established follow-up periods, were safe and effective methods of treating complex aneurysms in children [4, 9, 34, 38]. An additional important consideration for the long-term stability and efficacy of PEDs and stents in pediatric patients is ensuring appropriate antiplatelet therapy. While these protocols have been researched extensively in adults, there is little information regarding their applicability to children. In their study assessing flow diverters in children, Barburoglu et al. utilized weight-based dosing extrapolated from adult scales for older, larger children, and modified fractional dosing for younger or lower-weight children [4]. The utilization of flow diverters is also limited in the setting of SAH, which is present at diagnosis for many children, as dual antiplatelets are needed which can be associated with higher rates of hemorrhagic complications, as well as the delayed timeframe of aneurysm thrombosis [24]. However, flow diverters are increasingly being used for adult patients in the setting of rupture, particularly for IAs not amenable to other strategies such as blister aneurysms and may warrant exploration for children as well.
Institutional approach
At our institution, open surgery is the preferred treatment modality for pediatric IAs requiring intervention with amenable morphology. The higher risk of recurrence after endovascular intervention is an important factor for children who may have many decades to live. As shown in our case series, saccular IAs were exclusively clipped while IAs with unusual morphologies and aneurysmal malformations were considered for open or endovascular intervention on a case-by-case basis. Large or thrombosed IAs with mass effect, or ruptured IAs with associated intraparenchymal hemorrhages, were preferentially clipped or resected, while fusiform or dissecting lesions were better treated with endovascular approaches. Specifically, we consider flow diversion for irregularly shaped (e.g. dumbbell, fusiform) IAs that are not amenable to deconstructive techniques (i.e., with coils) due to vessel anatomy.
We frequently use DSA as a diagnostic adjunct, even for IAs considered amenable to open treatment. However, DSA is not without risk in the pediatric patient as the reported complication rates range from 0.4 to 6.7% [5, 7]. The majority of complications seen in these studies, however, were transient neurological deficits, with major complications occurring in 3/587 patients and 1/241 patients, respectively [5, 7]. We observed one DSA-related complication, a femoral artery thrombus requiring anticoagulation in a 2-year-old after intraoperative DSA during craniotomy.
As stent-assisted coiling and flow diversion require dual antiplatelet therapy (DAPT), they are rarely utilized in the setting of rupture to avoid hemorrhagic complications. Optimal antiplatelet regimens are not well established in children, particularly in those age less than 10 [8, 28]. We typically use aspirin plus a Plavix elixir for at least 6 months in those who require DAPT. Children are assessed with serial platelet reactivity tests to determine the minimum weight-based dose to achieve therapeutic effect.
Patients undergo post-intervention surveillance with MRA every 6–12 months to minimize tests involving radiation and undergo follow-up DSA if there is a concern for recurrence.
Outcomes
We did not identify any factors significantly impacting survival, possibly due to the high survival rate even among ruptured aneurysm patients in our series of 84%. Within the literature, post-treatment mortality rates range from 2 to 35% [14, 15, 16, 20]. Rebleeding from either de novo or recurrent aneurysms is one of the major factors of perioperative mortality in these patients, which underlines the need for consistent follow-up and surveillance imaging [2]. Recurrence occurred in five (13%) patients in our case series; only one recurrence was noted on surveillance imaging, and the other four presented as delayed post-treatment ruptures in which prior follow-up DSAs had demonstrated obliteration. Amelot et al. noted that rebleeding of IAs were associated with a higher mortality rate compared to unruptured aneurysms in their multivariate analysis (OR = 9.2; p = 0.02) [2]. Yasin et al. and others have also demonstrated an association between SAH severity (as measured by Hunt & Hess grade) and poor functional status and mortality by measure of Glasgow Outcomes Scale [36, 41].
In our series, four (10.5%) patients suffered periprocedural complications; results which are within the range reported in the literature (range 0–54%) [10, 17, 25]. Commonly reported complications in prior studies include intraoperative rupture and bleeding, thrombotic events, transient cranial nerve palsies, and neurocognitive deficits [15, 16, 20]. Recurrent aneurysms or reoperation occurs in a small but significant number of patients. In a study of 51 surgically treated pediatric IA patients, 60% experienced rebleeding, and 23% experienced asymptomatic aneurysm recurrence [2]. Another series of 57 aneurysms found favorable outcomes in the vast majority of cases using endovascular techniques, with complications including three new neurological deficits, two aneurysms recurrences that required retreatment, and one aneurysm rerupture that required retreatment [41]. Regardless of the treatment modality, close follow up is needed as re-treatment may be indicated for aneurysmal neck remnants detected on post-treatment angiograms, de-novo aneurysms that form in patients with connective tissue disorders, or after subsequent (potentially occult) bleeding events.
Limitations
Limitations of our study include its retrospective design, rarity of the pathology, and the long inclusion period (18 years) during which endovascular technologies have expanded and evolved. Treatment algorithms for rare pathologies such as pediatric IAs rely heavily on resources available at the institution, as well as the treating team’s clinical experience, and thus might not be generalizable to other hospitals. We also acknowledge that the relatively small sample size may have limited power to detect statistical differences between groups.
Conclusion
We describe our institutional approach to the preoperative evaluation, treatment selection, and postoperative care for a variety of aneurysmal morphologies in children. Intraoperative and postoperative complications were rare, with only one perioperative mortality. We performed a systematic literature review which contextualizes our findings with the existing literature. Our series builds on prior data demonstrating that good functional outcomes can be achieved for most pediatric IA patients.
Data availability
No datasets were generated or analysed during the current study.
References
Agid R, Souza MP, Reintamm G, Armstrong D, Dirks P, TerBrugge KG (2005) The role of endovascular treatment for pediatric aneurysms. Childs Nerv Syst 21:1030–1036
Amelot A, Saliou G, Benichi S, Alias Q, Boulouis G, Zerah M, Aghakhani N, Ozanne A, Blauwblomme T, Naggara O (2019) Long-term outcomes of cerebral aneurysms in Children. Pediatrics 143
Aryan HE, Giannotta SL, Fukushima T, Park MS, Ozgur BM, Levy ML (2006) Aneurysms in children: review of 15 years experience. J Clin Neurosci 13:188–192
Barburoglu M, Arat A (2017) Flow diverters in the treatment of Pediatric Cerebrovascular diseases. AJNR Am J Neuroradiol 38:113–118
Bashir Q, Ishfaq A, Baig AA (2018) Safety of diagnostic cerebral and Spinal Digital Subtraction Angiography in a developing country: a single-center experience. Interv Neurol 7:99–109
Brinjikji W, Nasr DM, Flemming KD, Rouchaud A, Cloft HJ, Lanzino G, Kallmes DF (2017) Clinical and imaging characteristics of diffuse intracranial dolichoectasia. AJNR Am J Neuroradiol 38:915–922
Burger IM, Murphy KJ, Jordan LC, Tamargo RJ, Gailloud P (2006) Safety of cerebral digital subtraction angiography in children: complication rate analysis in 241 consecutive diagnostic angiograms. Stroke 37:2535–2539
Chen R, Zhang S, You C, Guo R, Ma L (2018) Pediatric intracranial aneurysms: changes from previous studies. Childs Nerv Syst 34:1697–1704
Cherian J, Srinivasan V, Froehler MT, Grossberg JA, Cawley CM, Hanel RA, Puri A, Dumont T, Ducruet AF, Albuquerque F, Arthur A, Cheema A, Spiotta A, Anadani M, Lopes D, Saied A, Kim L, Kelly CM, Chen PR, Mocco J, De Leacy R, Powers CJ, Grandhi R, Fargen KM, Chen SR, Johnson JN, Lam S, Kan P (2020) Flow Diversion for Treatment of Intracranial aneurysms in Pediatric patients: Multicenter Case Series. Neurosurgery 87:53–62
Clarke JE, Luther E, Oppenhuizen B, Leuchter JD, Ragheb J, Niazi TN, Wang S (2022) Intracranial aneurysms in the infant population: an institutional case series and individual participant data meta-analysis. J Neurosurg Pediatr : 1–11
Deora H, Rao KVLN, Somanna S, Srinivas D, Shukla DP, Bhat DI (2017) Surgically managed Pediatric Intracranial aneurysms: how different are they from adult intracranial. Aneurysms? Pediatr Neurosurg 52:313–317
Garg K, Singh PK, Sharma BS, Chandra PS, Suri A, Singh M, Kumar R, Kale SS, Mishra NK, Gaikwad SK, Mahapatra AK (2014) Pediatric intracranial aneurysms–our experience and review of literature. Childs Nerv Syst 30:873–883
Garrido E, Metayer T, Borha A, Langlois O, Curey S, Papagiannaki C, Di Palma C, Emery E, Derrey S, Gaberel T, Gilard V (2021) Intracranial aneurysms in pediatric population: a two-center audit. Childs Nerv Syst 37:2567–2575
Ghali MGZ, Srinivasan VM, Cherian J, Wagner KM, Chen SR, Johnson J, Lam SK, Kan P (2018) Multimodal Treatment of Intracranial Aneurysms in children: clinical Case Series and Review of the literature. World Neurosurg 111:e294–e307
Hetts SW, Narvid J, Sanai N, Lawton MT, Gupta N, Fullerton HJ, Dowd CF, Higashida RT, Halbach VV (2009) Intracranial aneurysms in childhood: 27-year single-institution experience. AJNR Am J Neuroradiol 30:1315–1324
Huang J, McGirt MJ, Gailloud P, Tamargo RJ (2005) Intracranial aneurysms in the pediatric population: case series and literature review. Surg Neurol 63:424–432 discussion 432 – 423
Kakarla UK, Beres EJ, Ponce FA, Chang SW, Deshmukh VR, Bambakidis NC, Zabramski JM, Spetzler RF (2010) Microsurgical treatment of pediatric intracranial aneurysms: long-term angiographic and clinical outcomes. Neurosurgery 67:237–249 discussion 250
Kang XK, Guo SF, Lei Y, Wei W, Liu HX, Huang LL, Jiang QL (2020) Endovascular coiling versus surgical clipping for the treatment of unruptured cerebral aneurysms: direct comparison of procedure-related complications. Med (Baltim) 99:e19654
Kim ST, Brinjikji W, Lanzino G, Kallmes DF (2016) Neurovascular manifestations of connective-tissue diseases: a review. Interv Neuroradiol 22:624–637
Koroknay-P·l P, Lehto H, Niemel‰ M, Kivisaari R, Hernesniemi J (2012) Long-term outcome of 114 children with cerebral aneurysms. J Neurosurg Pediatr 9:636–645
Lasjaunias P, Wuppalapati S, Alvarez H, Rodesch G, Ozanne A (2005) Intracranial aneurysms in children aged under 15 years: review of 59 consecutive children with 75 aneurysms. Childs Nerv Syst 21:437–450
Liang J, Bao Y, Zhang H, Wrede KH, Zhi X, Li M, Ling F (2009) The clinical features and treatment of pediatric intracranial aneurysm. Childs Nerv Syst 25:317–324
Lv X, Jiang C, Li Y, Yang X, Wu Z (2009) Endovascular treatment for pediatric intracranial aneurysms. Neuroradiology 51:749–754
Madaelil TP, Moran CJ, Cross DT, Kansagra AP (2017) Flow Diversion in ruptured intracranial aneurysms: a Meta-analysis. AJNR Am J Neuroradiol 38:590–595
Nam SM, Jang D, Wang KC, Kim SK, Phi JH, Lee JY, Cho WS, Kim JE, Kang HS (2019) Characteristics and treatment outcome of intracranial aneurysms in children and adolescents. J Korean Neurosurg Soc 62:551–560
Patel AN, Richardson AE (1971) Ruptured intracranial aneurysms in the first two decades of life. A study of 58 patients. J Neurosurg 35:571–576
Proust F, Toussaint P, GarniÈri J, Hannequin D, Legars D, Houtteville JP, FrÈger P (2001) Pediatric cerebral aneurysms. J Neurosurg 94:733–739
Ravindra VM, Bollo RJ, Dewan MC, Riva-Cambrin JK, Tonetti D, Awad AW, Akbari SH, Gannon S, Shannon C, Birkas Y, Limbrick D, Jea A, Naftel RP, Kestle JR, Grandhi R (2021) Comparison of anticoagulation and antiplatelet therapy for treatment of blunt cerebrovascular injury in children < 10 years of age: a multicenter retrospective cohort study. Childs Nerv Syst 37:47–54
Requejo F, Ceciliano A, Cardenas R, Villasante F, Jaimovich R, Zuccaro G (2010) Cerebral aneurysms in children: are we talking about a single pathological entity? Childs Nerv Syst 26:1329–1335
Saleh E, Dawson RC (2011) Endovascular management of pediatric aneurysms. Neuroradiol J 24:693–698
Sanai N, Quinones-Hinojosa A, Gupta NM, Perry V, Sun PP, Wilson CB, Lawton MT (2006) Pediatric intracranial aneurysms: durability of treatment following microsurgical and endovascular management. J Neurosurg 104:82–89
Saraf R, Shrivastava M, Siddhartha W, Limaye U (2012) Intracranial pediatric aneurysms: endovascular treatment and its outcome. J Neurosurg Pediatr 10:230–240
Sharma BS, Sinha S, Mehta VS, Suri A, Gupta A, Mahapatra AK (2007) Pediatric intracranial aneurysms-clinical characteristics and outcome of surgical treatment. Childs Nerv Syst 23:327–333
Shlobin NA, Raz E, Shapiro M, Moretti L, Cantrell DR, Lam SK, Hurley MC, Ansari SA, Nossek E, Riina HA, Nelson PK, Jahromi BS, Shaibani A, Potts MB (2021) Pipeline embolization of cerebral aneurysms in pediatric patients: combined systematic review of patient-level data and multicenter retrospective review. J Neurosurg Pediatr 27:668–676
Slator N, Talibi SS, Mundil N, Thomas A, Lamin S, Walsh R, Rodrigues D, Solanki GA (2019) Paediatric intracranial aneurysms: a British institutional review. Childs Nerv Syst 35:1197–1205
Sorteberg A, Dahlberg D (2013) Intracranial non-traumatic aneurysms in children and adolescents. Curr Pediatr Rev 9:343–352
Team RC (2022) In: Team RC (ed) R: a Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna
Vargas SA, Diaz C, Herrera DA, Dublin AB (2016) Intracranial aneurysms in children: the role of Stenting and Flow-Diversion. J Neuroimaging 26:41–45
Wickham H, Averick M, Bryan J, Chang W, McGowan LDA, François R et al Welcome to the tidyverse. In: 2019 (ed). Journal of Open Source Software, p 1686
Yang M, Wang S, Zhao Y, Zhao J (2008) Management of intracranial aneurysm in children: clipped and coiled. Childs Nerv Syst 24:1005–1012
Yasin JT, Wallace AN, Madaelil TP, Osbun JW, Moran CJ, Cross DT, Limbrick DD, Zipfel GJ, Dacey RG, Kansagra AP (2019) Treatment of pediatric intracranial aneurysms: case series and meta-analysis. J Neurointerv Surg 11:257–264
Author information
Authors and Affiliations
Contributions
M.B., M.S., C.M., and G.P. wrote the main manuscript text and prepared the tables and figures. All authors critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brandel, M.G., Plonsker, J.H., Rennert, R.C. et al. Treatment of pediatric intracranial aneurysms: institutional case series and systematic literature review. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06384-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06384-x