Abstract
Purpose
Lateral meningocele syndrome (LMS) is a rare genetic connective tissue disorder which is associated with meningocele-related neurologic dysfunction. Several patients with LMS have been reported. But, guidelines for screening and treatment of LMS have not been established.
Method and results
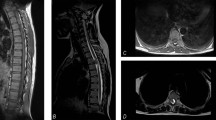
We review the current knowledge of LMS in the article. Then, we describe a boy for whom a genomic analysis which allowed us to make a diagnosis of LMS and to begin monitoring of his condition for possible neurological complications.
Conclusion
It would be difficult to make a diagnosis of LMS on the basis of clinical manifestations alone. The natural history of dural ectasia in patients with LMS needs to be better defined to establish surgical indications. Based upon the current literature, ventriculoperitoneal shunting (V-Ps) has been recommended as the first-line surgical treatment option for patients with symptomatic thoracolumbar meningoceles.



Similar content being viewed by others
Data availability
Not applicable.
References
Gripp KW, Robbins KM, Sobreira NL et al (2015) Truncating mutations in the last exon of NOTCH3 cause lateral meningocele syndrome. Am J Med Genet A 167A(2):271–281. https://doi.org/10.1002/ajmg.a.36863
Ejaz R, Carter M, Gripp K (2016) Lateral meningocele syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; June 23
Brown EC, Gupta K, Sayama C (2017) Neurosurgical management in lateral meningocele syndrome: case report. J Neurosurg Pediatr 19(2):232–238. https://doi.org/10.3171/2016.9.PEDS16311
Yamada M, Arimitsu T, Suzuki H, Miwa T, Kosaki K (2021) Early diagnosis of lateral meningocele syndrome in an infant without neurological symptoms based on genomic analysis [published online ahead of print, 2021 Jun 13]. Childs Nerv Syst.https://doi.org/10.1007/s00381-021-05232-6
Cuoco JA, Klein BJ, Busch CM et al (2020) Neurosurgical management of lateral meningocele syndrome: a clinical update for the pediatric neurosurgeon. Pediatr Neurosurg 55(1):2–11. https://doi.org/10.1159/000504060
Katz SG, Grünebaum M, Strand RD (1978) Thoracic and lumbar dural ectasia in a two-year-old boy. Pediatr Radiol 6(4):238–240. https://doi.org/10.1007/BF00975545
Chen KM, Bird L, Barnes P, Barth R, Hudgins L (2005) Lateral meningocele syndrome: vertical transmission and expansion of the phenotype. Am J Med Genet A 133A(2):115–121. https://doi.org/10.1002/ajmg.a.30526
Lehman RA, Stears JC, Wesenberg RL, Nusbaum ED (1977) Familial osteosclerosis with abnormalities of the nervous system and meninges. J Pediatr 90(1):49–54. https://doi.org/10.1016/s0022-3476(77)80763-4
Ejaz R, Qin W, Huang L et al (2016) Lateral meningocele (Lehman) syndrome: a child with a novel NOTCH3 mutation. Am J Med Genet A 170A(4):1070–1075. https://doi.org/10.1002/ajmg.a.37541
Castori M, Morlino S, Ritelli M et al (2014) Late diagnosis of lateral meningocele syndrome in a 55-year-old woman with symptoms of joint instability and chronic musculoskeletal pain. Am J Med Genet A 164A(2):528–534. https://doi.org/10.1002/ajmg.a.36301
Cappuccio G, Apuzzo D, Alagia M et al (2020) Expansion of the phenotype of lateral meningocele syndrome. Am J Med Genet A 182(5):1259–1262. https://doi.org/10.1002/ajmg.a.61536
Gripp KW, Scott CI Jr, Hughes HE et al (1997) Lateral meningocele syndrome: three new patients and review of the literature. Am J Med Genet 70(3):229–239
Pinna G, Alessandrini F, Alfieri A, Rossi M, Bricolo A (2000) Cerebrospinal fluid flow dynamics study in Chiari I malformation: implications for syrinx formation. Neurosurg Focus 8(3):E3. Published 2000 Mar 15. https://doi.org/10.3171/foc.2000.8.3.3
Kim YJ, Cho HM, Yoon CS, Lee CK, Lee TY, Seok JP (2011) Surgical treatment of thoracic menigocele associated with neurofibromatosis and kyphoscoliosis. Korean J Thorac Cardiovasc Surg 44(5):383–386. https://doi.org/10.5090/kjtcs.2011.44.5.383
Rainov NG, Heidecke V, Burkert W(1995) Thoracic and lumbar meningocele in neurofibromatosis type 1. Report of two cases and review of the literature. Neurosurg Rev 18(2):127–134. https://doi.org/10.1007/BF00417670
Philip N, Andrac L, Moncla A et al (1995) Multiple lateral meningoceles, distinctive facies and skeletal anomalies: a new case of Lehman syndrome. Clin Dysmorphol 4(4):347–351. https://doi.org/10.1097/00019605-199510000-00011
Piper RJ, Pike M, Harrington R, Magdum SA (2019) Chiari malformations: principles of diagnosis and management. BMJ 365:l1159. Published 2019 Apr 8. https://doi.org/10.1136/bmj.l1159
Davidson KA, Rogers JM, Stoodley MA (2018) Syrinx to subarachnoid shunting for syringomyelia. World Neurosurg 110:e53–e59. https://doi.org/10.1016/j.wneu.2017.09.205
Funding
The study was supported by the University natural science research project of Jiangsu province (21KJB320019).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yong Han is the first author.
Rights and permissions
About this article
Cite this article
Han, Y., Chen, M. & Wang, H. Management of lateral meningocele syndrome in a child without neurological symptoms and literature review. Childs Nerv Syst 38, 903–907 (2022). https://doi.org/10.1007/s00381-022-05466-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05466-y