Abstract
Purpose
German pediatric guidelines for severe traumatic brain injury (TBI) management expired in 2011. Thus, divergent evidence-based institutional protocols are predominantly being followed. We performed a survey of current Pediatric Intensive Care Unit (PICU) management of isolated severe TBI in Germany to reveal potential varying practices.
Methods
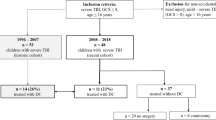
Seventy German PICUs were invited to join an anonymous online survey from February to May 2017. Twenty-nine participants (41.4%) successfully completed the survey (17 university hospitals and 12 district hospitals). The majority of items were polar (yes/no) or scaled (e.g., never - always). Main topics were imaging, neurosurgery, neuromonitoring, adjuvant therapy, and medication. Severity of TBI was defined via Glasgow Coma Scale.
Results
The majority of respondents (93.1%) had internal TBI standards, and patients were mainly administered to interdisciplinary trauma units. The use of advanced neuromonitoring techniques, intracranial hypertension management, and drug treatment differed between PICUs. Routine administration of hypertonic saline in TBI-associated cerebral edema was performed by 3.4%, while it was never an option for 31.0% of the participants. Prophylactic anticonvulsive therapy was restrictively performed. If indicated, the main anticonvulsive drugs used were phenobarbital and levetiracetam. Neuroendocrine follow-up was recommended/performed by 58.6% of the PICUs.
Conclusions
This survey provides an overview of the current PICU practices of isolated severe TBI management in Germany and demonstrates a wide instrumental and therapeutical range, revealing an unmet need for the revised national guideline and further (international) clinical trials for the treatment of severe TBI in pediatrics.




Similar content being viewed by others
References
Zaloshnja E, Miller T, Langlois JA, Selassie AW (2008) Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil 23:394–400
Coronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, Faul MD et al (2011) Surveillance for traumatic brain injury-related deaths—United States, 1997-2007. MMWR Surveill Summ 60:1–32
Kipfmueller F, Wyen H, Borgman MA, Spinella PC, Wirth S, Maegele M (2013) Epidemiology, risk stratification and outcome of severe pediatric trauma. Klin Padiatr 225:34–40
Elsässer G (2011) Unfälle, Gewalt, Selbstverletzung bei Kindern und Jugendlichen. Ergebnisse der amtlichen Statistik zum Verletzungsgeschehen 2009. Statistisches Bundesamt, Wiesbaden (https://www.destatis.de/)
Steudel WI, Cortbus F, Schwerdtfeger K (2005) Epidemiology and prevention of fatal head injuries in Germany—trends and the impact of the reunification. Acta Neurochir 147:231–242 discussion 242
Majdan M, Plancikova D, Brazinova A, Rusnak M, Nieboer D, Feigin V, Maas A (2016) Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health 1:e76–e83
Sarnaik A, Ferguson NM, O'Meara AMI, Agrawal S, Deep A, Buttram S et al (2018) Age and mortality in pediatric severe traumatic brain injury: results from an international study. Neurocrit Care 28:302–313
Vavilala MS, Kernic MA, Wang J, Kannan N, Mink RB, Wainwright MS, Groner JI, Bell MJ, Giza CC, Zatzick DF, Ellenbogen RG, Boyle LN, Mitchell PH, Rivara FP, Pediatric Guideline Adherence and Outcomes Study (2014) Acute care clinical indicators associated with discharge outcomes in children with severe traumatic brain injury. Crit Care Med 42:2258–2266
AWMF Guideline (13.02.2011) Register-ID: 024/018 – Schädel-Hirn-Trauma im Kindesalter (https://www.awmf.org)
Blaha M, Lazar D, Winn RH, Ghatan S (2003) Hemorrhagic complications of intracranial pressure monitors in children. Pediatr Neurosurg 39:27–31
Roberts I, Yates D, Sandercock P, Farrell B, Wasserberg J, Lomas G, Cottingham R, Svoboda P, Brayley N, Mazairac G, Laloë V, Muñoz-Sánchez A, Arango M, Hartzenberg B, Khamis H, Yutthakasemsunt S, Komolafe E, Olldashi F, Yadav Y, Murillo-Cabezas F, Shakur H, Edwards P, CRASH trial collaborators (2004) Effect of intravenous corticosteroids on death within 14 days in 10008 adults with clinically significant head injury (MRC CRASH trial): randomised placebo-controlled trial. Lancet 364:1321–1328
Kochanek PM, Carney N, Adelson PD, Ashwal S, Bell MJ, Bratton S et al (2012) Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents—second edition. Pediatric Crit Care Med : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 13(Suppl 1):S1–S82
Bell MJ, Adelson PD, Wisniewski SR, Investigators of the AS (2017) Challenges and opportunities for pediatric severe TBI-review of the evidence and exploring a way forward. Child’s Nerv Syst: ChNS : official journal of the International Society for Pediatric Neurosurgery 33:1663–1667
Boone MD, Oren-Grinberg A, Robinson TM, Chen CC, Kasper EM (2015) Mannitol or hypertonic saline in the setting of traumatic brain injury: what have we learned? Surg Neurol Int 6:177
Kurz JE, Poloyac SM, Abend NS, Fabio A, Bell MJ, Wainwright MS, Investigators for the Approaches and Decisions in Acute Pediatric TBI Trial (2016) Variation in anticonvulsant selection and electroencephalographic monitoring following severe traumatic brain injury in children-understanding resource availability in sites participating in a comparative effectiveness study. Pediatric Crit Care Med : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 17:649–657
Kruer RM, Harris LH, Goodwin H, Kornbluth J, Thomas KP, Slater LA et al (2013) Changing trends in the use of seizure prophylaxis after traumatic brain injury: a shift from phenytoin to levetiracetam. J Crit Care 28(883):e889–e813
Vella MA, Crandall ML, Patel MB (2017) Acute management of traumatic brain injury. Surg Clin North Am 97:1015–1030
Bor-Seng-Shu E, Figueiredo EG, Amorim RL, Teixeira MJ, Valbuza JS, de Oliveira MM et al (2012) Decompressive craniectomy: a meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg 117:589–596
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness a practical scale. Lancet 2:81–84
Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Feigelson HS, Roblin D, Flynn MJ, Vanneman N, Smith-Bindman R (2013) The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr 167:700–707
Narotam PK, Burjonrappa SC, Raynor SC, Rao M, Taylon C (2006) Cerebral oxygenation in major pediatric trauma: its relevance to trauma severity and outcome. J Pediatr Surg 41:505–513
Schrieff-Elson LE, Thomas KG, Rohlwink UK, Figaji AA (2015) Low brain oxygenation and differences in neuropsychological outcomes following severe pediatric TBI. Child’s Nerv Syst : ChNS : official journal of the International Society for Pediatric Neurosurgery 31:2257–2268
Huh JW, Raghupathi R (2009) New concepts in treatment of pediatric traumatic brain injury. Anesthesiol Clin 27:213–240
Stiefel MF, Udoetuk JD, Storm PB, Sutton LN, Kim H, Dominguez TE, Helfaer MA, Huh JW (2006) Brain tissue oxygen monitoring in pediatric patients with severe traumatic brain injury. J Neurosurg 105:281–286
Stowe CD, Lee KR, Storgion SA, Phelps SJ (2000) Altered phenytoin pharmacokinetics in children with severe, acute traumatic brain injury. J Clin Pharmacol 40:1452–1461
Torbic H, Forni AA, Anger KE, Degrado JR, Greenwood BC (2013) Use of antiepileptics for seizure prophylaxis after traumatic brain injury. Am J Health Syst Pharm 70:759–766
Bansal S, Blalock D, Kebede T, Dean NP, Carpenter JL (2014) Levetiracetam versus (fos)phenytoin for seizure prophylaxis in pediatric patients with intracranial hemorrhage. J Neurosurg Pediatr 13:209–215
Zou H, Brayer SW, Hurwitz M, Niyonkuru C, Fowler LE, Wagner AK (2013) Neuroprotective, neuroplastic, and neurobehavioral effects of daily treatment with levetiracetam in experimental traumatic brain injury. Neurorehabil Neural Repair 27:878–888
Szaflarski JP, Sangha KS, Lindsell CJ, Shutter LA (2010) Prospective, randomized, single-blinded comparative trial of intravenous levetiracetam versus phenytoin for seizure prophylaxis. Neurocrit Care 12:165–172
Adelson PD, Wisniewski SR, Beca J, Brown SD, Bell M, Muizelaar JP, Okada P, Beers SR, Balasubramani GK, Hirtz D, Paediatric Traumatic Brain Injury Consortium (2013) Comparison of hypothermia and normothermia after severe traumatic brain injury in children (cool kids): a phase 3, randomised controlled trial. The Lancet Neurology 12:546–553
Mellion SA, Bennett KS, Ellsworth GL, Moore K, Riva-Cambrin J, Metzger RR, Bratton SL (2013) High-dose barbiturates for refractory intracranial hypertension in children with severe traumatic brain injury. Pediatric Crit Care Med : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 14:239–247
Weintraub D, Williams BJ, Jane J Jr (2012) Decompressive craniectomy in pediatric traumatic brain injury: a review of the literature. NeuroRehabilitation 30:219–223
Rutigliano D, Egnor MR, Priebe CJ, McCormack JE, Strong N, Scriven RJ et al (2006) Decompressive craniectomy in pediatric patients with traumatic brain injury with intractable elevated intracranial pressure. J Pediatr Surg 41:83–87 discussion 83-87
Ylvisaker M, Adelson PD, Braga LW, Burnett SM, Glang A, Feeney T, Moore W, Rumney P, Todis B (2005) Rehabilitation and ongoing support after pediatric TBI: twenty years of progress. J Head Trauma Rehabil 20:95–109
Behan LA, Phillips J, Thompson CJ, Agha A (2008) Neuroendocrine disorders after traumatic brain injury. J Neurol Neurosurg Psychiatry 79:753–759
Reinisch JF, Yu DC, Li WY (2016) Getting a valid survey response from 662 plastic surgeons in the 21st century. Ann Plast Surg 76:3–5
Bakhru RN, McWilliams DJ, Wiebe DJ, Spuhler VJ, Schweickert WD (2016) Intensive care unit structure variation and implications for early mobilization practices. An international survey. Ann Am Thorac Soc 13:1527–1537
Acknowledgements
We thank all participants who committed their time and effort. We thank Prof. Dr. Dr. h.c. Wolfgang Rascher for supporting this study. Data acquisition was performed by Valerie Konrad in fulfillment of the requirements for obtaining the degree “Dr. med.” at the Friedrich-Alexander-University of Erlangen-Nuremberg, Dept. of Pediatrics and Adolescent Medicine, Germany.
Funding
Departmental funds only.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare no competing interests.
Additional information
Thomas M. K. Völkl and Fabian B. Fahlbusch contributed equally to this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Regensburger, A.P., Konrad, V., Trollmann, R. et al. Treatment of severe traumatic brain injury in German pediatric intensive care units—a survey of current practice. Childs Nerv Syst 35, 815–822 (2019). https://doi.org/10.1007/s00381-019-04098-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04098-z