Abstract
Background
Langerhans cell histiocytosis (LCH) is a disorder of immature LCH cells, eosinophils, macrophages, lymphocytes, and multinucleated giant cells. Eosinophilic granuloma (EG) is a focal form of LCH that presents mostly in the skull, femur, vertebrae, pelvis, mandible, and ribs. Intracranial presentation of EG is very rare in the literature.
Case description
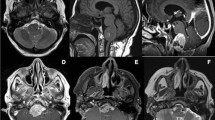
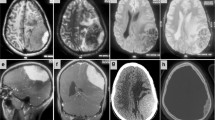
A 17-year-old boy visited our clinic with headache, dizziness, and tinnitus that were present for 2 months. Brain MRI depicted a lesion at the right cerebellopontine angle. The lesion was hypointense on T1-weighted and hyperintense on T2-weighted brain MR images. The lesion enhanced homogenously after I.V. contrast material administration. Pre-operative diagnoses were vestibular schwannoma and meningioma. Surgery was planned. Retrosigmoid approach was preferred in the surgery. The lesion was excised partially. Pathological analysis depicted cell infiltration composed of eosinophils besides histiocytes, plasma cells, and lymphocytes in different amounts. CD1a was positive yet S100 was negative. Final diagnosis was eosinophilic granuloma. Post-operative course was uneventful. The patient was referred to pediatric oncology unit, and steroid therapy was initiated. Post-operative follow-up brain MRIs showed that the lesion had regressed further than immediate post-operative images by only steroid use. In long-term follow-up, new lesions appeared on the patient’s skin in multiple locations and in the sclera of his left eye. At the last follow-up (3 years post-operatively) skin and scleral lesions were noticed to have regressed spontaneously and the intracranial structures were tumor free.
Discussion and conclusion
To the best of our knowledge, EG at the cerebellopontine angle has not been presented in the literature. What makes our case further unique is its negativity for S-100 antigen. Eosinophilic granuloma should be kept in differential diagnosis of mass lesions presented at the cerebellopontine angle, especially in children and young adults with high eosinophils and lymphocytes in their peripheral blood. Sole steroid trials could be conveyed in suspicious cases before any further intervention. If the lesions do not regress or enlarge with time, surgery should be considered. However, long-term follow-up of these patients is necessary since natural history of the disease has not been defined, yet.


Similar content being viewed by others
References
Grana N (2014) Langerhans cell histiocytosis. Cancer Control 21:328–334
Mut M, Cataltepe O, Bakar B, Cila A, Akalan N (2004) Eosinophilic granuloma of the skull associated with epidural haematoma: a case report and review of the literature. Childs Nerv Syst 20:765–769
Grant GA, Kim DK, Shaw CM, Berger MS (1999) Solitary eosinophilic granuloma of the temporal lobe: case report and review of the literature. Brain Tumor Pathol 16:55–59
Penar PL, Kim JH, Chyatte D (1987) Solitary eosinophilic granuloma of the frontal lobe. Neurosurgery 21:566–568
Itoh H, Waga S, Kojima T, Hoshino T (1992) Solitary eosinophilic granuloma in the frontal lobe: case report. Neurosurgery 30:295–298
Hayashi Y, Hashida K, Takaoka Y, Mise H, Nishikawa T, Takada K, Kanemitsu N, Itoh T, Matsumoto H, Ueda N (1993) A histiocytosis X without histological findings: a new entity of histiocytosis X. Kokyu To Junkan 41:171–174
Cerda-Nicolas M, Broseta J, Peydro-Olaya A, Barbera J, Barcia-Salorio JL, Llombart-Bosch A (1980) Primary eosinophilic granuloma of the frontal lobe. Virchows Arch A Pathol Anat Histol 388:221–228
Azumi N, Sheibani K, Swartz WG, Stroup RM, Rappaport H (1988) Antigenic phenotype of Langerhans cell histiocytosis: an immunohistochemical study demonstrating the value of LN-2, LN-3, and vimentin. Hum Pathol 19:1376–1382
Pennisi EM, Palladini G, Buttinelli C, Cusimano G, Galgani S, Lauro G, Fieschi C (1995) Immunohistological study of a case of cerebral Langerhans cell histiocytosis in brain biopsy. Clin Neuropathol 14:25–28
Acknowledgments
Murat Şakir Ekşi, M.D. was supported by a grant from Tubitak (The Scientific and Technological Research Council of Turkey), Grant number: 1059B191400255.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Öğrenci, A., Batçık, O.E., Ekşi, M.Ş. et al. Pandora’s box: eosinophilic granuloma at the cerebellopontine angle—should we open it?. Childs Nerv Syst 32, 1513–1516 (2016). https://doi.org/10.1007/s00381-015-2982-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2982-1