Abstract
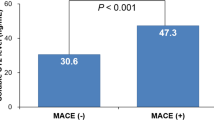
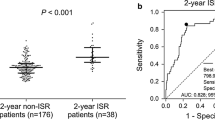
Cell division cycle 42 (CDC42) regulates cholesterol efflux, chronic inflammation, and reendothelialization in various atherosclerotic diseases. This study aimed to investigate the correlation of serum CDC42 with myocardial injury indicators and major adverse cardiac event (MACE) in ST-elevation myocardial infarction (STEMI) patients who were treated with percutaneous coronary intervention (PCI). In 250 STEMI patients about to receive PCI, serum samples were collected at enrollment before PCI treatment, and the serum samples were also obtained from 100 healthy controls (HCs) at enrollment. Serum CDC42 was detected by enzyme-linked immunosorbent assay. Serum CDC42 was decreased (versus HCs, P < 0.001) and negatively correlated with diabetes mellitus (P = 0.017), multivessel disease (P = 0.016), cardiac troponin I (P < 0.001), creatine kinase MB (P = 0.012), stent diameter ≥ 3.5 mm (P = 0.039), white blood cell (P < 0.001), low-density lipoprotein cholesterol (P = 0.049), and C-reactive protein (P < 0.001) in STEMI patients. Besides, 29 (11.6%) STEMI patients experienced MACE. The 1-year, 2-year, and 3-year accumulating MACE rates were 7.5%, 17.3%, and 19.3%, accordingly. Serum CDC42 was reduced in STEMI patients who experienced MACE compared to those who did not (P = 0.001). Serum CDC42 ≥ 250 pg/mL, ≥ 400 pg/mL, ≥ 700 pg/mL (cut by near integer value of 1/4th quartile, median, and 3/4th quartile) were associated with decreased accumulating MACE rates in STEMI patients (all P < 0.050). Notably, serum CDC42 ≥ 250 pg/mL (hazard ratio = 0.435, P = 0.031) was independently related to reduced accumulating MACE risk in STEMI patients. A serum CDC42 level of ≥ 250 pg/mL well predicts decreased MACE risk in STEMI patients who are treated with PCI.



Similar content being viewed by others
Data Availability
The original data presented in this study are included in the article, further inquiries can be directed to the corresponding author.
References
Bhatt DL, Lopes RD, Harrington RA (2022) Diagnosis and treatment of Acute Coronary syndromes: a review. JAMA 327(7):662–675
Vogel B, Claessen BE, Arnold SV, Chan D, Cohen DJ, Giannitsis E, Gibson CM, Goto S, Katus HA, Kerneis M, Kimura T, Kunadian V, Pinto DS, Shiomi H, Spertus JA, Steg PG, Mehran R (2019) ST-segment elevation Myocardial Infarction. Nat Rev Dis Primers 5(1):39
Frampton J, Devries JT, Welch TD, Gersh BJ (2020) Modern Management of ST-Segment Elevation Myocardial Infarction. Curr Probl Cardiol 45(3):100393
Gan L, Sun D, Cheng Y, Wang D, Wang F, Wang L, Li W, Shen D, Guo D, Zhang Z, Wang H, Li J, Yang Y, Liang T (2021) Post-operative blood pressure and 3-year major adverse cardiac events in Chinese patients undergoing PCI. BMC Cardiovasc Disord 21(1):623
Otowa K, Kohsaka S, Sawano M, Matsuura S, Chikata A, Maruyama M, Usuda K, Watanabe T, Ishii H, Amano T, Nakamura M, Ikari Y (2022) One-year outcome after percutaneous coronary intervention in nonagenarians: insights from the J-PCI OUTCOME registry. Am Heart J 246:105–116
Ito TK, Yokoyama M, Yoshida Y, Nojima A, Kassai H, Oishi K, Okada S, Kinoshita D, Kobayashi Y, Fruttiger M, Aiba A, Minamino T (2014) A crucial role for CDC42 in senescence-associated inflammation and Atherosclerosis. PLoS ONE 9(7):e102186
Nofer JR, Feuerborn R, Levkau B, Sokoll A, Seedorf U, Assmann G (2003) Involvement of Cdc42 signaling in apoA-I-induced cholesterol efflux. J Biol Chem 278(52):53055–53062
Ridley AJ (2015) Rho GTPase signalling in cell migration. Curr Opin Cell Biol 36:103–112
Feng Q, Guo J, Hou A, Guo Z, Zhang Y, Guo Y, Liu S, Cheng Z, Sun L, Meng L, Han S (2023) The clinical role of serum cell division control 42 in coronary Heart Disease. Scand J Clin Lab Invest 83(1):45–50
Florian MC, Klenk J, Marka G, Soller K, Kiryakos H, Peter R, Herbolsheimer F, Rothenbacher D, Denkinger M, Geiger H (2017) Expression and activity of the small RhoGTPase Cdc42 in blood cells of older adults are Associated with Age and Cardiovascular Disease. J Gerontol A Biol Sci Med Sci 72(9):1196–1200
Zhou M, Wu J, Tan G (2022) The relation of circulating cell division cycle 42 expression with Th1, Th2, and Th17 cells, adhesion molecules, and biochemical indexes in coronary Heart Disease patients. Ir J Med Sci 191(5):2085–2090
Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O’Gara PT, Sabatine MS, Smith PK, Smith SC Jr. (2016) 2016 ACC/AHA Guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary intervention, 2011 ACCF/AHA Guideline for coronary artery bypass graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the management of patients with Non-ST-Elevation Acute Coronary syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular evaluation and management of patients undergoing noncardiac Surgery. Circulation 134(10):e123–e155
Akhtar Z, Aleem MA, Ghosh PK, Islam A, Chowdhury F, MacIntyre CR, Frobert O (2021) In-hospital and 30-day major adverse cardiac events in patients referred for ST-segment elevation Myocardial Infarction in Dhaka, Bangladesh. BMC Cardiovasc Disord 21(1):85
Broman MT, Mehta D, Malik AB (2007) Cdc42 regulates the restoration of endothelial adherens junctions and permeability. Trends Cardiovasc Med 17(5):151–156
Flentje A, Kalsi R, Monahan TS (2019) Small GTPases and their role in Vascular Disease. Int J Mol Sci 20(4)
Cheng X, Ye J, Zhang X, Meng K (2022) Longitudinal variations of CDC42 in patients with Acute Ischemic Stroke during 3-Year period: correlation with CD4(+) T cells, Disease Severity, and prognosis. Front Neurol 13:848933
Uemura A, Fukushima Y (2021) Rho GTPases in Retinal Vascular Diseases. Int J Mol Sci 22(7)
Kologrivova I, Shtatolkina M, Suslova T, Ryabov V (2021) Cells of the Immune System in Cardiac Remodeling: main players in resolution of inflammation and repair after Myocardial Infarction. Front Immunol 12:664457
Damaskos C, Garmpis N, Kollia P, Mitsiopoulos G, Barlampa D, Drosos A, Patsouras A, Gravvanis N, Antoniou V, Litos A, Diamantis E (2020) Assessing Cardiovascular Risk in patients with Diabetes: an update. Curr Cardiol Rev 16(4):266–274
Huang QY, Lai XN, Qian XL, Lv LC, Li J, Duan J, Xiao XH, Xiong LX (2019) Cdc42: a Novel Regulator of insulin secretion and diabetes-Associated Diseases. Int J Mol Sci 20(1):179
Zhang Z, Hirano K, Tsukamoto K, Ikegami C, Koseki M, Saijo K, Ohno T, Sakai N, Hiraoka H, Shimomura I, Yamashita S (2005) Defective cholesterol efflux in Werner syndrome fibroblasts and its phenotypic correction by Cdc42, a RhoGTPase. Exp Gerontol 40(4):286–294
Guo F (2021) RhoA and Cdc42 in T cells: are they targetable for T cell-mediated inflammatory Diseases? Precis Clin Med 4(1):56–61
Abouelmagd K, Tayel H, Atta A, Ladwiniec A, Ibrahim M (2022) Early versus delayed complete revascularisation in patients presenting with ST-segment elevation Myocardial Infarction and multivessel Disease: a systematic review and meta-analysis of randomised controlled trials. Open Heart 9(1)
Bates ER, Tamis-Holland JE, Bittl JA, O’Gara PT, Levine GN (2016) PCI strategies in patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease. J Am Coll Cardiol 68(10):1066–1081
Gul F, Parekh A (2023) Multivessel Disease. StatPearls. Treasure Island (FL) ineligible companies. Akarsh Parekh declares no relevant financial relationships with ineligible companies, Disclosure
Kitahara H, Okada K, Kimura T, Yock PG, Lansky AJ, Popma JJ, Yeung AC, Fitzgerald PJ, Honda Y (2017) Impact of stent size selection on Acute and Long-Term outcomes after Drug-Eluting Stent Implantation in De Novo Coronary lesions. Circ Cardiovasc Interv 10(10)
Stone GW, Maehara A, Ali ZA, Held C, Matsumura M, Kjoller-Hansen L, Botker HE, Maeng M, Engstrom T, Wiseth R, Persson J, Trovik T, Jensen U, James SK, Mintz GS, Dressler O, Crowley A, Ben-Yehuda O, Erlinge D, Investigators PA (2020) Percutaneous coronary intervention for vulnerable coronary atherosclerotic plaque. J Am Coll Cardiol 76(20):2289–2301
Esposito G, Barbato E, Bartunek J (2021) Burden of In-Stent restenosis: shall we. Overcome? Circ Cardiovasc Interv 14(9):e011292
Zhang X, Liu L, Jiang N, Liu Y, Wang Q, Tang X, Zhai Q, Zhao L (2022) Correlation of lipoprotein-associated phospholipase A2 and cerebral microbleeds in patients with acute ischaemic Stroke. BMC Neurol 22(1):482
Zhu Q, Xiao W, Bai Y, Ye P, Luo L, Gao P, Wu H, Bai J (2016) The prognostic value of the plasma N-terminal pro-brain natriuretic peptide level on all-cause death and major cardiovascular events in a community-based population. Clin Interv Aging 11:245–253
Acknowledgements
None.
Funding
We received no funding for this study.
Author information
Authors and Affiliations
Contributions
Shaohua Luan and Lei Zhang designed the experiments. Xiaodan Cheng, Yuanyuan Wang, Qiang Feng and Jinjun Liu collected the data. Shaohua Luan, Lei Zhang, Lei Wei and Fan Jiang analyzed the data. Shaohua Luan, Lei Zhang, Xiaodan Cheng, Yuanyuan Wang, Qiang Feng and Jinjun Liu wrote the manuscript. All authors have reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The Ethics Committee supported this study. All subjects signed the informed consent.
Consent for publication
Not applicable.
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luan, S., Zhang, L., Cheng, X. et al. The ability and optimal cutoff value of serum cell division cycle 42 in estimating major adverse cardiac event in STEMI patients treated with percutaneous coronary intervention. Heart Vessels 39, 277–287 (2024). https://doi.org/10.1007/s00380-023-02350-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-023-02350-w