Abstract
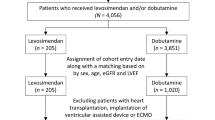
The optimal administration of inotrope after cardiac surgery is unknown. This study aimed to investigate the impact of postoperative inotrope on clinical outcomes in adult elective cardiac surgery patients. Data from the Blood Pressure and Relative Optimal Target after Heart Surgery in Epidemiologic Registry study were analyzed, employing propensity score considering the hospital of admission. The primary outcome was the length of hospital stay evaluated using quantile regression. Secondary outcomes were kidney injury progression, renal replacement therapy, atrial fibrillation, mortality, mechanical ventilation duration, and length of intensive care unit (ICU) stay. Among 870 patients from 14 ICUs in Japan, 535 received inotropes within 24 h of ICU admission, with usage rates ranging from 40 to 100% among facilities. After propensity score matching, 218 patients were included in each group. The inotrope group had a significantly longer hospital stay compared to the control group (16 days vs. 14 days; median difference 1.78 [95% confidence interval [CI] 0.31–3.24]; p = 0.018). However, no significant differences were observed in the secondary outcomes, except for mechanical ventilation duration. The results of the sensitivity analysis using a mixed-effects quantile regression analysis considering the hospital of admission for length of hospital stay in the original cohort were consistent with the results of the propensity analyses (median difference in days, 2.35 [95% CI, 0.35–4.36]; p = 0.022). The use of inotropes within 24 h of ICU admission in adult elective cardiac surgery patients was associated with an extended hospitalization period of approximately 2 days, without offering any prognostic benefit. Clinical trial registration: UMIN-CTR, https://www.umin.ac.jp/ctr/index-j.htm, UMIN000037074.


Similar content being viewed by others
Availability of data and material
The data supporting the findings of this study are available from the corresponding author, TY, upon reasonable request.
References
Gillies M, Bellomo R, Doolan L, Buxton B (2005) Bench-to-bedside review: Inotropic drug therapy after adult cardiac surgery—a systematic literature review. Crit Care 9:266–279
St. André AC, DelRossi A, (2005) Hemodynamic management of patients in the first 24 hours after cardiac surgery. Crit Care Med 33:2082–2093
Bastien O, Vallet B (2005) French multicentre survey on the use of inotropes after cardiac surgery. Crit Care 9:241–242
Hernandez AF, Li S, Dokholyan RS, O’Brien SM, Ferguson TB, Peterson ED (2009) Variation in perioperative vasoactive therapy in cardiovascular surgical care: data from the Society of Thoracic Surgeons. Am Heart J 158:47–52
Shahin J, deVarennes B, Tse CW, Amarica DA, Dial S (2011) The relationship between inotrope exposure, six-hour postoperative physiological variables, hospital mortality and renal dysfunction in patients undergoing cardiac surgery. Crit Care 15:R162
Bendjelid K, Schütz N, Suter PM, Romand JA (2006) Continuous cardiac output monitoring after cardiopulmonary bypass: a comparison with bolus thermodilution measurement. Intensive Care Med 32:919–922
Ball TR, Tricinella AP, Kimbrough BA, Luna S, Gloyna DF, Villamaria FJ, Culp WC Jr (2013) Accuracy of noninvasive estimated continuous cardiac output (esCCO) compared to thermodilution cardiac output: a pilot study in cardiac patients. J Cardiothorac Vasc Anesth 27:1128–1132
Wetterslev M, Møller-Sørensen H, Johansen RR, Perner A (2016) Systematic review of cardiac output measurements by echocardiography vs. thermodilution: the techniques are not interchangeable. Intensive Care Med 42:1223–1233
Wu N-H, Hsieh T-H, Chang C-Y, Shih PC, Kao MC, Lin HY (2023) Validation of cardiac output estimation using the fourth-generation FloTrac/EV1000TM system in patients undergoing robotic-assisted off-pump coronary artery bypass surgery. Heart Vessels 38:341–347
Koponen T, Karttunen J, Musialowicz T, Pietiläinen L, Uusaro A, Lahtinen P (2019) Vasoactive-inotropic score and the prediction of morbidity and mortality after cardiac surgery. Br J Anaesth 122:428–436
Nielsen DV, Hansen MK, Johnsen SP, Hansen M, Hindsholm K, Jakobsen CJ (2014) Health outcomes with and without use of inotropic therapy in cardiac surgery: results of a propensity score-matched analysis. Anesthesiology 120:1098–1108
Weis F, Kilger E, Beiras-Fernandez A, Nassau K, Reuter D, Goetz A, Lamm P, Reindl L, Briegel J (2006) Association between vasopressor dependence and early outcome in patients after cardiac surgery. Anaesthesia 61:938–942
Monaco F, Di Prima AL, Kim JH, Plamondon MJ, Yavorovskiy A, Likhvantsev V, Lomivorotov V, Hajjar LA, Landoni G, Riha H, Farag AMGA, Gazivoda G, Silva FS, Lei C, Bradic N, El-Tahan MR, Bukamal NAR, Sun L, Wang CY (2020) Management of challenging cardiopulmonary bypass separation. J Cardiothorac Vasc Anesth 34:1622–1635
Mebazaa A, Pitsis AA, Rudiger A, Toller W, Longrois D, Ricksten SE, Bobek I, De Hert S, Wieselthaler G, Schirmer U, von Segesser LK, Sander M, Poldermans D, Ranucci M, Karpati PC, Wouters P, Seeberger M, Schmid ER, Weder W, Follath F (2010) Clinical review: practical recommendations on the management of perioperative heart failure in cardiac surgery. Crit Care 14:201
Fellahi J-L, Parienti J-J, Hanouz J-L, Plaud B, Riou B, Ouattara A (2008) Perioperative use of dobutamine in cardiac surgery and adverse cardiac outcome: propensity-adjusted analyses. Anesthesiology 108:979–987
Vail EA, Shieh MS, Pekow PS, Gershengorn HB, Walkey AJ, Lindenauer PK, Wunsch H (2021) Use of vasoactive medications after cardiac surgery in the United States. Ann Am Thorac Soc 18:103–111
Kotani Y, Yoshida T, Kumasawa J, Kamei J, Taguchi A, Kido K, Yamaguchi N, Kariya T, Nakasone M, Mikami N, Koga T, Nakayama I, Shibata M, Yoshida T, Nashiki H, Karatsu S, Nogi K, Tokuhira N, Izawa J (2021) The impact of relative hypotension on acute kidney injury progression after cardiac surgery: a multicenter retrospective cohort study. Ann Intensive Care 11:178
Koga T, Yoshida T, Kotani Y, BROTHER study group (2023) Association between the intraoperative fluid balance during cardiac surgery and postoperative sequential organ failure assessment score: a post hoc analysis of the BROTHER study, a retrospective multicenter cohort study. Heart Vessels. https://doi.org/10.1007/s00380-023-02306-0
Kellum JA, Lameire N, KDIGO AKI Guideline Work Group (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care 17:204
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424
Franco RA, de Almeida JP, Landoni G, Scheeren TWL, Galas FRBG, Fukushima JT, Zefferino S, Nardelli P, de Albuquerque PM, Arita ECTC, Park CHL, Cunha LCC, de Oliveira GQ, Costa IBSDS, Kalil Filho R, Jatene FB, Hajjar LA (2021) Dobutamine-sparing versus dobutamine-to-all strategy in cardiac surgery: a randomized noninferiority trial. Ann Intensive Care 11:15
Barone JE, Tucker JB, Rassias D, Corvo PR (2001) Routine perioperative pulmonary artery catheterization has no effect on rate of complications in vascular surgery: a meta-analysis. Am Surg 67:674–679
Schwann NM, Hillel Z, Hoeft A, Barash P, Möhnle P, Miao Y, Mangano DT (2011) Lack of effectiveness of the pulmonary artery catheter in cardiac surgery. Anesth Analg 113:994–1002
Rajaram SS, Desai NK, Kalra A, Gajera M, Cavanaugh SK, Brampton W, Young D, Harvey S, Rowan K (2013) Pulmonary artery catheters for adult patients in intensive care. Cochrane database Syst Rev 2013(2):CD003408. https://doi.org/10.1002/14651858.CD003408.pub3
Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, Brampton W, Williams D, Young D, Rowan K, PAC-Man study collaboration (2005) Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet 366:472–477
Shah MR, Hasselblad V, Stevenson LW, Binanay C, O’Connor CM, Sopko G, Califf RM (2005) Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA 294:1664–1670
Yanatori M, Tomita S, Miura Y, Ueno Y (2007) Feasibility of the fast-track recovery program after cardiac surgery in Japan. Gen Thorac Cardiovasc Surg 55:445–449
Shibasaki I, Ouchi M, Fukuda T, Tsuchiya G, Ogawa H, Takei Y, Tezuka M, Kanazawa Y, Katayanagi S, Nozawa N, Mizushima T, Toyoda S, Fukuda H, Nakajima T (2022) Effect of sarcopenia on hospital stay from post cardiac surgery to discharge. Int J Cardiol Hear Vasc 39:101003
Kobayashi J, Kusachi S, Sawa Y, Motomura N, Imoto Y, Makuuchi H, Tanemoto K, Shimahara Y, Sumiyama Y (2015) Socioeconomic effects of surgical site infection after cardiac surgery in Japan. Surg Today 45:422–428
Tatsuishi W, Kumamaru H, Nakano K, Miyata H, Motomura N (2021) Evaluation of postoperative outcomes of valve reoperation: a retrospective study. Eur J Cardiothorac Surg 59:869–877
Acknowledgements
We would like to thank all colleagues in the BROTHER study participating hospitals who performed the extensive data entry. The BROTHER study group: Kameda Medical Center: Yuki Kotani; Jikei University School of Medicine: Takahiro Koga; Okinawa Chubu Hospital: Izumi Nakayama; Tottori University Faculty of Medicine: Masato Nakasone; Wakayama Medical University: Mami Shibata; Hokkaido University Hospital: Tomonao Yoshida; Kobe City Medical Center General Hospital: Akihisa Taguchi, Daisuke Kawakami; Hirosaki University Graduate School of Medicine: Noriko Mikami, Junichi Saito, Mirei Kubota, Tsubasa Oyama; Kurashiki Central Hospital: Jun Kamei; Yokohama City Minato Red Cross Hospital: Isao Nagata, Shinsuke Karatsu; Tokyo Bay Urayasu Ichikawa Medical Center: Naoki Yamaguchi; Yokohama City University Hospital: Takayuki Kariya; Iwate Prefectural Central Hospital: Hiroshi Nashiki; and Hiroshima Citizens Hospital, Hiroshima: Koji Kido, Hiroki Omiya.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Contributions
TY had full access to all data in the study and takes responsibility for the integrity of the data. Study concept and design: TY, TM, SS, YK, and AG. Acquisition of data: TY and YK. Analysis and interpretation of data: TY, TM, SS, YK, and AG. Drafting of the manuscript: TY. Critical revision of the manuscript for important intellectual content: TY, TM, SS, YK, and AG.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethics approval and consent to participate
The ethics committee of Kameda Medical Center approved this study (No. 19–013), and all the ethics committees of the participating hospitals approved an opt-out method of informed consent. As this was a retrospective cohort study, we applied the opt-out method of informed consent for participation.
Consent for publication
As this was a retrospective cohort study, we applied the opt-out method of informed consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the BROTHER study group are mentioned in Acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoshida, T., Goto, A., Shinoda, S. et al. The epidemiology of postoperative dobutamine and phosphodiesterase inhibitors after adult elective cardiac surgery and its impact on the length of hospital stay: a post hoc analysis from the multicenter retrospective observational study. Heart Vessels 39, 438–445 (2024). https://doi.org/10.1007/s00380-023-02349-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-023-02349-3