Abstract
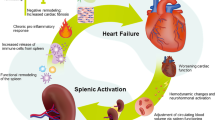
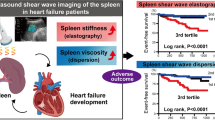
The spleen is an important immune organ that releases erythrocytes and monocytes and destroys aged platelets. It also reserves 20–30% of the total blood volume, and its size decreases in hypovolemic shock. However, the clinical significance of splenic size in patients with heart failure (HF) remains unclear. We retrospectively analyzed the data of 206 patients with clinically stable HF gathered between January 2001 and August 2020 and recorded in a single-center registry. All patients underwent right heart catheterization and computed tomography (CT). Splenic size was measured using CT volumetry. The primary outcomes were composite cardiac events occurring for the first time during follow-up, namely, cardiac death and hospitalization for worsening HF. The median splenic volume and splenic volume index (SVI) were 118.0 mL and 68.9 mL/m2, respectively. SVI was positively correlated with cardiac output (r = 0.269, P < 0.001) and stroke volume (r = 0.228, P = 0.002), and negatively correlated with systemic vascular resistance (r = − 0.302, P < 0.001). Seventy cardiac events occurred, and the optimal receiver operating characteristic curve SVI cutoff value for predicting cardiac events was 68.9 mL/m2. The median blood adrenaline concentration was higher in the low-SVI group than the high-SVI group (0.039 ng/mL vs. 0.026 ng/mL, respectively; P = 0.004), and the low-SVI group experienced more cardiac events (log-rank test, P < 0.001). Multivariate Cox proportional hazards regression revealed that a low SVI was an independent predictor of cardiac events, even when adjusted for the validated HF risk score, blood–brain natriuretic peptide concentration, blood catecholamine concentrations, and hemodynamic parameters. Splenic size reflects hemodynamics, including systemic circulating blood volume status and sympathetic nerve activity, and is associated with HF prognosis.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Hamza SM, Kaufman S (2009) Role of spleen in integrated control of splanchnic vascular tone: physiology and pathophysiology. Can J Physiol Pharmacol 87:1–7
Mebius RE, Kraal G (2005) Structure and function of the spleen. Nat Rev Immunol 5:606–616
Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, Figueiredo JL, Kohler RH, Chudnovskiy A, Waterman P, Aikawa E, Mempel TR, Libby P, Weissleder R, Pittet MJ (2009) Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science 325:612–616
Kaneko J, Sugawara Y, Matsui Y, Ohkubo T, Makuuchi M (2002) Normal splenic volume in adults by computed tomography. Hepatogastroenterology 49:1726–1727
Caglar V, Alkoc OA, Serdaroglu O, Ozen OA (2014) Determination of normal splenic volume in relation to age, gender and body habitus: a stereological study on computed tomography. Folia Morphol (Warsz) 73:331–338
Chow KU, Luxembourg B, Seifried E, Bonig H (2016) Spleen size is significantly influenced by body height and sex: establishment of normal values for spleen size at US with a cohort of 1200 healthy individuals. Radiology 279:306–313
Tonelli AR, Yadav R, Gupta A, Arrossi AV, Heresi GA, Dweik RA (2013) Spleen size in idiopathic and heritable pulmonary arterial hypertension. Respiration 85:391–399
Jahng JW, Song E, Sweeney G (2016) Crosstalk between the heart and peripheral organs in heart failure. Exp Mol Med 48:e217
Rubio-Gracia J, Giménez-López I, Sánchez-Martelez M, Josa-Laorden C, Pérez-Calvo JI (2020) Intra-abdominal pressure and its relationship with markers of congestion in patients admitted for acute decompensated heart failure. Heart Vessels 35:1545–1556
Aizawa Y, Okumura Y, Saito Y, Ikeya Y, Nakai T, Arima K (2020) Association of renal resistance index and arterial stiffness on clinical outcomes in patients with mild-to-moderate renal dysfunction and presence or absence of heart failure with preserved ejection fraction. Heart Vessels 35:1699–1708
Kimura H, Hiramitsu S, Miyagishima K, Mori K, Yoda R, Kato S, Kato Y, Morimoto SI, Hishida H, Ozaki Y (2010) Cardio-renal interaction: impact of renal function and anemia on the outcome of chronic heart failure. Heart Vessels 25:306–312
Omote K, Nagai T, Asakawa N, Kamiya K, Tokuda Y, Aikawa T, Fukushima A, Noguchi K, Kato Y, Komoriyama H, Nishida M, Kudo Y, Iwano H, Yokota T, Anzai T (2019) Impact of admission liver stiffness on long-term clinical outcomes in patients with acute decompensated heart failure. Heart Vessels 34:984–991
Maeda D, Sakane K, Ito T, Kanzaki Y, Sohmiya K, Hoshiga M (2020) Fibrosis-4 index reflects right-sided filling pressure in patients with heart failure. Heart Vessels 35:376–383
Ismahil MA, Hamid T, Bansal SS, Patel B, Kingery JR, Prabhu SD (2014) Remodeling of the mononuclear phagocyte network underlies chronic inflammation and disease progression in heart failure: critical importance of the cardiosplenic axis. Circ Res 114:266–282
Emami H, Singh P, MacNabb M, Vucic E, Lavender Z, Rudd JHF, Fayad ZA, Lehrer-Graiwer J, Korsgren M, Figueroa AL, Fredrickson J, Rubin B, Hoffmann U, Truong QA, Min JK, Baruch A, Nasir K, Nahrendorf M, Tawakol A (2015) Splenic metabolic activity predicts risk of future cardiovascular events: demonstration of a cardiosplenic axis in humans. JACC Cardiovasc Imaging 8:121–130
Fujinami M, Kondo H, Yufu K, Shinohara T, Ishii Y, Teshima Y, Nakagawa M, Takahashi N (2018) Association between the baseline peripheral blood monocyte counts, the size of spleen, and the response to cardiac resynchronization therapy. J Cardiol 71:299–304
Hiraiwa H, Okumura T, Sawamura A, Kondo T, Kazama S, Kimura Y, Shibata N, Arao Y, Oishi H, Kato H, Kuwayama T, Yamaguchi S, Furusawa K, Morimoto R, Murohara T (2020) Spleen size improvement in advanced heart failure patients using a left ventricular assist device. Artif Organs 44:700–708
Hiraiwa H, Okumura T, Sawamura A, Kondo T, Kazama S, Kimura Y, Shibata N, Arao Y, Oishi H, Kato H, Kuwayama T, Yamaguchi S, Furusawa K, Morimoto R, Fujimoto K, Mutsuga M, Usui A, Murohara T (2021) Association between splenic volume and pulsatility index in patients with left ventricular assist devices. Int J Artif Organs 44:282–287
Maeda D, Sakane K, Kanzaki Y, Horai R, Akamatsu K, Tsuda K, Ito T, Sohmiya K, Hoshiga M (2021) Splenic volume index determined using computed tomography upon admission is associated with readmission for heart failure among patients with acute decompensated heart failure. Int Heart J 62:584–591
Saito Y, Matsumoto N, Aizawa Y, Fukamachi D, Kitano D, Kazuto T, Tamaki T, Fujito H, Sezai A, Okumura Y (2020) Clinical significance of spleen stiffness in patients with acute decompensated heart failure. ESC Heart Fail 7:4005–4014
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, Hollenberg SM, Lindenfeld J, Masoudi FA, McBride PE, Peterson PN, Stevenson LW, Westlake C (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 70:776–803
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzáles-Juanetey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, ESC Scientific Document Group (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200
Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL, Douglas PS, Faxon DP, Gillam LD, Kimball TR, Kussmaul WG, Pearlman AS, Philbrick JT, Rakowski H, Thys DM, Antman EM, Smith SC Jr, Alpert JS, Gregoratos G, Anderson JL, Hiratzka LF, Hunt SA, Fuster V, Jacobs AK, Gibbons RJ, Russell RO (2003) ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (ACC/AHA/ASE committee to update the 1997 guidelines for the clinical application of echocardiography). J Am Coll Cardiol 42:954–970
Pocock SJ, Ariti CA, McMurray JJV, Maggioni A, Køber L, Squire IB, Swedberg K, Dobson J, Poppe KK, Whalley GA, Doughty RN, Meta-Analysis Global Group in Chronic Heart Failure (2013) Predicting survival in heart failure: a risk score based on 39 372 patients from 30 studies. Eur Heart J 34:1404–1413
Borlaug BA, Kass DA (2011) Invasive hemodynamic assessment in heart failure. Cardiol Clin 29:269–80
Corradi F, Brusasco C, Garlaschi A, Santori G, Vezzani A, Moscatelli P, Pelosi P (2012) Splenic Doppler resistive index for early detection of occult hemorrhagic shock after polytrauma in adult patients. Shock 38:466–473
Kiguchi T, Higuchi T, Takahashi N, Shimokoshi T, Yamazaki M, Yoshimira N, Aoyama H (2015) CT measurement of splenic volume changes as a result of hypovolemic shock. Jpn J Radiol 33:645–649
Cruz-Romero C, Agarwal S, Abujudeh HH, Thrall J, Hahn PF (2016) Spleen volume on CT and the effect of abdominal trauma. Emerg Radiol 23:315–323
Enslow MS, Preece SR, Wildman-Tobriner B, Enslow RA, Mazurowski M, Nelson RC (2018) Splenic contraction: a new member of the hypovolemic shock complex. Abdom Radiol 43:2375–2383
Ayers AB, Davies BN, Withrington PG (1972) Responses of the isolated, perfused human spleen to sympathetic nerve stimulation, catecholamines and polypeptides. Br J Pharmacol 44:17–30
Kaufman MJ, Siegel AJ, Mendelson JH, Rose SL, Kukes TJ, Sholar MB, Lukas SE, Renshaw PF (1985) Cocaine administration induces human splenic constriction and altered hematologic parameters. J Appl Physiol 85:1877–1883
Silagy C, Shelby-James T, Sage M, Wallage A (1998) Patient-detected diurnal changes in spleen volume. Lancet 352:710
Bakovic D, Pivac N, Zubin Maslov P, Breskovic T, Damonja G, Dujic Z (2013) Spleen volume changes during adrenergic stimulation with low doses of epinephrine. J Physiol Pharmacol 64:649–655
Triposkiadis F, Karayannis G, Giamouzis G, Skoularigis J, Louridas G, Butler J (2009) The sympathetic nervous system in heart failure physiology, pathophysiology, and clinical implications. J Am Coll Cardiol 54:1747–1762
Smith GL, Lichtman JH, Bracken MB, Shlipak MG, Phillips CO, DiCapua P, Krumholz HM (2006) Renal impairment and outcomes in heart failure: systematic review and meta-analysis. J Am Coll Cardiol 47:1987–1996
Komukai K, Ogawa T, Yagi H, Date T, Sakamoto H, Kanzaki Y, Shibayama K, Hashimoto K, Inada K, Minai K, Ogawa K, Kosuga T, Kawai M, Hongo K, Taniguchi I, Yoshimura M (2008) Decreased renal function as an independent predictor of re-hospitalization for congestive heart failure. Circ J 72:1152–1157
Schefold JC, Filippatos G, Hasenfuss G, Anker SD, von Haehling S (2016) Heart failure and kidney dysfunction: epidemiology, mechanisms and management. Nat Rev Nephrol 12:610–623
Damman K, Navis G, Voors AA, Asselbergs FW, Smilde TDJ, Cleland JGF, van Veldhuisen DJ, Hillege HL (2007) Worsening renal function and prognosis in heart failure: systematic review and meta-analysis. J Card Fail 13:599–608
Ahmad T, Jackson K, Rao VS, Wilson Tang WH, Brisco-Bacik MA, Chen HH, Felker GM, Hernandez AF, O’Connor CM, Sabbisetti VS, Bonventre JV, Wilson FP, Coca SG, Testani JM (2018) Worsening renal function in patients with acute heart failure undergoing aggressive diuresis is not associated with tubular injury. Circulation 137:2016–2028
Schagatay E, Lunde A, Nilsson S, Palm O, Lodin-Sundström A (2020) Spleen contraction elevates hemoglobin concentration at high altitude during rest and exercise. Eur J Appl Physiol 120:2693–2704
Kuwahira I, Kamiya U, Iwamoto T, Moue Y, Urano T, Ohta Y, Gonzalez NC (1999) Splenic contraction-induced reversible increase in hemoglobin concentration in intermittent hypoxia. J Appl Physiol 86:181–187
Jung M, Riley P, Drozdzewski A, Pressler SJ (2017) Mild to moderate hypoxemia among stable heart failure patients with reduced ejection fraction: 24-hour oxygen monitoring. J Card Fail 23:S81
Pozo AL, Godfrey EM, Bowles KM (2009) Splenomegaly: investigation, diagnosis and management. Blood Rev 23:105–111
Schagatay E, Hubinette A, Lodin-Sundström A, Engan H, Stenfors N (2015) Exercise induced hemoconcentration following spleen contraction in subjects with COPD. COPD Res Pract 1:13
Acknowledgements
None.
Funding
This research was supported in part by Grant-in-Aid for Scientific Research of the Japan Society for the Promotion of Science (JSPS KAKENHI [grant numbers JP21K16085 to H.H. and JP19K17592 to T.O.]).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
TO received research grants from Ono Pharmaceutical Co. Ltd., Bayer Pharmaceutical Co. Ltd., Daiichi-Sankyo Pharma Inc., and Amgen Astellas BioPharma KK outside of the submitted work. TO received honorariums from Ono Pharmaceutical Co. Ltd., Otsuka Pharmaceutical Co. Ltd., Novartis Pharma KK, and Medtronic Japan Co. Ltd. TM received lecture fees from Bayer Pharmaceutical Co. Ltd., Daiichi-Sankyo Co. Ltd., Sumitomo Dainippon Pharma Co. Ltd., Kowa Co. Ltd., MSD KK, Mitsubishi Tanabe Pharma Co., Nippon Boehringer Ingelheim Co. Ltd., Novartis Pharma KK, Pfizer Japan Inc., Sanofi-Aventis KK, and Takeda Pharmaceutical Co. Ltd. TM received an unrestricted research grant for the Department of Cardiology, Nagoya University Graduate School of Medicine from Astellas Pharma Inc., Daiichi-Sankyo Co. Ltd., Sumitomo Dainippon Pharma Co. Ltd., Kowa Co. Ltd., MSD KK, Mitsubishi Tanabe Pharma Co., Nippon Boehringer Ingelheim Co. Ltd., Novartis Pharma KK, Otsuka Pharma Ltd., Pfizer Japan Inc., Sanofi-Aventis KK, Takeda Pharmaceutical Co. Ltd., and Teijin Pharma Ltd. The remaining authors have no conflicts of interest relevant to this article to disclose.
Ethics approval
The study protocol complied with the Declaration of Helsinki, and the protocol was approved by the ethics review board of our institution.
Consent to participate
Written informed consent was obtained from all patients for participation.
Consent to publish
Written informed consent was obtained from all patients for publication of data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hiraiwa, H., Okumura, T., Sawamura, A. et al. Splenic size as an indicator of hemodynamics and prognosis in patients with heart failure. Heart Vessels 37, 1344–1355 (2022). https://doi.org/10.1007/s00380-022-02030-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02030-1