Abstract
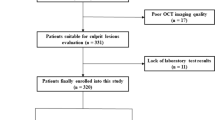
A low ratio of eicosapentaenoic acid to arachidonic acid (EPA/AA) has been demonstrated to be associated with a higher risk of cardiovascular events. Optical coherence tomography (OCT) is useful for the assessment of coronary plaque vulnerability. The purpose of this study was to evaluate the association between EPA/AA ratio and coronary plaque vulnerability. This study involved 58 patients with stable angina pectoris undergoing percutaneous coronary intervention. OCT image acquisition was performed before the procedure in the culprit lesions. We assessed lipid-rich plaque length and arc, fibrous cap thickness, frequency of thin-cap fibroatheroma (TCFA), thrombus, ruptured plaque, macrophage infiltration, and microvessels using OCT. Patients were divided into two groups according to the median value of serum EPA/AA ratio: a low-EPA/AA group (n = 29, EPA/AA ratio <0.36) and a high-EPA/AA group (n = 29, EPA/AA ratio ≥0.36). In qualitative analyses, TCFA (35.4 vs 6.9 %, P = 0.0095), macrophage infiltration (48.3 vs 13.8 %, P = 0.0045), and microvessels (44.8 vs 10.3 %, P = 0.0033) were more frequently observed in the low-EPA/AA group. In quantitative analyses, the low-EPA/AA group had wider maximum lipid arc (114.0 ± 94.8° vs 56.4 ± 66.0°, P = 0.0097), longer lipid length (4.8 ± 4.5 vs 1.6 ± 2.6 mm, P = 0.0037), and thinner fibrous cap (69.3 ± 28.3 vs 113.3 ± 46.6 μm, P = 0.005) compared with the high-EPA/AA group. EPA/AA ratio was positively correlated with fibrous cap thickness (r = 0.46, P = 0.007). In a multivariate model, an EPA/AA ratio <0.36 was associated with the presence of TCFA (odds ratio 6.41, 95 % confidence interval 1.11–61.91, P = 0.0371). In our detailed OCT analysis, lower EPA/AA ratio was associated with higher vulnerability of coronary plaques to rupture.


Similar content being viewed by others
References
Deedwania P, Stone PH, Bairey Merz CN, Cosin-Aguilar J, Koylan N, Luo D, Ouyang P, Piotrowicz R, Schenck-Gustafsson K, Sellier P, Stein JH, Thompson PL, Tzivoni D (2007) Effects of intensive versus moderate lipid-lowering therapy on myocardial ischemia in older patients with coronary heart disease: results of the Study Assessing Goals in the Elderly (SAGE). Circulation 115:700–707
LaRosa JC, Grundy SM, Waters DD, Shear C, Barter P, Fruchart JC, Gotto AM, Greten H, Kastelein JJ, Shepherd J, Wenger NK, Treating to New Targets Investigators (2005) Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 352:1425–1435
Lauderdale SA, Sheehan AH (2005) Intensive lipid-lowering therapy in patients with coronary heart disease. Ann Pharmacother 39:329–334
Nakamura T, Azuma A, Kuribayashi T, Sugihara H, Okuda S, Nakagawa M (2003) Serum fatty acid levels, dietary style and coronary heart disease in three neighbouring areas in Japan: the Kumihama study. Br J Nutr 89:267–272
Domei T, Yokoi H, Kuramitsu S, Soga Y, Arita T, Ando K, Shirai S, Kondo K, Sakai K, Goya M, Iwabuchi M, Ueeda M, Nobuyoshi M (2012) Ratio of serum n-3 to n-6 polyunsaturated fatty acids and the incidence of major adverse cardiac events in patients undergoing percutaneous coronary intervention. Circ J 76:423–429
Ueeda M, Doumei T, Takaya Y, Ohnishi N, Takaishi A, Hirohata S, Miyoshi T, Shinohata R, Usui S, Kusachi S (2011) Association of serum levels of arachidonic acid and eicosapentaenoic acid with prevalence of major adverse cardiac events after acute myocardial infarction. Heart Vessels 26:145–152
Yokoyama M, Origasa H, Matsuzaki M, Matsuzawa Y, Saito Y, Ishikawa Y, Oikawa S, Sasaki J, Hishida H, Itakura H, Kita T, Kitabatake A, Nakaya N, Sakata T, Shimada K, Shirato K (2007) Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet 369:1090–1098
Hansson GK (2005) Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 352:1685–1695
Stoll G, Bendszus M (2006) Inflammation and atherosclerosis: novel insights into plaque formation and destabilization. Stroke 37:1923–1932
Libby P (2012) Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol 32:2045–2051
Calder PC (2012) The role of marine omega-3 (n-3) fatty acids in inflammatory processes, atherosclerosis and plaque stability. Mol Nutr Food Res 56:1073–1080
Onuma Y, Serruys PW, Perkins LE, Okamura T, Gonzalo N, Garcia–Garcia HM, Regar E, Kamberi M, Powers JC, Rapoza R, van Beusekom H, van der Giessen W, Virmani R (2010) Intracoronary optical coherence tomography and histology at 1 month and 2, 3, and 4 years after implantation of everolimus-eluting bioresorbable vascular scaffolds in a porcine coronary artery model: an attempt to decipher the human optical coherence tomography images in the ABSORB trial. Circulation 122:2288–2300
Takarada S, Imanishi T, Liu Y, Ikejima H, Tsujioka H, Kuroi A, Ishibashi K, Komukai K, Tanimoto T, Ino Y, Kitabata H, Kubo T, Nakamura N, Hirata K, Tanaka A, Mizukoshi M, Akasaka T (2010) Advantage of next-generation frequency-domain optical coherence tomography compared with conventional time-domain system in the assessment of coronary lesion. Catheter Cardiovasc Interv 75:202–206
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, Bouma B, Bruining N, Cho JM, Chowdhary S, Costa MA, de Silva R, Dijkstra J, Di Mario C, Dudek D, Falk E, Feldman MD, Fitzgerald P, Garcia-Garcia HM, Gonzalo N, Granada JF, Guagliumi G, Holm NR, Honda Y, Ikeno F, Kawasaki M, Kochman J, Koltowski L, Kubo T, Kume T, Kyono H, Lam CC, Lamouche G, Lee DP, Leon MB, Maehara A, Manfrini O, Mintz GS, Mizuno K, Morel MA, Nadkarni S, Okura H, Otake H, Pietrasik A, Prati F, Raber L, Radu MD, Rieber J, Riga M, Rollins A, Rosenberg M, Sirbu V, Serruys PW, Shimada K, Shinke T, Shite J, Siegel E, Sonoda S, Suter M, Takarada S, Tanaka A, Terashima M, Thim T, Uemura S, Ughi GJ, van Beusekom HM, van der Steen AF, van Es GA, van Soest G, Virmani R, Waxman S, Weissman NJ, Weisz G, International Working Group for Intravascular Optical Coherence Tomography (2012) Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol 59:1058–1072
Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico (1999) Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 354:447–455
Albert CM, Campos H, Stampfer MJ, Ridker PM, Manson JE, Willett WC, Ma J (2002) Blood levels of long-chain n-3 fatty acids and the risk of sudden death. N Engl J Med 346:1113–1118
van der Wal AC, Becker AE, van der Loos CM, Das PK (1994) Site of intimal rupture or erosion of thrombosed coronary atherosclerotic plaques is characterized by an inflammatory process irrespective of the dominant plaque morphology. Circulation 89:36–44
Bogaty P, Poirier P, Simard S, Boyer L, Solymoss S, Dagenais GR (2001) Biological profiles in subjects with recurrent acute coronary events compared with subjects with long-standing stable angina. Circulation 103:3062–3068
Matsumoto M, Sata M, Fukuda D, Tanaka K, Soma M, Hirata Y, Nagai R (2008) Orally administered eicosapentaenoic acid reduces and stabilizes atherosclerotic lesions in ApoE-deficient mice. Atherosclerosis 197:524–533
Thies F, Garry JM, Yaqoob P, Rerkasem K, Williams J, Shearman CP, Gallagher PJ, Calder PC, Grimble RF (2003) Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet 361:477–485
Virmani R (2011) Are our tools for the identification of TCFA ready and do we know them? JACC Cardiovasc Imaging 4:656–658
Kusama I, Hibi K, Kosuge M, Sumita S, Tsukahara K, Okuda J, Ebina T, Umemura S, Kimura K (2012) Intravascular ultrasound assessment of the association between spatial orientation of ruptured coronary plaques and remodeling morphology of culprit plaques in ST-elevation acute myocardial infarction. Heart Vessels 27:541–547
Hallenbeck JM, Hansson GK, Becker KJ (2005) Immunology of ischemic vascular disease: plaque to attack. Trends Immunol 26:550–556
Calder PC (2003) N-3 polyunsaturated fatty acids and inflammation: from molecular biology to the clinic. Lipids 38:343–352
Calder PC (2006) n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am J Clin Nutr 83:1505S–1519S
Kashiyama T, Ueda Y, Nemoto T, Wada M, Masumura Y, Matsuo K, Nishio M, Hirata A, Asai M, Kashiwase K, Kodama K (2011) Relationship between coronary plaque vulnerability and serum n-3/n-6 polyunsaturated fatty acid ratio. Circ J 75:2432–2438
Ogita M, Miyauchi K, Miyazaki T, Naito R, Konishi H, Tsuboi S, Dohi T, Kasai T, Yokoyama T, Okazaki S, Kurata T, Daida H (2013) Low high-density lipoprotein cholesterol is a residual risk factor associated with long-term clinical outcomes in diabetic patients with stable coronary artery disease who achieve optimal control of low-density lipoprotein cholesterol. Heart Vessels. doi:10.1007/s00380-011-0205-6
Kurisu S, Ishibashi K, Kato Y, Mitsuba N, Dohi Y, Nishioka K, Kihara Y (2013) Effects of lipid-lowering therapy with strong statin on serum polyunsaturated fatty acid levels in patients with coronary artery disease. Heart Vessels 28:34–38
Conflict of interest
There are no conflicts of interest to disclose in connection with any commercial associations for any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hasegawa, T., Otsuka, K., Iguchi, T. et al. Serum n-3 to n-6 polyunsaturated fatty acids ratio correlates with coronary plaque vulnerability: an optical coherence tomography study. Heart Vessels 29, 596–602 (2014). https://doi.org/10.1007/s00380-013-0404-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-013-0404-4