Abstract
Purpose
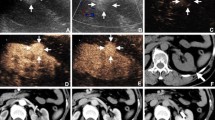
To evaluate the diagnostic performance of contrast-enhanced (CE) ultrasound using Sonazoid (SNZ–CEUS) by comparing with contrast-enhanced computed tomography (CE–CT) and contrast-enhanced magnetic resonance imaging (CE–MRI) for differentiating benign and malignant renal masses.
Materials and methods
306 consecutive patients (from 7 centers) with renal masses (40 benign tumors, 266 malignant tumors) diagnosed by both SNZ–CEUS, CE–CT or CE–MRI were enrolled between September 2020 and February 2021. The examinations were performed within 7 days, but the sequence was not fixed. Histologic results were available for 301 of 306 (98.37%) lesions and 5 lesions were considered benign after at least 2 year follow-up without change in size and image characteristics. The diagnostic performances were evaluated by sensitivity, specificity, positive predictive value, negative predictive value, and compared by McNemar’s test.
Results
In the head-to-head comparison, SNZ–CEUS and CE–MRI had comparable sensitivity (95.60 vs. 94.51%, P = 0.997), specificity (65.22 vs. 73.91%, P = 0.752), positive predictive value (91.58 vs. 93.48%) and negative predictive value (78.95 vs. 77.27%); SNZ–CEUS and CE–CT showed similar sensitivity (97.31 vs. 96.24%, P = 0.724); however, SNZ–CEUS had relatively lower than specificity than CE–CT (59.09 vs. 68.18%, P = 0.683). For nodules > 4 cm, CE–MRI demonstrated higher specificity than SNZ–CEUS (90.91 vs. 72.73%, P = 0.617) without compromise the sensitivity.
Conclusions
SNZ–CEUS, CE–CT, and CE–MRI demonstrate desirable and comparable sensitivity for the differentiation of renal mass. However, the specificity of all three imaging modalities is not satisfactory. SNZ–CEUS may be a suitable alternative modality for patients with renal dysfunction and those allergic to gadolinium or iodine-based agents.
Key Points
-
This prospective multicenter study demonstrated that the diagnostic performance of SNZ–CEUS was comparable to CE–CT and CE–MRI.
-
The three imaging modalities displayed desirable sensitivity, while the specificity needs to be further improved.
-
CE–MRI may have better specificity than SNZ–CEUS for differentiating renal masses bigger than 4 cm

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Data availability
The article does not contain applicable data availability statements.
Change history
13 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00345-024-05075-1
Abbreviations
- ALMs:
-
Angioleiomyomas
- BMI:
-
Body mass index
- ccRCC:
-
Clear-cell RCC
- CE:
-
Contrast-enhanced
- CE–CT:
-
Contrast-enhanced computed tomography
- CE–MRI:
-
Contrast-enhanced magnetic resonance imaging
- CEUS:
-
Contrast-enhanced ultrasound
- EAU:
-
European Association of Urology
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- RCC:
-
Renal cell carcinoma
- SNZ–CEUS:
-
Contrast-enhanced ultrasound using Sonazoid
- TFE3:
-
Transcription factor e3
References
Siegel RL, Miller KD, Fuchs HE et al (2021) Cancer statistics, 2021. CA Cancer J Clin 71:7
Ferlay J, Colombet M, Soerjomataram I et al (2018) Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 103:356
Ljungberg B, Bensalah K, Canfield S et al (2015) EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67:913
Song XD, Tian YN, Li H et al (2020) Research progress on advanced renal cell carcinoma. J Int Med Res 48:300060520924265
Barr RG, Peterson C, Hindi A (2014) Evaluation of indeterminate renal masses with contrast-enhanced US: a diagnostic performance study. Radiology 271:133
Kazmierski B, Deurdulian C, Tchelepi H et al (2018) Applications of contrast-enhanced ultrasound in the kidney. Abdom Radiol 43:880
Bertolotto M, Bucci S, Valentino M et al (2018) Contrast-enhanced ultrasound for characterizing renal masses. Eur J Radiol 105:41
Tsuruoka K, Yasuda T, Koitabashi K et al (2010) Evaluation of renal microcirculation by contrast-enhanced ultrasound with Sonazoid as a contrast agent. Int Heart J 51:176
Miyoshi T, Okayama H, Hiasa G et al (2016) Contrast-enhanced ultrasound for the evaluation of acute renal infarction. J Med Ultrason 43(141):2016
Siedlecki AM, Benson C, Frates M et al (2019) First report of perfluorobutane microsphere-enhanced ultrasound in the transplant kidney. Transplantation 103:e283
Davenport MS, Cohan RH, Ellis JH (2015) Contrast media controversies in 2015: imaging patients with renal impairment or risk of contrast reaction. AJR Am J Roentgenol 204:1174
Shen L, Li Y, Li N et al (2019) Clinical utility of contrast-enhanced ultrasonography in the diagnosis of benign and malignant small renal masses among Asian population. Cancer Med 8:7532
Furrer MA, Spycher SCJ, Büttiker SM et al (2020) Comparison of the diagnostic performance of contrast-enhanced ultrasound with that of contrast-enhanced computed tomography and contrast-enhanced magnetic resonance imaging in the evaluation of renal masses: a systematic review and meta-analysis. Eur Urol Oncol 3:464
Cai Y, Du L, Li F et al (2014) Quantification of enhancement of renal parenchymal masses with contrast-enhanced ultrasound. Ultrasound Med Biol 40:1387
Ascenti G, Zimbaro G, Mazziotti S et al (2001) Usefulness of power doppler and contrast-enhanced sonography in the differentiation of hyperechoic renal masses. Abdom Imaging 26:654
Lu Q, Huang BJ, Wang WP et al (2015) Qualitative and quantitative analysis with contrast-enhanced ultrasonography: diagnosis value in hypoechoic renal angiomyolipoma. Korean J Radiol 16:334
Ignee A, Straub B, Schuessler G et al (2010) Contrast enhanced ultrasound of renal masses. World J Radiol 2:15
Aoki S, Hattori R, Yamamoto T et al (2011) Contrast-enhanced ultrasound using a time-intensity curve for the diagnosis of renal cell carcinoma. BJU Int 108:349
Gassert F, Schnitzer M, Kim SH et al (2021) Comparison of magnetic resonance imaging and contrast-enhanced ultrasound as diagnostic options for unclear cystic renal lesions: a cost-effectiveness analysis. Ultraschall Med 42:411
Zhao P, Zhu J, Wang L et al (2023) Comparative diagnostic performance of contrast-enhanced ultrasound and dynamic contrast-enhanced magnetic resonance imaging for differentiating clear cell and non-clear cell renal cell carcinoma. Eur Radiol 33:3766
Funding
This work was supported by Grants 81871374 and 82171941, 91859201 and 82030047 from the National Scientific Foundation Committee of China. The funders had no role in data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Concept and design: Ping Liang, Zhi-gang Cheng. Experiments and procedures: All authors. Writing of article: Qin-xian Zhao, Yang Bai. Statistical analysis: Qin-xian Zhao, Yang Bai, Ming-jing Mei; Case collection: Qin-xian Zhao, Chong Wu, Hai-xiang Zhang, Mei-mei Zhu, Xiang-ru Dong, Hua Liang, Si-jie Yuan, Yue Song. Thanks for support of GE healthcare pharmaceutical diagnostics medical affairs for contributing to the data analysis.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to this work. We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Ethical approval
The study was approved and supervised by the institutional review boards of the seven participating institutions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to incorrect first author name. Now, it has been corrected from Qin-xin Zhao to Qin-xian Zhao.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, Qx., Wu, C., Tan, S. et al. Comparing Sonazoid contrast-enhanced ultrasound to contrast-enhanced CT and MRI for differentially diagnosing renal lesions: a prospective multicenter study. World J Urol 42, 302 (2024). https://doi.org/10.1007/s00345-024-04885-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04885-7