Abstract
Purpose
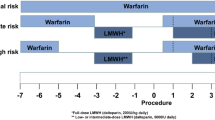
The perioperative management of patients who are receiving antithrombotic (antiplatelet or anticoagulant) therapy and require urologic surgery is challenging due to the inherent risk for surgical bleeding and the need to minimize thromboembolic risk. The aim of this review is to assess the quality and consistency of clinical practice guidelines (CPGs) and clinical practice recommendations (CPRs) on this topic, and to summarize the evidence and associated strength of recommendations relating to perioperative antithrombotic management.
Methods
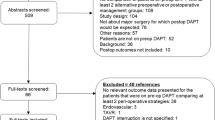
A pragmatic search of electronic databases and guidelines websites was performed to identify relevant CPGs/CPRs. The AGREE II (Appraisal of Guidelines for REsearch and Evaluation) instrument was used to assess the methodological quality and integrity of the CPGs.
Results
The CPGs provided by the European Association of Urology (EAU), the American College of Chest Physicians (ACCP) and the European Society of Cardiology/European Society of Anaesthesiology (ESC/ESA), and the CPRs provided by the International Consultation on Urological Disease (ICUD)/American Urologic Association (AUA) were retrieved and reviewed. The 3 CPGs were critically assessed using the AGREE II instrument. Inconsistent recommendations were provided based on the indication for antithrombotic medication, the antiplatelet/anticoagulant agent and the type of urological procedure. Based on the AGREE II tool for CPG assessment, the EAU CPGs scored higher (83.3 points) compared to the ESC/ESA (75 points) and ACCP CPG (66.7 points).
Conclusion
The perioperative management of antithrombotic therapy in urological patients is potentially challenging but inconsistent CPG of varying quality may create uncertainty as to best practices to minimize thromboembolic and bleeding risk.
Similar content being viewed by others
References
Holbrook A, Schulman S, Witt DM et al (2012) Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 141:e152S–e184S. https://doi.org/10.1378/chest.11-2295
Patrono C, Baigent C, Hirsh J, Roth G (2008) Antiplatelet drugs: American college of chest physicians evidence-based clinical practice guidelines (8th edition). Chest 133:199–233. https://doi.org/10.1378/chest.08-0672
DiNicolantonio JJ, D’Ascenzo F, Tomek A et al (2013) Clopidogrel is safer than ticagrelor in regard to bleeds: a closer look at the PLATO trial. Int J Cardiol 168:1739–1744. https://doi.org/10.1016/j.ijcard.2013.06.135
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361:1045–1057. https://doi.org/10.1056/NEJMoa0904327
Tafur A, Douketis J (2018) Perioperative management of anticoagulant and antiplatelet therapy. Heart Br Card Soc 104:1461–1467. https://doi.org/10.1136/heartjnl-2016-310581
Schwarz UR, Walter U, Eigenthaler M (2001) Taming platelets with cyclic nucleotides. Biochem Pharmacol 62:1153–1161. https://doi.org/10.1016/s0006-2952(01)00760-2
Diener HC, Cunha L, Forbes C et al (1996) European stroke prevention study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 143:1–13. https://doi.org/10.1016/s0022-510x(96)00308-5
Dornbos D, Nimjee SM (2018) Reversal of systemic anticoagulants and antiplatelet therapeutics. Neurosurg Clin N Am 29:537–545. https://doi.org/10.1016/j.nec.2018.06.005
Altenburg A, Haage P (2012) Antiplatelet and anticoagulant drugs in interventional radiology. Cardiovasc Intervent Radiol 35:30–42. https://doi.org/10.1007/s00270-011-0204-0
Sedat J, Chau Y, Mondot L et al (2014) Is eptifibatide a safe and effective rescue therapy in thromboembolic events complicating cerebral aneurysm coil embolization? Single-center experience in 42 cases and review of the literature. Neuroradiology 56:145–153. https://doi.org/10.1007/s00234-013-1301-3
Ageno W, Gallus AS, Wittkowsky A et al (2012) Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 141:e44S–e88S. https://doi.org/10.1378/chest.11-2292
Hackett CT, Ramanathan RS, Malhotra K et al (2015) Safety of venous thromboembolism prophylaxis with fondaparinux in ischemic stroke. Thromb Res 135:249–254. https://doi.org/10.1016/j.thromres.2014.11.041
Levy JH, Douketis J, Weitz JI (2018) Reversal agents for non-vitamin K antagonist oral anticoagulants. Nat Rev Cardiol 15:273–281. https://doi.org/10.1038/nrcardio.2017.223
Gómez-Outes A, Terleira-Fernández AI, Calvo-Rojas G et al (2013) Dabigatran, rivaroxaban, or apixaban versus warfarin in patients with nonvalvular atrial fibrillation: a systematic review and meta-analysis of subgroups. Thrombosis 2013:640723. https://doi.org/10.1155/2013/640723
O’Donnell MJ, Eikelboom JW, Yusuf S et al (2016) Effect of apixaban on brain infarction and microbleeds: AVERROES-MRI assessment study. Am Heart J 178:145–150. https://doi.org/10.1016/j.ahj.2016.03.019
Potpara TS, Polovina MM, Licina MM et al (2012) Novel oral anticoagulants for stroke prevention in atrial fibrillation: focus on apixaban. Adv Ther 29:491–507. https://doi.org/10.1007/s12325-012-0026-8
Granger CB, Alexander JH, McMurray JJV et al (2011) Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 365:981–992. https://doi.org/10.1056/NEJMoa1107039
Frost C, Wang J, Nepal S et al (2013) Apixaban, an oral, direct factor Xa inhibitor: single dose safety, pharmacokinetics, pharmacodynamics and food effect in healthy subjects. Br J Clin Pharmacol 75:476–487. https://doi.org/10.1111/j.1365-2125.2012.04369.x
Brouwers MC, Kho ME, Browman GP et al (2010) AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ Can Med Assoc J J Assoc Med Can 182:E839–842. https://doi.org/10.1503/cmaj.090449
Tikkinen KAO, Craigie S, Agarwal A et al (2018) Procedure-specific risks of thrombosis and bleeding in urological cancer surgery: systematic review and meta-analysis. Eur Urol 73:242–251. https://doi.org/10.1016/j.eururo.2017.03.008
Tikkinen KAO, Craigie S, Agarwal A et al (2018) Procedure-specific Risks of Thrombosis and Bleeding in Urological Non-cancer Surgery: systematic review and meta-analysis. Eur Urol 73:236–241. https://doi.org/10.1016/j.eururo.2017.02.025
Douketis JD, Spyropoulos AC, Spencer FA et al (2012) Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 141:e326S–e350S. https://doi.org/10.1378/chest.11-2298
Kristensen SD, Knuuti J, Saraste A et al (2014) 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management: the Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 35:2383–2431. https://doi.org/10.1093/eurheartj/ehu282
Culkin DJ, Exaire EJ, Green D et al (2014) Anticoagulation and antiplatelet therapy in urological practice: ICUD/AUA review paper. J Urol 192:1026–1034. https://doi.org/10.1016/j.juro.2014.04.103
Douketis JD, Spyropoulos AC, Duncan J et al (2019) Perioperative management of patients with atrial fibrillation receiving a direct oral anticoagulant. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2019.2431
Brosseau L, Rahman P, Toupin-April K et al (2014) (2014) A systematic critical appraisal for non-pharmacological management of osteoarthritis using the Appraisal of Guidelines Research and Evaluation II instrument. PLoS ONE 9(1):e82986
Author information
Authors and Affiliations
Contributions
KD: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. MIO: protocol/project development, data collection or management, data analysis, and manuscript writing/editing. AC: data collection or management and manuscript writing/editing. EA: data collection or management and manuscript writing/editing. JD: protocol/project development, data collection or management, and manuscript writing/editing. SG: protocol/project development, data collection or management, and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
No financial conflicts of interest. K. Dimitropoulos is a Senior Associate of the EAU Guidelines Office and a member of the EAU Guidelines Office Urethral Strictures panel, M.I. Omar is the EAU Guidelines Office Methodology Supervisor, S. Gravas is the Chair of the EAU Guidelines Office Male LUTS panel and J. Douketis is the first author of the ACCP Guidelines publication.
Human animals rights
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dimitropoulos, K., Omar, M.I., Chalkias, A. et al. Perioperative antithrombotic (antiplatelet and anticoagulant) therapy in urological practice: a critical assessment and summary of the clinical practice guidelines. World J Urol 38, 2761–2770 (2020). https://doi.org/10.1007/s00345-020-03078-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03078-2