Abstract
Objective
To compare contrast-enhanced ultrasound (CEUS) with microbubbles containing sulfur hexafluoride (SHF) and perfluorobutane (PFB) for the detection of colorectal liver metastasis (CRLM).
Methods
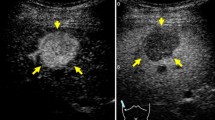
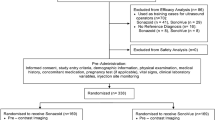
In this prospective study, conducted from September to November 2021, patients with colorectal cancer were consecutively recruited and underwent same-day ultrasound, SHF-CEUS, and PFB-CEUS. The reference standard was contrast-enhanced MRI and follow-up imaging. The size, depth, echogenicity, and calcification of each focal liver lesion were recorded. The number and conspicuity of CRLMs, based on washout appearance during the late phase (LP) (> 120 s)/Kupffer phase (KP), were evaluated offsite by two blinded readers.
Results
Overall, 230 lesions (CRLMs, n = 219; benign lesions, n = 11) in 78 patients were evaluated. Lesion conspicuity (p = 0.344) and accuracy in the detection of CRLM were comparable for SHF- and PFB-CEUS (0.877 for SHF vs. 0.770 for PFB, p = 0.087). More CRLMs ≥ 10 mm were identified by LP contrast washout in SHF-CEUS than in KP PFB-CEUS (p < 0.001). More CRLMs < 10 mm were identified by KP washout in PFB-CEUS than in LP SHF-CEUS (p < 0.001). Conspicuity was better on PFB-CEUS than on SHF-CEUS (p = 0.027). In hyperechoic lesions, lesions located deeper than 80 mm, and calcified lesions, CRLM conspicuity on PFB-CEUS was inferior to that on SHF-CEUS (p < 0.05).
Conclusions
The overall accuracy of detection and conspicuity of washout in CRLMs were comparable between SHF and PFB-CEUS. PFB-CEUS has the advantage of identifying washout in small CRLMs. However, larger, hyperechogenic, deep-seated, or calcified lesions were better identified using SHF-CEUS.
Clinical relevance statement
Accuracy of detection and conspicuity of washout in CRLMs were comparable between SHF- and PFB-CEUS. PFB-CEUS has the advantage in detecting small CRLMs, whereas SHF-CEUS is better for detecting larger, hyperechogenic, deep-seated, or calcified lesions.
Key Points
-
Contrast-enhanced ultrasound with sulfur hexafluoride in the late phase and perfluorobutane microbubbles in the Kupffer phase were comparable in terms of accuracy in the detection and conspicuity of colorectal liver metastases.
-
Small colorectal liver metastases (< 10 mm) were more often identified in the Kupffer phase contrast-enhanced ultrasound imaging when using perfluorobutane microbubbles.
-
Larger, hyperechogenic, deep-seated, or calcified lesions were better identified in the late phase contrast-enhanced ultrasound imaging (> 120 s) when using sulfur hexafluoride microbubbles.





Similar content being viewed by others
Abbreviations
- AP:
-
Arterial phase
- AUC:
-
The area under the ROC curve
- CEUS:
-
Contrast-enhanced ultrasound
- CRC:
-
Colorectal cancer
- CRLM:
-
Colorectal liver metastasis
- FLL:
-
Focal liver lesion
- KP:
-
Kupffer phase
- LP:
-
Late phase
- PFB:
-
Microbubbles containing perfluorobutane
- PVP:
-
Portal venous phase
- ROC:
-
Receiver operating characteristic
- SHF:
-
Microbubbles containing sulfur hexafluoride
- UCA:
-
Ultrasound contrast agent
- US:
-
Ultrasound
References
Chakedis J, Squires MH, Beal EW et al (2017) Update on current problems in colorectal liver metastasis. Curr Probl Surg 54:554–602. https://doi.org/10.1067/j.cpsurg.2017.10.002
Sawatzki M, Güller U, Güsewell S, Husarik DB, Semela D, Brand S (2021) Contrast-enhanced ultrasound can guide the therapeutic strategy by improving the detection of colorectal liver metastases. J Hepatol 74:419–427. https://doi.org/10.1016/j.jhep.2020.09.036
Lincke T, Zech CJ (2017) Liver metastases: detection and staging. Eur J Radiol 97:76–82. https://doi.org/10.1016/j.ejrad.2017.10.016
Vreugdenburg TD, Ma N, Duncan JK, Riitano D, Cameron AL, Maddern GJ (2016) Comparative diagnostic accuracy of hepatocyte-specific gadoxetic acid (Gd-EOB-DTPA) enhanced MR imaging and contrast enhanced CT for the detection of liver metastases: a systematic review and meta-analysis. Int J Colorectal Dis 31:1739–1749. https://doi.org/10.1007/s00384-016-2664-9
Baghdadi A, Mirpour S, Ghadimi M et al (2022) Imaging of colorectal liver metastasis. J Gastrointest Surg 26:245–257. https://doi.org/10.1007/s11605-021-05164-1
Qin S, Chen Y, Liu XY et al (2017) Clinical application of contrast-enhanced ultrasound using high-frequency linear probe in the detection of small colorectal liver metastases. Ultrasound Med Biol 43:2765–2773. https://doi.org/10.1016/j.ultrasmedbio.2017.08.932
Tsili AC, Alexiou G, Naka C, Argyropoulou MI (2021) Imaging of colorectal cancer liver metastases using contrast-enhanced US, multidetector CT, MRI, and FDG PET/CT: a meta-analysis. Acta Radiol 62:302–312. https://doi.org/10.1177/0284185120925481
Dietrich CF, Nolsøe CP, Barr RG et al (2020) Guidelines and good clinical practice recommendations for contrast-enhanced ultrasound (CEUS) in the liver-update 2020 WFUMB in cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound Med Biol 46:2579–2604. https://doi.org/10.1016/j.ultrasmedbio.2020.04.030
Lv K, Zhai H, Jiang Y et al (2021) Prospective assessment of diagnostic efficacy and safety of SonazoidTM and SonoVue® ultrasound contrast agents in patients with focal liver lesions. Abdom Radiol (NY) 46:4647–4659. https://doi.org/10.1007/s00261-021-03010-1
Barr RG, Huang P, Luo Y et al (2020) Contrast-enhanced ultrasound imaging of the liver: a review of the clinical evidence for SonoVue and Sonazoid. Abdom Radiol (NY) 45:3779–3788. https://doi.org/10.1007/s00261-020-02573-9
Zhai HY, Liang P, Yu J et al (2019) Comparison of SonoVue and Sonazoid in the diagnosis of focal liver lesions: a preliminary study. J Ultrasound Med 38:2417–2425. https://doi.org/10.1002/jum.14940
Kang HJ, Lee JM, Yoon JH, Lee K, Kim H, Han JK (2020) Contrast-enhanced US with sulfur hexafluoride and perfluorobutane for the diagnosis of hepatocellular carcinoma in individuals with high risk. Radiology 297:108–116. https://doi.org/10.1148/radiol.2020200115
Piscaglia F, Corradi F, Mancini M et al (2007) Real time contrast enhanced ultrasonography in detection of liver metastases from gastrointestinal cancer. BMC Cancer 7:171. https://doi.org/10.1186/1471-2407-7-171
Kobayashi N, Iijima H, Tada T et al (2021) A new ultrasonographic “fluttering sign” for hepatic hemangioma. Ultrasound Med Biol 47:941–946. https://doi.org/10.1016/j.ultrasmedbio.2020.12.004
Kang TW, Jeong WK, Kim YY et al (2021) Comparison of super-resolution US and contrast material-enhanced US in detection of the spoke wheel sign in patients with focal nodular hyperplasia. Radiology 298:82–90. https://doi.org/10.1148/radiol.2020200885
Lee MW, Kim YJ, Park SW et al (2010) Sequential changes in echogenicity and conspicuity of small hepatocellular carcinoma on gray scale sonography after transcatheter arterial chemoembolization. J Ultrasound Med 29:1305–1312. https://doi.org/10.7863/jum.2010.29.9.1305
Lee JY, Minami Y, Choi BI et al (2020) The AFSUMB consensus statements and recommendations for the clinical practice of contrast-enhanced ultrasound using Sonazoid. J Med Ultrasound 28:59–82. https://doi.org/10.4103/JMU.JMU_124_19
Cantisani V, Ricci P, Erturk M et al (2010) Detection of hepatic metastases from colorectal cancer: prospective evaluation of gray scale US versus SonoVue® low mechanical index real time-enhanced US as compared with multidetector-CT or Gd-BOPTA-MRI. Ultraschall Med 31:500–505. https://doi.org/10.1055/s-0028-1109751
Shiozawa K, Watanabe M, Ikehara T et al (2017) Comparison of contrast-enhanced ultrasonograpy with Gd-EOB-DTPA-enhanced MRI in the diagnosis of liver metastasis from colorectal cancer. J Clin Ultrasound 45:138–144. https://doi.org/10.1002/jcu.22421
Sun L, Yin S, Xing B, Li Z, Fan Z, Yan K (2023) Contrast-enhanced ultrasound with SonoVue and Sonazoid for the diagnosis of colorectal liver metastasis after chemotherapy. J Ultrasound Med 42:355–362. https://doi.org/10.1002/jum.16042
Mainenti PP, Mancini M, Mainolfi C et al (2010) Detection of colo-rectal liver metastases: prospective comparison of contrast enhanced US, multidetector CT, PET/CT, and 1.5 Tesla MR with extracellular and reticulo-endothelial cell specific contrast agents. Abdom Imaging 35:511–521. https://doi.org/10.1007/s00261-009-9555-2
Zhang L, Zhang L, Wang H, Chen L, Sui G (2019) Diagnostic performance of contrast-enhanced ultrasound and magnetic resonance imaging for detecting colorectal liver metastases: a systematic review and meta-analysis. Dig Liver Dis 51:1241–1248. https://doi.org/10.1016/j.dld.2019.06.004
Goto E, Masuzaki R, Tateishi R et al (2012) Value of post-vascular phase (Kupffer imaging) by contrast-enhanced ultrasonography using Sonazoid in the detection of hepatocellular carcinoma. J Gastroenterol 47:477–485. https://doi.org/10.1007/s00535-011-0512-9
Sugimoto K, Moriyasu F, Saito K, Yoshiara H, Imai Y (2014) Kupffer-phase findings of hepatic hemangiomas in contrast-enhanced ultrasound with Sonazoid. Ultrasound Med Biol 40:1089–1095. https://doi.org/10.1016/j.ultrasmedbio.2013.12.019
Tochio H, Sugahara M, Imai Y et al (2015) Hyperenhanced rim surrounding liver metastatic tumors in the postvascular phase of Sonazoid-enhanced ultrasonography: a histological indication of the presence of Kupffer cells. Oncology 89:33–41. https://doi.org/10.1159/000440629
Ciner AT, Jones K, Muschel RJ, Brodt P (2020) The unique immune microenvironment of liver metastases: challenges and opportunities. Semin Cancer Biol 71:143–156. https://doi.org/10.1016/j.semcancer.2020.06.003
Qiao T, Yang W, He X et al (2023) Dynamic differentiation of F4/80+ tumor-associated macrophage and its role in tumor vascularization in a syngeneic mouse model of colorectal liver metastasis. Cell Death Dis 14:117. https://doi.org/10.1038/s41419-023-05626-1
Zhou Y, Zhang J, Dan P et al (2019) Tumor calcification as a prognostic factor in cetuximab plus chemotherapy-treated patients with metastatic colorectal cancer. Anticancer Drugs 30:195–200. https://doi.org/10.1097/CAD.0000000000000726
Dietrich CF, Averkiou M, Nielsen MB et al (2018) How to perform contrast-enhanced ultrasound (CEUS). Ultrasound Int Open 4:E2–E15. https://doi.org/10.1055/s-0043-123931
Fetzer DT, Vijay K, Caserta MP, Patterson-Lachowicz A, Dahiya N, Rodgers SK (2023) Artifacts and technical considerations at contrast-enhanced US. Radiographics 43:e220093. https://doi.org/10.1148/rg.220093
Acknowledgements
Supported by National Key Clinical Discipline. Supported by the program of Guangdong Provincial Clinical Research Center for Digestive Diseases (2020B1111170004).
Funding
This study has received funding by the program of Guangdong Provincial Clinical Research Center for Digestive Diseases (2020B1111170004).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is GuangJian Liu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
The study subjects or cohorts have not been reported yet.
Methodology
-
prospective
-
observational
-
performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 186 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qin, S., Chen, Y., Wang, Y. et al. Contrast-enhanced ultrasound with microbubbles containing sulfur hexafluoride and perfluorobutane with Kupffer phase for the detection of colorectal liver metastases. Eur Radiol 34, 622–631 (2024). https://doi.org/10.1007/s00330-023-10051-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10051-1