Abstract
Objectives
To compare interobserver agreement and image quality of 3D T2-weighted fast spin echo (T2w-FSE) L-spine MRI images processed with a deep learning reconstruction (DLRecon) against standard-of-care (SOC) reconstruction, as well as against 2D T2w-FSE images. The hypothesis was that DLRecon 3D T2w-FSE would afford improved image quality and similar interobserver agreement compared to both SOC 3D and 2D T2w-FSE.
Methods
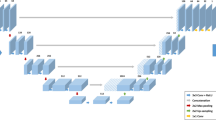
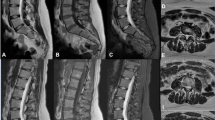
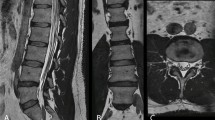
Under IRB approval, patients who underwent routine 3-T lumbar spine (L-spine) MRI from August 17 to September 17, 2020, with both isotropic 3D and 2D T2w-FSE sequences, were retrospectively included. A DLRecon algorithm, with denoising and sharpening properties was applied to SOC 3D k-space to generate 3D DLRecon images. Four musculoskeletal radiologists blinded to reconstruction status evaluated randomized images for motion artifact, image quality, central/foraminal stenosis, disc degeneration, annular fissure, disc herniation, and presence of facet joint cysts. Inter-rater agreement for each graded variable was evaluated using Conger’s kappa (κ).
Results
Thirty-five patients (mean age 58 ± 19, 26 female) were evaluated. 3D DLRecon demonstrated statistically significant higher median image quality score (2.0/2) when compared to SOC 3D (1.0/2, p < 0.001), 2D axial (1.0/2, p < 0.001), and 2D sagittal sequences (1.0/2, p value < 0.001). κ ranges (and 95% CI) for foraminal stenosis were 0.55–0.76 (0.32–0.86) for 3D DLRecon, 0.56–0.73 (0.35–0.84) for SOC 3D, and 0.58–0.71 (0.33–0.84) for 2D. Mean κ (and 95% CI) for central stenosis at L4-5 were 0.98 (0.96–0.99), 0.97 (0.95–0.99), and 0.98 (0.96–0.99) for 3D DLRecon, 3D SOC and 2D, respectively.
Conclusions
DLRecon 3D T2w-FSE L-spine MRI demonstrated higher image quality and similar interobserver agreement for graded variables of interest when compared to 3D SOC and 2D imaging.
Key Points
• 3D DLRecon T2w-FSE isotropic lumbar spine MRI provides improved image quality when compared to 2D MRI, with similar interobserver agreement for clinical evaluation of pathology.
• 3D DLRecon images demonstrated better image quality score (2.0/2) when compared to standard-of-care (SOC) 3D (1.0/2), p value < 0.001; 2D axial (1.0/2), p value < 0.001; and 2D sagittal sequences (1.0/2), p value < 0.001.
• Interobserver agreement for major variables of interest was similar among all sequences and reconstruction types. For foraminal stenosis, κ ranged from 0.55 to 0.76 (95% CI 0.32–0.86) for 3D DLRecon, 0.56–0.73 (95% CI 0.35–0.84) for standard-of-care (SOC) 3D, and 0.58–0.71 (95% CI 0.33–0.84) for 2D.





Similar content being viewed by others
Abbreviations
- DL:
-
Deep learning
- DLRecon:
-
Deep learning reconstruction
- L-spine:
-
Lumbar spine
- MPR:
-
Multiplanar reformat
- SOC:
-
Standard of care
- T2w-FSE:
-
T2-weighted fast spin echo
- 3D:
-
Three-dimensional
- 2D:
-
Two-dimensional
References
McBee MP, Awan OA, Colucci AT et al (2018) Deep learning in radiology. Acad Radiol 25:1472–1480
Mazurowski MA, Buda M, Saha A, Bashir MR (2019) Deep learning in radiology: an overview of the concepts and a survey of the state of the art with focus on MRI. J Magn Reson Imaging 49:939–954
Rajpurkar P, Irvin J, Zhu K et al (2017) CheXNet: radiologist-level pneumonia detection on chest X-rays with deep learning. arXiv:1711.05225
Castro-Mateos I, Hua R, Pozo JM, Lazary A, Frangi AF (2016) Intervertebral disc classification by its degree of degeneration from T2-weighted magnetic resonance images. Eur Spine J 25:2721–2727
Hallinan JTPD, Zhu L, Yang K et al (2021) Deep learning model for automated detection and classification of central canal, lateral recess, and neural foraminal stenosis at lumbar spine MRI. Radiology 300:130–138
LewandrowskI K-U, Muraleedharan N, Eddy SA et al (2020) Feasibility of deep learning algorithms for reporting in routine spine magnetic resonance imaging. Int J Spine Surg 14:S86–S97
Higaki T, Nakamura Y, Tatsugami F, Nakaura T, Awai K (2019) Improvement of image quality at CT and MRI using deep learning. Jpn J Radiol 37:73–80
Chaudhari AS, Fang Z, Kogan F et al (2018) Super-resolution musculoskeletal MRI using deep learning. Magn Reson Med 80:2139–2154
Tatsugami F, Higaki T, Nakamura Y et al (2019) Deep learning–based image restoration algorithm for coronary CT angiography. Eur Radiol 29:5322–5329
Kidoh M, Shinoda K, Kitajima M et al (2020) Deep learning based noise reduction for brain MR imaging: tests on phantoms and healthy volunteers. Magn Reson Med Sci 19:195–206
Hammernik K, Klatzer T, Kobler E et al (2018) Learning a variational network for reconstruction of accelerated MRI data. Magn Reson Med 79:3055–3071
Lee S, Jee WH, Jung JY, Lee SY, Ryu KS, Ha KY (2015) MRI of the lumbar spine: comparison of 3D isotropic turbo spin-echo SPACE sequence versus conventional 2D sequences at 3.0 T. Acta Radiol 56:174–181
Blizzard DJ, Haims AH, Lischuk AW, Arunakul R, Hustedt JW, Grauer JN (2015) 3D-FSE isotropic MRI of the lumbar spine: novel application of an existing technology. J Spinal Disord Tech 28:152–157
Sayah A, Jay AK, Toaff JS, Makariou EV, Berkowitz F (2016) Effectiveness of a rapid lumbar spine MRI protocol using 3D T2-weighted SPACE imaging versus a standard protocol for evaluation of degenerative changes of the lumbar spine. AJR Am J Roentgenol 207:614–620
Rodegerdts EA, Boss A, Riemarzik K et al (2006) 3D imaging of the whole spine at 3T compared to 1.5T: initial experiences. Acta Radiol 47:488–493
Ristow O, Steinbach L, Sabo G et al (2009) Isotropic 3D fast spin-echo imaging versus standard 2D imaging at 3.0 T of the knee--image quality and diagnostic performance. Eur Radiol 19:1263–1272
Carrino JA, Lurie JD, Tosteson AN et al (2009) Lumbar spine: reliability of MR imaging findings. Radiology 250:161–170
Schizas C, Theumann N, Burn A et al (2010) Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976) 35:1919–1924
Lurie JD, Tosteson AN, Tosteson TD et al (2008) Reliability of readings of magnetic resonance imaging features of lumbar spinal stenosis. Spine (Phila Pa 1976) 33:1605–1610
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878
Weishaupt D, Zanetti M, Boos N, Hodler J (1999) MR imaging and CT in osteoarthritis of the lumbar facet joints. Skelet Radiol 28:215–219
Lebel RM (2020) Performance characterization of a novel deep learning-based MR image reconstruction pipeline.
Kim M, Kim HS, Kim HJ et al (2021) Thin-slice pituitary MRI with deep learning-based reconstruction: diagnostic performance in a postoperative setting. Radiology 298:114–122
Zochowski KC, Tan ET, Argentieri EC et al (2021) Improvement of peripheral nerve visualization using a deep learning-based MR reconstruction algorithm. Magn Reson Imaging 85:186–192
van der Velde N, Hassing HC, Bakker BJ et al (2021) Improvement of late gadolinium enhancement image quality using a deep learning-based reconstruction algorithm and its influence on myocardial scar quantification. Eur Radiol 31:3846–3855
Oh CH, Yoon SH (2017) Whole spine disc degeneration survey according to the ages and sex using Pfirrmann disc degeneration grades. Korean J Spine 14:148–154
Ishimoto Y, Yoshimura N, Muraki S et al (2013) Associations between radiographic lumbar spinal stenosis and clinical symptoms in the general population: the Wakayama Spine Study. Osteoarthritis Cartilage 21:783–788
Stadnik TW, Lee RR, Coen HL, Neirynck EC, Buisseret TS, Osteaux MJ (1998) Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology 206:49–55
Weishaupt D, Zanetti M, Hodler J, Boos N (1998) MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology 209:661–666
Schönström N, Hansson T (1988) Pressure changes following constriction of the cauda equina. An experimental study in situ. Spine (Phila Pa 1976) 13:385–388
Argentieri EC, Koff MF, Breighner RE, Endo Y, Shah PH, Sneag DB (2018) Diagnostic accuracy of zero-echo time MRI for the evaluation of cervical neural foraminal stenosis. Spine (Phila Pa 1976) 43:928–933
Ashby D (1991) Practical statistics for medical research. Douglas G. Altman, Chapman and Hall, London, 1991. No. of pages: 611. Stat Med 10:1635–1636
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Koontz NA, Wiggins RH 3rd, Mills MK et al (2017) Less is more: efficacy of rapid 3D-T2 SPACE in ED patients with acute atypical low back pain. Acad Radiol 24:988–994
Lee S, Lee JW, Yeom JS et al (2010) A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol 194:1095–1098
Acknowledgements
We would like to acknowledge Yan Wen (GE Healthcare) and Maggie Fung (GE Healthcare) for their important contributions to the 3D deep learning reconstruction implementation. We would also like to acknowledge Jake Fiore for his assistance with data collection.
Funding
The Hospital for Special Surgery receives institutional research support from GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Darryl B. Sneag.
Conflict of interest
Hospital for Special Surgery receives institutional research support from GE Healthcare. All authors acknowledge that they have no personal investment in the software evaluated in this study.
Statistics and biometry
Joseph Nguyen kindly provided statistical advice for this manuscript. One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, S., Tan, E.T., Mintz, D.N. et al. Evaluation of deep learning reconstructed high-resolution 3D lumbar spine MRI. Eur Radiol 32, 6167–6177 (2022). https://doi.org/10.1007/s00330-022-08708-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08708-4