Abstract
Objectives
To investigate the role of clinicopathological factors and MR imaging factors in risk stratification of combined hepatocellular cholangiocarcinoma (cHCC-CCA) patients who were classified as LR-M and LR-4/5.
Methods
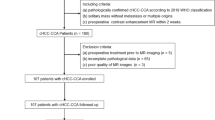
We retrospectively identified consecutive patients who were confirmed as cHCC-CCA after surgical surgery in our institution from June 2015 to November 2020. Two radiologists evaluated the preoperative MR imaging features independently, and each lesion was assigned with a LI-RADS category. Preoperative clinical data were also collected. Multivariate Cox proportional hazards model was applied to separately identify the independent factors correlated with the recurrence of cHCC-CCAs in LR-M and LR-4/5. Risk stratifications were conducted separately in LR-M and LR-4/5. Recurrence-free survival (RFS) rates and overall survival (OS) rates were analyzed by using the Kaplan-Meier survival curves and log-rank test.
Results
A total of 131 patients with single primary lesion which met the 2019 WHO classification criteria were finally included. Corona enhancement, delayed central enhancement, and microvascular invasion (MVI) were identified as predictors of RFS in LR-M. Mosaic architecture, CA19-9, and MVI were independently associated with RFS in LR-4/5. Based on the number of these independent predictors, patients were stratified into favorable-outcome groups (LR-ML subgroup and LR-4/5L subgroup) and dismal-outcome groups (LR-MH subgroup and LR-4/5H subgroup). The corresponding median RFS for LR-ML, LR-MH, LR-5L, and LR-5H were 25.6 months, 8.2 months, 51.7 months, and 18.1 months.
Conclusion
Our study explored the prognostic values of imaging and clinicopathological factors for LR-M and LR-4/5 cHCC-CCA patients, and different survival outcomes were observed among four subgroups after conducting risk stratifications.
Key Points
• Corona enhancement, delayed central enhancement, and MVI were identified as predictors of RFS in cHCC-CCAs which were classified into LR-M. Mosaic architecture, CA19-9, and MVI were independently associated with RFS in cHCC-CCAs which were classified into LR-4/5.
• Based on the identified risk factors, LR-M and LR-4/5 cHCC-CCA patients could be stratified into two subgroups respectively, with significantly different RFS and OS.
• cHCC-CCA patients from LR-M did not always have worse RFS and OS than those from LR-4/5 in some cases.





Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- CA19-9:
-
Carbohydrate 19-9
- cHCC-CCA:
-
Combined hepatocellular cholangiocarcinoma
- LI-RADS/LR:
-
Liver Imaging Reporting and Data System
- MR:
-
Magnetic resonance
- MVI:
-
Microvascular invasion
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
References
Brunt E, Aishima S, Clavien PA et al (2018) cHCC-CCA: consensus terminology for primary liver carcinomas with both hepatocytic and cholangiocytic differentation. Hepatology 68:113–126
Schizas D, Mastoraki A, Routsi E et al (2020) Combined hepatocellular-cholangiocarcinoma: an update on epidemiology, classification, diagnosis and management. Hepatobiliary Pancreat Dis Int 19:515–523
Xue R, Chen L, Zhang C et al (2019) Genomic and transcriptomic profiling of combined hepatocellular and intrahepatic cholangiocarcinoma reveals distinct molecular subtypes. Cancer Cell 35:932–947.e938
Joseph NM, Tsokos CG, Umetsu SE et al (2019) Genomic profiling of combined hepatocellular-cholangiocarcinoma reveals similar genetics to hepatocellular carcinoma. J Pathol 248:164–178
Lee HS, Kim MJ, An C (2019) How to utilize LR-M features of the LI-RADS to improve the diagnosis of combined hepatocellular-cholangiocarcinoma on gadoxetate-enhanced MRI? Eur Radiol 29:2408–2416
Granata V, Fusco R, Venanzio Setola S et al (2020) Major and ancillary features according to LI-RADS in the assessment of combined hepatocellular-cholangiocarcinoma. Radiol Oncol 54:149–158
Jeon SK, Joo I, Lee DH et al (2019) Combined hepatocellular cholangiocarcinoma: LI-RADS v2017 categorisation for differential diagnosis and prognostication on gadoxetic acid-enhanced MR imaging. Eur Radiol 29:373–382
Choi SH, Jeon SK, Lee SS et al (2021) Radio-pathologic correlation of biphenotypic primary liver cancer (combined hepatocellular cholangiocarcinoma): changes in the 2019 WHO classification and impact on LI-RADS classification at liver MRI. Eur Radiol. https://doi.org/10.1007/s00330-021-07984-w
Choi SH, Lee SS, Park SH et al (2019) LI-RADS classification and prognosis of primary liver cancers at gadoxetic acid-enhanced MRI. Radiology 290:388–397
Beaufrère A, Calderaro J, Paradis V (2021) Combined hepatocellular-cholangiocarcinoma: an update. J Hepatol 74:1212–1224
Wakizaka K, Yokoo H, Kamiyama T et al (2019) Clinical and pathological features of combined hepatocellular-cholangiocarcinoma compared with other liver cancers. J Gastroenterol Hepatol 34:1074–1080
Chu KJ, Lu CD, Dong H, Fu XH, Zhang HW, Yao XP (2014) Hepatitis B virus-related combined hepatocellular-cholangiocarcinoma: clinicopathological and prognostic analysis of 390 cases. Eur J Gastroenterol Hepatol 26:192–199
Zhou C, Wang Y, Ma L, Qian X, Yang C, Zeng M (2021) Combined hepatocellular carcinoma-cholangiocarcinoma: MRI features correlated with tumor biomarkers and prognosis. Eur Radiol. https://doi.org/10.1007/s00330-021-08188-y
Park SH, Lee SS, Yu E et al (2017) Combined hepatocellular-cholangiocarcinoma: gadoxetic acid-enhanced MRI findings correlated with pathologic features and prognosis. J Magn Reson Imaging 46:267–280
Chernyak V, Fowler KJ, Kamaya A et al (2018) Liver imaging reporting and data system (LI-RADS) version 2018: imaging of hepatocellular carcinoma in at-risk patients. Radiology 289:816–830
Wang X, Wang W, Ma X et al (2020) Combined hepatocellular-cholangiocarcinoma: which preoperative clinical data and conventional MRI characteristics have value for the prediction of microvascular invasion and clinical significance? Eur Radiol 30:5337–5347
Lim K, Kwon H, Cho J (2020) Inter-reader agreement and imaging-pathology correlation of the LI-RADS M on gadoxetic acid-enhanced magnetic resonance imaging: efforts to improve diagnostic performance. Abdom Radiol (NY) 45:2430–2439
Nagtegaal ID, Odze RD, Klimstra D et al (2020) The 2019 WHO classification of tumours of the digestive system. Histopathology 76:182–188
Durnez A, Verslype C, Nevens F et al (2006) The clinicopathological and prognostic relevance of cytokeratin 7 and 19 expression in hepatocellular carcinoma. A possible progenitor cell origin. Histopathology 49:138–151
Wu H, Han X, Wang Z et al (2020) Prediction of the Ki-67 marker index in hepatocellular carcinoma based on CT radiomics features. Phys Med Biol 65:235048
Jiang H, Song B, Qin Y et al (2021) Diagnosis of LI-RADS M lesions on gadoxetate-enhanced MRI: identifying cholangiocarcinoma-containing tumor with serum markers and imaging features. Eur Radiol 31:3638–3648
Kitao A, Zen Y, Matsui O, Gabata T, Nakanuma Y (2009) Hepatocarcinogenesis: multistep changes of drainage vessels at CT during arterial portography and hepatic arteriography--radiologic-pathologic correlation. Radiology 252:605–614
Ham JH, Yu JS, Choi JM, Cho ES, Kim JH, Chung JJ (2021) Corona enhancement can substitute enhancing capsule in the imaging diagnosis of small (≤ 3 cm) HCCs on gadoxetic acid-enhanced MRI. Eur Radiol. https://doi.org/10.1007/s00330-021-07911-z
Wei H, Jiang H, Liu X et al (2020) Can LI-RADS imaging features at gadoxetic acid-enhanced MRI predict aggressive features on pathology of single hepatocellular carcinoma? Eur J Radiol 132:109312
Wei H, Jiang H, Zheng T et al (2021) LI-RADS category 5 hepatocellular carcinoma: preoperative gadoxetic acid-enhanced MRI for early recurrence risk stratification after curative resection. Eur Radiol 31:2289–2302
Chen J, Zhou J, Kuang S et al (2019) Liver Imaging Reporting and Data System Category 5: MRI predictors of microvascular invasion and recurrence after hepatectomy for hepatocellular carcinoma. AJR Am J Roentgenol 213:821–830
Li M, Xin Y, Fu S et al (2016) Corona enhancement and mosaic architecture for prognosis and selection between of liver resection versus transcatheter arterial chemoembolization in single hepatocellular carcinomas >5 cm without extrahepatic metastases: an imaging-based retrospective study. Medicine (Baltimore) 95:e2458
Asayama Y, Yoshimitsu K, Irie H et al (2006) Delayed-phase dynamic CT enhancement as a prognostic factor for mass-forming intrahepatic cholangiocarcinoma. Radiology 238:150–155
Funding
This study has received funding by National Natural Science Foundation of China (grant number 91859107), National Natural Science Foundation of China (grant number 82171897), Shanghai Science and Technology Committee (grant number 19411965500), Clinical Research Project of Zhongshan Hospital, Fudan University (grant number 2018ZSLC22), Shanghai Municipal Key Clinical Specialty (grant number shslczdzk03202), Clinical Research Plan of SHDC (grant number SHDC2020CR1029B), and Clinical Research Project of Zhongshan Hospital, Fudan University (grant number 2020ZSLC61).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Mengsu Zeng.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethics approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Wang X, Wang W, Ma X et al (2020) Combined hepatocellular-cholangiocarcinoma: which preoperative clinical data and conventional MRI characteristics have value for the prediction of microvascular invasion and clinical significance? European radiology 30:5337-5347
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Y., Zhu, GQ., Zhou, CW. et al. Risk stratification of LI-RADS M and LI-RADS 4/5 combined hepatocellular cholangiocarcinoma: prognostic values of MR imaging features and clinicopathological factors. Eur Radiol 32, 5166–5178 (2022). https://doi.org/10.1007/s00330-022-08691-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08691-w