Abstract
Objectives
To evaluate the diagnostic performance of zero echo time (ZTE) MRI in the depiction of structural lesions of sacroiliac joints (SIJs) in patients with the suspicion of sacroiliitis compared with T1-weighted fast spin echo (T1 FSE), using CT as the reference standard.
Methods
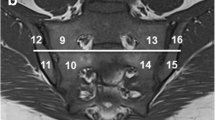
Forty patients with suspicion of sacroiliitis underwent both CT and MR scans of SIJs with 80 SIJs (160 bone articular surfaces) included for analysis. Two readers independently scored SIJs for structural lesions on CT and MR images. The diagnostic capability of ZTE MRI and T1 FSE were compared by the McNemar test, using CT as the reference standard. Agreements of diagnosis and sum scores of lesions between MR sequences and CT as well as between readers were also investigated using Cohen’s κappa tests and intraclass correlation coefficients.
Results
Diagnostic accuracy of ZTE MRI was higher than that of T1 FSE for erosions, sclerosis, and joint space changes (e.g., joint space changes: 91.3% vs 75.0%). ZTE MRI also improved sensitivity for detection of erosions and sclerosis (e.g., erosions at the joint level: 98.2% vs 80.0%) as well as specificity for detection of joint space changes (93.0% vs 67.4%). ZTE MRI had more consistency with CT than T1 FSE for both diagnosis and sum scores. Inter-reader agreements were higher for CT and ZTE MRI than those for T1 FSE.
Conclusions
ZTE MRI showed superior diagnostic performance in the depiction of SIJ structural lesions compared with routine T1-weighted MRI and had reliability comparable to CT.
Key Points
• ZTE MRI can provide CT-like bone contrast for the depiction of osseous structural lesions of the sacroiliac joints.
• ZTE MRI showed superior diagnostic performance than conventional T1 FSE in the detection of osseous structural lesions of sacroiliitis, using CT as the reference standard.
• In terms of inter-reader reliability, ZTE MRI performed comparably to CT and better than conventional T1 FSE.






Similar content being viewed by others
Abbreviations
- 3D:
-
Three-dimensional
- ASAS:
-
Assessment of SpondyloArthritis international Society
- AxSpA:
-
Axial spondyloarthritis
- DICOM:
-
Digital Imaging and Communications in Medicine
- FSE:
-
Fast spin echo
- GRE:
-
Gradient echo
- ICC:
-
Intraclass correlation coefficient
- IRB:
-
Institutional review board
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- sCT:
-
Synthetic CT
- SIJ:
-
Sacroiliac joint
- TE:
-
Echo time
- TR:
-
Repetition time
- UTE:
-
Ultrashort echo time
- VIBE:
-
Volumetric interpolated breath-hold examination
- WS-bSSFP:
-
Water selective balanced steady-state free precession
- ZTE:
-
Zero echo time
References
Sieper J, Poddubnyy D (2017) Axial spondyloarthritis. Lancet 390:73–84
Sieper J, Rudwaleit M, Baraliakos X et al (2009) The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 68(Suppl 2):ii1-44
van Gaalen FA, Bakker PA, de Hooge M, Schoones JW, van der Heijde D (2014) Assessment of sacroiliitis by radiographs and MRI: where are we now? Curr Opin Rheumatol 26:384–388
Oostveen J, Prevo R, den Boer J, van de Laar M (1999) Early detection of sacroiliitis on magnetic resonance imaging and subsequent development of sacroiliitis on plain radiography. A prospective, longitudinal study. J Rheumatol 26:1953–1958
Maksymowych WP, Wichuk S, Dougados M et al (2017) MRI evidence of structural changes in the sacroiliac joints of patients with non-radiographic axial spondyloarthritis even in the absence of MRI inflammation. Arthritis Res Ther 19:126
Maksymowych WP, Lambert RG, Østergaard M et al (2019) MRI lesions in the sacroiliac joints of patients with spondyloarthritis: an update of definitions and validation by the ASAS MRI working group. Ann Rheum Dis 78:1550–1558
Weber U, Lambert RG, Pedersen SJ, Hodler J, Østergaard M, Maksymowych WP (2010) Assessment of structural lesions in sacroiliac joints enhances diagnostic utility of magnetic resonance imaging in early spondylarthritis. Arthritis Care Res (Hoboken) 62:1763–1771
Weber U, Lambert RG, Østergaard M, Hodler J, Pedersen SJ, Maksymowych WP (2010) The diagnostic utility of magnetic resonance imaging in spondylarthritis: an international multicenter evaluation of one hundred eighty-seven subjects. Arthritis Rheum 62:3048–3058
Berthelot JM, le Goff B, Maugars Y, Laredo JD (2016) Sacroiliac joint edema by MRI: far more often mechanical than inflammatory? Joint Bone Spine 83:3–5
Arnbak B, GretheJurik A, Hørslev-Petersen K et al (2016) Associations between spondyloarthritis features and magnetic resonance imaging findings: a cross-sectional analysis of 1,020 patients With Persistent Low Back Pain. Arthritis Rheumatol 68:892–900
Dubreuil M, Deodhar AA (2017) Axial spondyloarthritis classification criteria: the debate continues. Curr Opin Rheumatol 29:317–322
Heuft-Dorenbosch L, Landewé R, Weijers R et al (2006) Combining information obtained from magnetic resonance imaging and conventional radiographs to detect sacroiliitis in patients with recent onset inflammatory back pain. Ann Rheum Dis 65:804–808
Weber U, Pedersen SJ, Østergaard M, Rufibach K, Lambert RG, Maksymowych WP (2012) Can erosions on MRI of the sacroiliac joints be reliably detected in patients with ankylosing spondylitis? - a cross-sectional study. Arthritis Res Ther 14:R124
Devauchelle-Pensec V, D’Agostino MA, Marion J et al (2012) Computed tomography scanning facilitates the diagnosis of sacroiliitis in patients with suspected spondylarthritis: results of a prospective multicenter French cohort study. Arthritis Rheum 64:1412–1419
Leone A, Cassar-Pullicino VN, D’Aprile P, Nasuto M, Guglielmi G (2017) Computed Tomography and MR Imaging in Spondyloarthritis. Radiol Clin North Am 55:1009–1021
Dougados M, Sepriano A, Molto A et al (2017) Sacroiliac radiographic progression in recent onset axial spondyloarthritis: the 5-year data of the DESIR cohort. Ann Rheum Dis 76:1823–1828
Maksymowych WP (2019) The role of imaging in the diagnosis and management of axial spondyloarthritis. Nat Rev Rheumatol 15:657–672
Wiesinger F, Sacolick LI, Menini A et al (2016) Zero TE MR bone imaging in the head. Magn Reson Med 75:107–114
Breighner RE, Endo Y, Konin GP, Gulotta LV, Koff MF, Potter HG (2018) Technical developments: zero echo time imaging of the shoulder: enhanced osseous detail by using MR imaging. Radiology 286:960–966
Weiger M, Pruessmann KP, Hennel F (2011) MRI with zero echo time: hard versus sweep pulse excitation. Magn Reson Med 66:379–389
Du J, Bydder GM (2013) Qualitative and quantitative ultrashort-TE MRI of cortical bone. NMR Biomed 26:489–506
Chang EY, Du J, Statum S, Pauli C, Chung CB (2015) Quantitative bi-component T2* analysis of histologically normal Achilles tendons. Muscles Ligaments Tendons J 5:58–62
Weiger M, Pruessmann KP (2019) Short-T(2) MRI: principles and recent advances. Prog Nucl Magn Reson Spectrosc 114–115:237–270
Argentieri EC, Koff MF, Breighner RE, Endo Y, Shah PH, Sneag DB (2018) Diagnostic accuracy of zero-echo time MRI for the evaluation of cervical neural foraminal stenosis. Spine (Phila Pa 1976) 43:928–933
Breighner RE, Bogner EA, Lee SC, Koff MF, Potter HG (2019) Evaluation of osseous morphology of the hip using zero echo time magnetic resonance imaging. Am J Sports Med 47:3460–3468
Rudwaleit M, van der Heijde D, Landewé R et al (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68:777–783
Lambert RG, Dhillon SS, Jaremko JL (2012) Advanced imaging of the axial skeleton in spondyloarthropathy: techniques, interpretation, and utility. Semin Musculoskelet Radiol 16:389–400
Diekhoff T, Hermann KG, Greese J et al (2017) Comparison of MRI with radiography for detecting structural lesions of the sacroiliac joint using CT as standard of reference: results from the SIMACT study. Ann Rheum Dis 76:1502–1508
Xie R, Sun D, Morelli JN, Yin C, Xiong Y, Li X (2020) Recognition of sacroiliac joint structural lesions: comparison of volumetric interpolated breath-hold examination (VIBE) sequences with different slice thicknesses to T1-weighted turbo-echo. Eur J Radiol 124:108849
Agresti A, Coull BA (1998) Approximate is better than “exact” for interval estimation of binomial proportions. Am Stat 52:119–126
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Weber U, Østergaard M, Lambert RG et al (2015) Candidate lesion-based criteria for defining a positive sacroiliac joint MRI in two cohorts of patients with axial spondyloarthritis. Ann Rheum Dis 74:1976–1982
Jans LBO, Chen M, Elewaut D et al (2021) MRI-based synthetic CT in the detection of structural lesions in patients with suspected sacroiliitis: comparison with MRI. Radiology 298:343–349
Diekhoff T, Greese J, Sieper J, Poddubnyy D, Hamm B, Hermann KA (2018) Improved detection of erosions in the sacroiliac joints on MRI with volumetric interpolated breath-hold examination (VIBE): results from the SIMACT study. Ann Rheum Dis 77:1585–1589
Hu L, Huang Z, Zhang X et al (2014) The performance of MRI in detecting subarticular bone erosion of sacroiliac joint in patients with spondyloarthropathy: a comparison with X-ray and CT. Eur J Radiol 83:2058–2064
Puhakka KB, Jurik AG, Egund N et al (2003) Imaging of sacroiliitis in early seronegative spondylarthropathy. Assessment of abnormalities by MR in comparison with radiography and CT. Acta Radiol 44:218–229
Baraliakos X, Hoffmann F, Deng X, Wang YY, Huang F, Braun J (2019) Detection of erosions in sacroiliac joints of patients with axial spondyloarthritis using the magnetic resonance imaging volumetric interpolated breath-hold examination. J Rheumatol 46:1445–1449
Chen M, Bird P, Jans L (2020) Emerging imaging techniques in spondyloarthritis: dual-energy computed tomography and new MRI sequences. Rheum Dis Clin North Am 46:287–296
Acknowledgements
We acknowledge Weiyin Vivian Liu from GE Healthcare for the technical support and manuscript revision. We also thank professor John N. Morelli for proofreading and editing the language of this paper.
Funding
This research was supported by the National Natural Science Foundation of China (NSFC) (No. 31630025 and 81930045) and Tongji Hospital Clinical Research Flagship Program (No. 2019CR102).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xiaoming Li.
Conflict of interest
One of the authors of this manuscript (Weiyin Vivian Liu) is an employee of GE Healthcare. The remaining authors declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, Y., Xiong, Y., Hou, B. et al. Comparison of zero echo time MRI with T1-weighted fast spin echo for the recognition of sacroiliac joint structural lesions using CT as the reference standard. Eur Radiol 32, 3963–3973 (2022). https://doi.org/10.1007/s00330-021-08513-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08513-5