Abstract
Objective
To investigate the radiological classification, gene-mutation status, and surgical prognosis of synchronous multiple primary lung cancer (sMPLC).
Methods
From January 2013 to October 2019, 192 consecutive patients with sMPLC were investigated. The clinical, CT, molecular, and pathological features of all patients were analyzed. Furthermore, the prognosis of 89 patients who only underwent surgical resection was evaluated.
Results
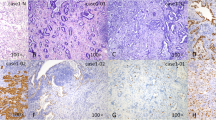
Among 192 patients, all lesions pathologically confirmed or highly suspected as tumors based on radiological findings were retrospectively analyzed, and the CT findings of sMPLC were classified into three types: (I) all lesions manifested as solid nodules/masses (14.06%, 27/192), (II) all lesions manifested as subsolid nodules/masses (43.23%, 83/192), and (III) tumor lesions manifested as a combination of ≥ 2 of the following patterns: solid nodules/masses, subsolid nodules/masses, cystic airspace, and focal consolidation (42.71%, 82/192). For 252 tumors undergoing epidermal growth factor receptor (EGFR)–mutation testing, the EGFR-mutation rate was higher in subsolid tumors than that in solid tumors (p < 0.05). Among 19 patients with all tumors undergoing surgery and driver-gene testing, genetic heterogeneity was prevalent among the multiple tumors (63.16%,12/19). The highest clinical stage of non-I, ipsilateral distribution of tumors, and CT classification of I indicated a poor prognosis for patients with sMPLC (all p < 0.05).
Conclusion
Subsolid lesions are the most common presentation of sMPLC. Genetic heterogeneity in driver mutations among sMPLC may be present. Prognosis in patients with sMPLC is determined by the highest clinical TNM stage, distribution, and radiological classification among the multiple tumors.
Key Points
• Synchronous multiple primary lung cancer (sMPLC) has three types of CT findings.
• Genetic heterogeneity may be prevalent among the multiple tumors.
• Prognosis in patients with sMPLC is associated with the highest clinical TNM stage, distribution, and radiological classification among the multiple tumors.



Similar content being viewed by others
Abbreviations
- ADC:
-
Adenocarcinoma
- CT:
-
Computed tomography
- EGFR:
-
Epidermal growth factor receptor
- GGO:
-
Ground-glass opacity
- IA:
-
Invasive adenocarcinoma
- LADC:
-
Lung adenocarcinoma
- mMPLC:
-
Metachronous multiple primary lung cancer
- MPLC:
-
Multiple primary lung cancer
- PACS:
-
Picture archiving and communication system
- PFS:
-
Progression-free survival
- sMPLC:
-
Synchronous multiple primary lung cancer
References
Siegel RL, Fedewa SA, Miller KD et al (2015) Cancer statistics for Hispanics/Latinos, 2015. CA Cancer J Clin 65:457–80
Martini N, Melamed MR (1975) Multiple primary lung cancers. J Thorac Cardiovasc Surg 70:606–12
Jeudy J, White CS, Munden RF, Boiselle PM (2008) Management of small (3–5-mm)pulmonary nodules at chest CT: global survey of thoracic radiologists. Radiology 247:847–53
Warth A, Macher-Goeppinger S, Muley T et al (2012) Clonality of multifocal non-small cell lung cancer: implications for staging and therapy. Eur Respir J 39:1437–42
Yu YC, Hsu PK, Yeh YC et al (2013) Surgical results of synchronous multiple primary lung cancers: similar to the stage-matched solitary primary lung cancers? Ann Thorac Surg 96:1966–74
Rostad H, Strand TE, Naalsund A, Norstein J (2008) Resected synchronous primary malignant lung tumors: a population-based study. Ann Thorac Surg 85:204–9
Nakata M, Sawada S, Yamashita M et al (2004) Surgical treatments for multiple primary adenocarcinoma of the lung. Ann Thorac Surg 78:1194–9
Kozower BD, Larner JM, Detterbeck FC, Jones DR (2013) Special treatment issues in non-small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 143:e369S-99S
Ye C, Wang J, Li W, Chai Y (2016) Novel strategy for synchronous multiple primary lung cancer displaying unique molecular profiles. Ann Thorac Surg 101:e45-7
Cao Y, Xu H, Liao M et al (2018) Associations between clinical data and computed tomography features in patients with epidermal growth factor receptor mutations in lung adenocarcinoma. Int J Clin Oncol 23:249–57
Liu Y, Kim J, Qu F et al (2016) CT features associated with epidermal growth factor receptor mutation status in patients with lung adenocarcinoma. Radiology 280:271–80
Voltolini L, Rapicetta C, Luzzi L et al (2010) Surgical treatment of synchronous multiple lung cancer located in a different lobe or lung: high survival in node-negative subgroup. Eur J Cardiothorac Surg 37:1198–204
Fabian T, Bryant AS, Mouhlas AL, Federico JA, Cerfolio RJ (2011) Survival after resection of synchronous non-small cell lung cancer. J Thorac Cardiovasc Surg 142:547–53
Finley DJ, Yoshizawa A, Travis W et al (2010) Predictors of outcomes after surgical treatment of synchronous primary lung cancers. J Thorac Oncol 5:197–205
Hattori A, Matsunaga T, Takamochi K, Oh S, Suzuki K (2017) Radiological classification of multiple lung cancers and the prognostic impact based on the presence of a ground glass opacity component on thin-section computed tomography. Lung Cancer 113:7–13
Hattori A, Takamochi K, Oh S, Suzuki K (2020) Prognostic classification of multiple primary lung cancers based on a ground-glass opacity component. Ann Thorac Surg 109:420–7
Aokage K, Miyoshi T, Ishii G et al (2018) Influence of ground glass opacity and the corresponding pathological findings on survival in patients with clinical stage I non-small cell lung cancer. J Thorac Oncol 13:533–42
Kim TH, Kim SJ, Ryu YH et al (2006) Differential CT features of infectious pneumonia versus bronchioloalveolar carcinoma (BAC) mimicking pneumonia. Eur Radiol 16:1763–8
Li Q, Li X, Li XY, Huo JW, Lv FJ, Luo TY (2020) Spectral CT in lung cancer: usefulness of iodine concentration for evaluation of tumor angiogenesis and prognosis. AJR Am J Roentgenol 215:595–602
Li TY (1989) CT diagnosis of pulmonary solitary nodule–a correlative study of CT, X-ray and pathology. Zhonghua Fang She Xue Za Zhi 23:346–9
Vazquez M, Carter D, Brambilla E et al (2009) Solitary and multiple resected adenocarcinomas after CT screening for lung cancer: histopathologic features and their prognostic implications. Lung Cancer 64:148–54
Moon Y, Lee KY, Park JK (2017) The prognosis of invasive adenocarcinoma presenting as ground-glass opacity on chest computed tomography after sublobar resection. J Thorac Dis 9:3782–92
Berry MF, Gao R, Kunder CA et al (2018) Presence of even a small ground-glass component in lung adenocarcinoma predicts better survival. Clin Lung Cancer 19:e47-51
Yang Y, Yang Y, Zhou X et al (2015) EGFR L858R mutation is associated with lung adenocarcinoma patients with dominant ground-glass opacity. Lung Cancer 87:272–7
Lee HJ, Kim YT, Kang CH et al (2013) Epidermal growth factor receptor mutation in lung adenocarcinomas: relationship with CT characteristics and histologic subtypes. Radiology 268:254–64
El Ghissassi F, Baan R, Straif K (2009) A review of human carcinogens–part D: radiation. Lancet Oncol 10:751–2
Shimada Y, Saji H, Otani K et al (2015) Survival of a surgical series of lung cancer patients with synchronous multiple ground-glass opacities, and the management of their residual lesions. Lung Cancer 88:174–80
Tanvetyanon T, Finley DJ, Fabian T et al (2013) Prognostic factors for survival after complete resections of synchronous lung cancers in multiple lobes: pooled analysis based on individual patient data. Ann Oncol 24:889–94
Griffioen GH, Lagerwaard FJ, Haasbeek CJ, Smit EF, Slotman BJ, Senan S (2013) Treatment of multiple primary lung cancers using stereotactic radiotherapy, either with or without surgery. Radiother Oncol 107:403–8
Jung EJ, Lee JH, Jeon K et al (2011) Treatment outcomes for patients with synchronous multiple primary non-small cell lung cancer. Lung Cancer. 73:237–42
Alam N, Darling G, Shepherd FA, Mackay JA, Evans WK (2006) Postoperative chemotherapy in nonsmall cell lung cancer: a systematic review. Ann Thorac Surg 81:1926–36
Ohde Y, Nagai K, Yoshida J et al (2003) The proportion of consolidation to ground-glass opacity on high resolution CT is a good predictor for distinguishing the population of non-invasive peripheral adenocarcinoma. Lung Cancer 42:303–10
Funding
This study has received funding from the Chongqing Science and Technology Commission (cstc2017jcyjAX0281 and cstc2016shms-ztzx10002) and Chongqing Health and Family Planning Commission (2022MSXM147) of China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Qi Li.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
This study and all its protocols were approved by the ethics committee of our institute, written informed consent was not required for this study due to the retrospective nature.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• case-control study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huo, Jw., Luo, Ty., He, Xq. et al. Radiological classification, gene-mutation status, and surgical prognosis of synchronous multiple primary lung cancer. Eur Radiol 32, 4264–4274 (2022). https://doi.org/10.1007/s00330-021-08464-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08464-x