Abstract
Objectives
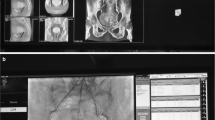
To evaluate the effects of center experience and a variety of patient- and procedure-related factors on patient radiation exposure during prostatic artery embolization (PAE) in three Scandinavian centers with different PAE protocols and levels of experience. Understanding factors that influence radiation exposure is crucial in effective patient selection and procedural planning.
Methods
Data were collected retrospectively for 352 consecutive PAE procedures from January 2015 to June 2020 at the three centers. Dose area product (DAP (Gy·cm2)) was selected as the primary outcome measure of radiation exposure. Multiple patient- and procedure-related explanatory variables were collected and correlated with the outcome variable. A multiple linear regression model was built to determine significant predictors of increased or decreased radiation exposure as reflected by DAP.
Results
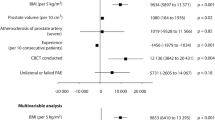
There was considerable variation in DAP between the centers. Intended unilateral PAE (p = 0.03) and each 10 additional patients treated (p = 0.02) were significant predictors of decreased DAP. Conversely, increased patient body mass index (BMI, p < 0.001), fluoroscopy time (p < 0.001), and number of digital subtraction angiography (DSA) acquisitions (p < 0.001) were significant predictors of increased DAP.
Conclusions
To minimize patient radiation exposure during PAE radiologists may, in collaboration with clinicians, consider unilateral embolization, pre-interventional CTA for procedure planning, using predominantly anteroposterior (AP) projections, and limiting the use of cone-beam CT (CBCT) and fluoroscopy.
Key Points
• Growing center experience and intended unilateral embolization decrease patient radiation exposure during prostatic artery embolization.
• Patient BMI, fluoroscopy time, and number of DSA acquisitions are associated with increased DAP during procedures.
• Large variation in radiation exposure between the centers may reflect the use of CTA before and CBCT during the procedure.


Similar content being viewed by others
Abbreviations
- AP:
-
Anteroposterior
- BMI:
-
Body mass index
- BPH:
-
Benign prostatic hyperplasia
- CBCT:
-
Cone beam computed tomography
- DAP:
-
Dose area product
- DSA:
-
Digital subtraction angiography
- LUTS:
-
Lower urinary tract symptoms
- PA:
-
Prostate artery
- PAE:
-
Prostatic artery embolization
- PV:
-
Prostate volume
- TURP:
-
Transurethral resection of the prostate
References
Ray AF, Powell J, Speakman MJ et al (2018) Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int 122:270–282
Xiang P, Guan D, Du Z et al (2021) Efficacy and safety of prostatic artery embolization for benign prostatic hyperplasia: a systematic review and meta-analysis of randomized controlled trials. Eur Radiol 31:4929–4946
Malling B, Røder MA, Brasso K, Forman J, Taudorf M, Lönn L (2019) Prostate artery embolisation for benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Radiol 29:287–298
Kably I, Acharya V, Richardson AJ, Bhatia S (2020) Prostatic artery embolization in refractory hematuria of prostatic origin. Tech Vasc Interv Radiol 23:100694
Malling B, Røder MA, Lindh M, Frevert S, Brasso K, Lönn L (2019) Palliative prostate artery embolization for prostate cancer: a case series. Cardiovasc Intervent Radiol 42:1405–1412
Foster HE, Dahm P, Kohler TS et al (2019) Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline amendment 2019. J Urol 202:592–598
Wang MQ, Duan F, Yuan K, Zhang GD, Yan J, Wang Y (2017) Benign prostatic hyperplasia: cone-beam CT in conjunction with DSA for identifying prostatic arterial anatomy. Radiology 282:271–280
Bilhim T (2019) Dealing with prostatic arteries—how many roads must a man walk down? J Vasc Interv Radiol 30:652–653
de Assis AM, Moreira AM, de Paula Rodrigues VC et al (2015) Pelvic arterial anatomy relevant to prostatic artery embolisation and proposal for angiographic classification. Cardiovasc Intervent Radiol 38:855–861
Schott P, Katoh M, Fischer N, Freyhardt P (2019) Radiation dose in prostatic artery embolization using cone-beam CT and 3D roadmap software. J Vasc Interv Radiol 30:1452–1458
Durack JC, Brown KT, Avignon G et al (2018) Assessment of automated cone-beam CT vessel identification software during transarterial hepatic embolisation: radiation dose, contrast medium volume, processing time, and operator perspectives compared to digital subtraction angiography. Clin Radiol 73:1057.e1-1057.e6
Goni H, Tsalafoutas IA, Tzortzis G et al (2005) Radiation doses to patients from digital subtraction angiography. Radiat Prot Dosimetry 117:251–255
Kriechenbauer BMT, Franiel T, Bürckenmeyer F et al (2020) Influence of interventionists’ experience on radiation exposure of patients who underwent prostate artery embolization: 4-year results from a retrospective, single-center study. Cardiovasc Intervent Radiol 43:1194–1201
Zumstein V, Binder J, Güsewell S et al (2021) Radiation exposure during prostatic artery embolisation: a systematic review and calculation of associated risks. Eur Urol Focus 7:608–611
du Pisanie J, Abumoussa A, Donovan K, Stewart J, Bagla S, Isaacson A (2019) Predictors of prostatic artery embolization technical outcomes: patient and procedural factors. J Vasc Interv Radiol 30:233–240
Lacayo EA, Khera SS, Spies JB (2020) Impact of patient and procedure-related factors on radiation exposure from uterine artery embolization. Cardiovasc Intervent Radiol 43:120–126
Barral M, Gardavaud F, Lassalle L et al (2021) Limiting radiation exposure during prostatic arteries embolization: influence of patient characteristics, anatomical conditions, and technical factors. Eur Radiol. https://doi.org/10.1007/s00330-021-07844-7
Hacking N, Vigneswaran G, Maclean D et al (2019) Technical and imaging outcomes from the UK Registry of Prostate Artery Embolization (UK-ROPE) Study: focusing on Predictors of Clinical Success. Cardiovasc Intervent Radiol 42:666–676
Carnevale FC, Moreira AM, Antunes AA (2014) The “PErFecTED Technique”: proximal embolization first, then embolize distal for benign prostatic hyperplasia. Cardiovasc Intervent Radiol 37:1602–1605
Nickoloff EL, Lu ZF, Dutta AK, So JC (2008) Radiation dose descriptors: BERT, COD, DAP, and other strange creatures. Radiographics 28:1439–1450
Vano E, Gonzalez L, Ten JI, Fernandez JM, Guibelalde E, Macaya C (2001) Skin dose and dose-area product values for interventional cardiology procedures. Br J Radiol 74:48–55
Le Heron JC (1992) Estimation of effective dose to the patient during medical x-ray examinations from measurements of the dose-area product. Phys Med Biol 37:2117–2126
United Nations Scientific Committee on Effects of Atomic Radiation (2017) UNSCEAR’s global survey of radiation exposure. United Nations Scientific Committee on Effects of Atomic Radiation, Vienna. Available via http://www.survey.unscear.org. Accessed 10 March 2021
R Core Team (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. Available via http://www.r-project.org. Accessed 1 May 2021
Bates DM, Maechler M, Bolker B (2012) lme4: Linear mixed-effects models using S4 classes. R package version 0.999999–0. Available via http://cran.r-project.org/web/packages/lme4/index.html. Accessed 1 May 2021
Moschouris H, Dimakis A, Papadaki MG et al (2021) Prostatic artery embolization performed in anteroposterior projections versus steep oblique projections: single centre retrospective comparative analysis. CVIR Endovasc 4:21
Andrade G, Khoury HJ, Garzón WJ et al (2017) Radiation exposure of patients and interventional radiologists during prostatic artery embolization: a prospective single-operator study. J Vasc Interv Radiol 28:517–521
Alaei P, Spezi E (2015) Imaging dose from cone beam computed tomography in radiation therapy. Phys Med 31:647–658
Lintin L, Barge T, Boardman P, Tong G, Tapping C (2021) Predictors of technical outcome for prostatic artery embolisation using pre-procedural CT angiography. Eur Radiol 31:1308–1315
Enderlein GF, Lehmann T, von Rundstedt F-C et al (2020) Prostatic artery embolization—anatomic Predictors of Technical Outcomes. J Vasc Interv Radiol 31:378–387
Brambilla M, Marano G, Dominietto M, Cotroneo AR, Carriero A (2004) Patient radiation doses and references levels in interventional radiology. Radiol Med (Torino) 107:408–418
Carnevale FC, Moreira AM, de Assis AM et al (2020) Prostatic artery embolization for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: 10 years’ experience. Radiology 296:444–451
Bilhim T, Pisco J, Rio Tinto H et al (2013) Unilateral versus bilateral prostatic arterial embolization for lower urinary tract symptoms in patients with prostate enlargement. Cardiovasc Intervent Radiol 36:403–411
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Lars Lönn.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
No complex statistical methods were necessary for this paper.
Informed consent
Institutional Review Board in each respective country granted approval for the collection of data related to PAE procedures in the specified timeframe for the purpose of analysis and publication. As the study was retrospective, it did not include any additional interaction with individual patients or include data from which individual patients could be identified in any way.
Ethical approval
Institutional Review Board approvals were obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in:
14 subjects in the Copenhagen cohort: Malling B, Røder MA, Lindh M, et al (2019) Palliative prostate artery embolization for prostate cancer: a case series. Cardiovasc Intervent Radiol 42:1405–1412.
25 subjects in the Oslo cohort: Kløw NE, Grøtta OJ, Bay D, Sandbæk G, Bjerklund Johansen TE, Hagen T, Baco E. Outcome after prostatic artery embolization in patients with symptomatic benign prostatic hyperplasia. Acta Radiol 2019 Sep;60(9):1175–1180.
37 subjects in the Helsingborg cohort: Hans Lindgren and Mats Bläckberg. Introduction of prostate artery embolization (PAE) in Sweden. Scand J Urol. 2019 Apr-Jun;53(2–3):151–155.
All three studies are unrelated to the current investigation and concern clinical outcomes of PAE.
Methodology
• Retrospective
• Observational
• Multicenter study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Svarc, P., Hagen, T., Waltenburg, H. et al. Center experience and other determinants of patient radiation exposure during prostatic artery embolization: a retrospective study in three Scandinavian centers. Eur Radiol 32, 2404–2413 (2022). https://doi.org/10.1007/s00330-021-08351-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08351-5