Abstract
Objectives
The aim of the study is to assess amide concentration changes in ALS patients compared with healthy controls by using quantitative amide proton transfer (APT) and multiparameter magnetic resonance imaging, and testing its correlation with clinical scores.
Methods
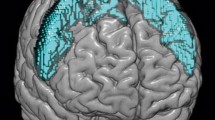
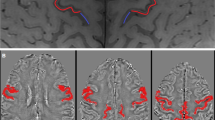
Sixteen ALS patients and sixteen healthy controls were recruited as part of the Canadian ALS Neuroimaging Consortium, and multimodal magnetic resonance imaging was performed at 3 T, including APT and diffusion imaging. Lorentz fitting was used to quantify the amide effect. Clinical disability was evaluated using the revised ALS functional rating scale (ALSFRS-R), and its correlation with image characteristics was assessed. The diagnostic performance of different imaging parameters was evaluated with receiver operating characteristic analysis.
Results
Our results showed that the amide peak was significantly different between the motor cortex and other gray matter territories within the brain of ALS patients (p < 0.001). Compared with controls, amide signal intensities in ALS were significantly reduced in the motor cortex (p < 0.001) and corticospinal tract (p = 0.046), while abnormalities were not detected using routine imaging methods. There was no significant correlation between amide and ALSFRS-R score. The diagnostic accuracy of the amide peak was superior to that of diffusion imaging.
Conclusions
This study demonstrated changes of amide signal intensities in the motor cortex and corticospinal tract of ALS patients.
Key Points
• The neurodegenerative disease amyotrophic lateral sclerosis (ALS) has a lack of objective imaging indicators for diagnosis and assessment.
• Analysis of amide proton transfer imaging revealed changes in the motor cortex and corticospinal tract of ALS patients that were not visible on standard magnetic resonance imaging.
• The diagnostic accuracy of the amide peak was superior to that of diffusion imaging.






Similar content being viewed by others
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- ALS:
-
Amyotrophic lateral sclerosis
- ALSFRS-R:
-
Revised ALS functional rating scale
- ANCOVA:
-
Analysis of covariance
- APT:
-
Amide proton transfer
- ASICs:
-
Acid-sensing ion channel
- CALSNIC:
-
Canadian ALS neuroimaging consortium
- DTI:
-
Diffusion tensor imaging
- FA:
-
Fractional anisotropy
- MT:
-
Magnetization transfer
- NOE:
-
Nuclear Overhauser effect
- RIPK1:
-
Receptor-interacting serine/threonine-protein kinase 1
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- WASSR:
-
Water saturation shift reference
References
Kiernan MC, Vucic S, Cheah BC et al (2011) Amyotrophic lateral sclerosis. Lancet 377:942–955
McCampbell A, Cole T, Wegener AJ et al (2018) Antisense oligonucleotides extend survival and reverse decrement in muscle response in ALS models. J Clin Investig 128:3558–3567
Scott A (2017) Drug therapy: on the treatment trail for ALS. Nature 550:S120–s121
Ludolph A, Drory V, Hardiman O et al (2015) A revision of the El Escorial criteria-2015. Amyotroph Lateral Scler Frontotemporal Degener 16:291–292
Schrooten M, Smetcoren C, Robberecht W, Van Damme P (2011) Benefit of the Awaji diagnostic algorithm for amyotrophic lateral sclerosis: a prospective study. Ann Neurol 70:79–83
Menke RA, Agosta F, Grosskreutz J, Filippi M, Turner MR (2017) Neuroimaging endpoints in amyotrophic lateral sclerosis. Neurotherapeutics 14:11–23
Simon NG, Turner MR, Vucic S et al (2014) Quantifying disease progression in amyotrophic lateral sclerosis. Ann Neurol 76:643–657
Chakraborty S, Gupta A, Nguyen T, Bourque P (2015) The “motor band sign:” susceptibility-weighted imaging in amyotrophic lateral sclerosis. Can J Neurol Sci 42:260–263
Han J, Ma L (2010) Study of the features of proton MR spectroscopy (1H-MRS) on amyotrophic lateral sclerosis. J Magn Reson Imaging 31:305–308
Chen Z, Ma L (2010) Grey matter volume changes over the whole brain in amyotrophic lateral sclerosis: a voxel-wise meta-analysis of voxel based morphometry studies. Amyotroph Lateral Scler 11:549–554
Dai Z, Chen Y, Yan G, Shen Z, Wu R (2019) Progress of magnetic resonance imaging in amyotrophic lateral sclerosis. Radiol Infect Dis 6:1–7
Zhou J, Payen J-F, Wilson DA, Traystman RJ, van Zijl PC (2003) Using the amide proton signals of intracellular proteins and peptides to detect pH effects in MRI. Nat Med 9:1085–1090
Jones KM, Pollard AC, Pagel MD (2018) Clinical applications of chemical exchange saturation transfer (CEST) MRI. J Magn Reson Imaging 47:11–27
Zhou J, Lal B, Wilson DA, Laterra J, van Zijl P (2003) Amide proton transfer (APT) contrast for imaging of brain tumors. Magn Reson Med 50:1120–1126
Zhou J, Tryggestad E, Wen Z et al (2011) Differentiation between glioma and radiation necrosis using molecular magnetic resonance imaging of endogenous proteins and peptides. Nat Med 17:130–134
Lin G, Zhuang C, Shen Z et al (2018) APT weighted MRI as an effective imaging protocol to predict clinical outcome after acute ischemic stroke. Front Neurol 9:901
Zhang H, Wang W, Jiang S et al (2017) Amide proton transfer-weighted MRI detection of traumatic brain injury in rats. J Cereb Blood Flow Metab 37:3422–3432
Lokesh N, Seegerer A, Hioe J, Gschwind RM (2018) Chemical exchange saturation transfer in chemical reactions: a mechanistic tool for NMR detection and characterization of transient intermediates. J Am Chem Soc 140:1855–1862
Liu G, Liang Y, Bar-Shir A et al (2011) Monitoring enzyme activity using a diamagnetic chemical exchange saturation transfer MRI contrast agent. J Am Chem Soc 133(41):16326–16329
Zhuang Z, Shen Z, Chen Y et al (2018) Mapping the changes of glutamate using glutamate chemical exchange saturation transfer (GluCEST) technique in a traumatic brain injury model: a longitudinal pilot study. ACS Chem Nerosci 10(1):649–657
van Zijl PCM, Yadav NN (2011) Chemical exchange saturation transfer (CEST): what is in a name and what isn’t? Magn Reson Med 65:927–948
Sun PZ, Xiao G, Zhou IY, Guo Y, Wu R (2016) A method for accurate pH mapping with chemical exchange saturation transfer (CEST) MRI. Contrast Media Mol Imaging 11:195–202
Wu R, Xiao G, Zhou IY, Ran C, Sun PZ (2015) Quantitative chemical exchange saturation transfer (qCEST) MRI - omega plot analysis of RF-spillover-corrected inverse CEST ratio asymmetry for simultaneous determination of labile proton ratio and exchange rate. NMR Biomed 28:376–383
Dai Z, Ji J, Xiao G et al (2014) Magnetization transfer prepared gradient echo MRI for CEST imaging. PLoS One 9:e112219
Dupuis L, Pradat P-F, Ludolph AC, Loeffler J-P (2011) Energy metabolism in amyotrophic lateral sclerosis. Lancet Neurol 10:75–82
Pyra T, Hui B, Hanstock C et al (2010) Combined structural and neurochemical evaluation of the corticospinal tract in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 11:157–165
Wong JC, Concha L, Beaulieu C, Johnston W, Allen PS, Kalra S (2007) Spatial profiling of the corticospinal tract in amyotrophic lateral sclerosis using diffusion tensor imaging. J Neuroimaging 17:234–240
Wu R, Bruening R (2006) Comparison of diffusion-weighted MR imaging and T2-weighted MR imaging in patients with amyotrophic lateral sclerosis. Neuroradiol J 19:705–710
Cedarbaum JM, Stambler N, Malta E et al (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. J Neurol Sci 169:13–21
Kim M, Gillen J, Landman BA, Zhou J, van Zijl PCM (2009) Water saturation shift referencing (WASSR) for chemical exchange saturation transfer (CEST) experiments. Magn Reson Med 61:1441–1450
Zhou J, Heo HY, Knutsson L, van Zijl PCM, Jiang S (2019) APT-weighted MRI: techniques, current neuro applications, and challenging issues. J Magn Reson Imaging 50:347–364
Wang E, Wu Y, Cheung JS et al (2019) Mapping tissue pH in an experimental model of acute stroke - determination of graded regional tissue pH changes with non-invasive quantitative amide proton transfer MRI. Neuroimage 191:610–617
By S, Barry RL, Smith AK et al (2018) Amide proton transfer CEST of the cervical spinal cord in multiple sclerosis patients at 3T. Magn Reson Med 79:806–814
Lee S, Shang Y, Redmond SA et al (2016) Activation of HIPK2 promotes ER stress-mediated neurodegeneration in amyotrophic lateral sclerosis. Neuron 91:41–55
Hughes J (1982) Pathology of amyotrophic lateral sclerosis. Adv Neurol 36:61–74
Dodge JC, Treleaven CM, Fidler JA et al (2013) Metabolic signatures of amyotrophic lateral sclerosis reveal insights into disease pathogenesis. Proc Natl Acad Sci U S A 110:10812–10817
Szelechowski M, Amoedo N, Obre E et al (2018) Metabolic reprogramming in amyotrophic lateral sclerosis. Sci Rep 8:3953
Ahmed RM, Irish M, Piguet O et al (2016) Amyotrophic lateral sclerosis and frontotemporal dementia: distinct and overlapping changes in eating behaviour and metabolism. Lancet Neurol 15:332–342
Kori M, Aydın B, Unal S, Arga KY, Kazan D (2016) Metabolic biomarkers and neurodegeneration: a pathway enrichment analysis of Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis. OMICS 20:645–661
Zhang F, Chen G, He M et al (2018) Altered white matter microarchitecture in amyotrophic lateral sclerosis: a voxel-based meta-analysis of diffusion tensor imaging. Neuroimage Clin 19:122–129
List J, Kohl Z, Winkler J, Marxreiter F, Doerfler A, Schmidt MA (2019) Ascending axonal degeneration of the corticospinal tract in pure hereditary spastic paraplegia: a cross-sectional DTI study. Brain Sci 9
Li C, Peng S, Wang R et al (2014) Chemical exchange saturation transfer MR imaging of Parkinson’s disease at 3 tesla. Eur Radiol 24:2631–2639
Li C, Wang R, Chen H et al (2015) Chemical exchange saturation transfer MR imaging is superior to diffusion-tensor imaging in the diagnosis and severity evaluation of Parkinson’s disease: a study on substantia nigra and striatum. Front Aging Neurosci 7:198
Togao O, Yoshiura T, Keupp J et al (2013) Amide proton transfer imaging of adult diffuse gliomas: correlation with histopathological grades. Neuro Oncol 16:441–448
Goldenberg JM, Pagel MD (2019) Assessments of tumor metabolism with CEST MRI. NMR Biomed 32:e3943
Roccatagliata L, Bonzano L, Mancardi G, Canepa C, Caponnetto C (2009) Detection of motor cortex thinning and corticospinal tract involvement by quantitative MRI in amyotrophic lateral sclerosis. Amyotroph Lateral Scler 10:47–52
Wang S, Poptani H, Woo JH et al (2006) Amyotrophic lateral sclerosis: diffusion-tensor and chemical shift MR imaging at 3.0 T. Radiology 239:831–838
Lindeman LR, Randtke EA, High RA, Jones KM, Howison CM, Pagel MD (2018) A comparison of exogenous and endogenous CEST MRI methods for evaluating in vivo pH. Magn Reson Med 79:2766–2772
Albatany M, Li A, Meakin S, Bartha R (2018) Dichloroacetate induced intracellular acidification in glioblastoma: in vivo detection using AACID-CEST MRI at 9.4 tesla. J Neurooncol 136:255–262
Ferri A, Coccurello R (2017) What is “hyper” in the ALS hypermetabolism? Mediators Inflamm 2017:7821672
Tefera TW, Tan KN, McDonald TS, Borges K (2017) Alternative fuels in epilepsy and amyotrophic lateral sclerosis. Neurochem Res 42:1610–1620
Hermosura MC, Garruto RM (2007) TRPM7 and TRPM2-candidate susceptibility genes for Western Pacific ALS and PD? Biochim Biophys Acta 1772:822–835
Pal B (2018) Involvement of extrasynaptic glutamate in physiological and pathophysiological changes of neuronal excitability. Cell Mol Life Sci 75:2917–2949
Blasco H, Mavel S, Corcia P, Gordon PH (2014) The glutamate hypothesis in ALS: pathophysiology and drug development. Curr Med Chem 21:3551–3575
Lawton KA, Cudkowicz ME, Brown MV et al (2012) Biochemical alterations associated with ALS. Amyotroph Lateral Scler 13:110–118
Ikawa M, Okazawa H, Tsujikawa T et al (2015) Increased oxidative stress is related to disease severity in the ALS motor cortex: a PET study. Neurology 84:2033–2039
Behan AT, Breen B, Hogg M et al (2013) Acidotoxicity and acid-sensing ion channels contribute to motoneuron degeneration. Cell Death Differ 20:589–598
Friese MA, Craner MJ, Etzensperger R et al (2007) Acid-sensing ion channel-1 contributes to axonal degeneration in autoimmune inflammation of the central nervous system. Nat Med 13:1483–1489
Nuzziello N, Liguori M (2019) The microRNA centrism in the orchestration of neuroinflammation in neurodegenerative diseases. Cells 8
Sun PZ, Wang Y, Dai ZZ, Xiao G, Wu RH (2014) Quantitative chemical exchange saturation transfer (qCEST) MRI - RF spillover effect-corrected omega plot for simultaneous determination of labile proton fraction ratio and exchange rate. Contrast Media Mol Imaging 9:268–275
Chitnis T, Weiner HL (2017) CNS inflammation and neurodegeneration. J Clin Invest 127:3577–3587
Ito Y, Ofengeim D, Najafov A et al (2016) RIPK1 mediates axonal degeneration by promoting inflammation and necroptosis in ALS. Science 353:603–608
Zaiss M, Kunz P, Goerke S, Radbruch A, Bachert P (2013) MR imaging of protein folding in vitro employing nuclear-Overhauser-mediated saturation transfer. NMR Biomed 26:1815–1822
Jenabi M, Peck KK, Young RJ, Brennan N, Holodny AI (2015) Identification of the corticobulbar tracts of the tongue and face using deterministic and probabilistic DTI fiber tracking in patients with brain tumor. AJNR Am J Neuroradiol 36:2036–2041
Guo YL, Li SJ, Zhang ZP et al (2016) Parameters of diffusional kurtosis imaging for the diagnosis of acute cerebral infarction in different brain regions. Exp Ther Med 12:933–938
Zhang H, Kang H, Zhao X et al (2016) Amide proton transfer (APT) MR imaging and magnetization transfer (MT) MR imaging of pediatric brain development. Eur Radiol 26:3368–3376
Bellani M, Boschello F, Delvecchio G et al (2016) DTI and myelin plasticity in bipolar disorder: integrating neuroimaging and neuropathological findings. Front Psychiatry 7:21
Wu Y, Zhou IY, Lu D et al (2018) pH-sensitive amide proton transfer effect dominates the magnetization transfer asymmetry contrast during acute ischemia-quantification of multipool contribution to in vivo CEST MRI. Magn Reson Med 79:1602–1608
Khlebnikov V, Siero JCW, Bhogal AA, Luijten PR, Klomp DWJ, Hoogduin H (2018) Establishing upper limits on neuronal activity-evoked pH changes with APT-CEST MRI at 7 T. Magn Reson Med 80:126–136
Xu X, Yadav NN, Zeng H et al (2016) Magnetization transfer contrast-suppressed imaging of amide proton transfer and relayed nuclear overhauser enhancement chemical exchange saturation transfer effects in the human brain at 7T. Magn Reson Med 75:88–96
Verstraete E, Polders DL, Mandl RC et al (2014) Multimodal tract-based analysis in ALS patients at 7T: a specific white matter profile? Amyotroph Lateral Scler Frontotemporal Degener 15:84–92
Wu B, Warnock G, Zaiss M et al (2016) An overview of CEST MRI for non-MR physicists. EJNMMI Phys 3:19
Cai K, Singh A, Poptani H et al (2015) CEST signal at 2 ppm (CEST@ 2ppm) from Z-spectral fitting correlates with creatine distribution in brain tumor. NMR Biomed 28:1–8
Fieremans E, Jensen JH, Helpern JA (2011) White matter characterization with diffusional kurtosis imaging. Neuroimage 58:177–188
Acknowledgments
Grateful acknowledgment is made to Dr. Mark D. Pagel from MD Anderson Cancer Center and Dr. Edward A. Randtke from the University of Arizona for technical assistance with pulse sequence implementation.
Funding
This study has received funding from the Canadian Institutes of Health Research to A.H.W.; the ALS Society of Canada and Brain Canada to S.K.; the Natural Science Foundation of China (grant numbers 81471730, 31870981) to R.W.; the 2020 La Ka Shing Foundation Cross-DisciplinaryResearch Grant (grant number 2020LKSFG06C) to Z.D.; the Department of Education Guangdong Province (grant number 2020KZDZX1085) to Z.D. and the Natural Science Foundation of Guangdong Province (grant number 2018A030307057) to Z.D.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Alan H. Wilman.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors, Professor Sanjay Kalra, has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• case-control study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dai, Z., Kalra, S., Mah, D. et al. Amide signal intensities may be reduced in the motor cortex and the corticospinal tract of ALS patients. Eur Radiol 31, 1401–1409 (2021). https://doi.org/10.1007/s00330-020-07243-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07243-4