Abstract
Objectives
The purpose of this study was to evaluate the 10-year overall survival and local tumor progression (LTP) of percutaneous radiofrequency ablation (RFA) for single nodular hepatocellular carcinoma (HCC) < 3 cm using a large longitudinal hospital registry and clinical factors associated with overall survival and LTP.
Methods
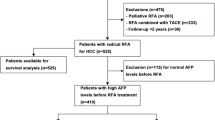
A total of 467 newly diagnosed patients with single nodular HCC < 3 cm who underwent RFA as first-line therapy between January 2008 to December 2016 were analyzed. Overall survival and LTP were estimated using the Kaplan-Meier method. Cox regression and competing risks Cox regression analysis were performed to identify prognostic factors for overall survival and LTP, respectively.
Results
The 5- and 10-year overall survival rates after RFA were 83.7% and 74.2%, respectively. LTP (hazard ratio (HR), 2.03; 95% confidence interval (CI), 1.19–3.47) was one of the important factors for overall survival after RFA. The 5- and 10-year LTP rates after RFA were 20.4% and 25.1%, respectively. Periportal location (subdistribution HR, 2.29; 95% CI, 1.25–4.21), subphrenic location (2.25, 1.34–3.86), size ≥ 1.5–< 2.0 cm (1.88, 1.05–3.39), and size ≥ 2.0 cm (2.10, 1.14–3.86) were independent factors for LTP.
Conclusion
Ten-year therapeutic outcomes of percutaneous RFA as first-line therapy were excellent for single HCC < 3 cm. LTP was an important prognostic factor for overall survival after RFA. Periportal and subphrenic location of HCCs and tumor size were predictors for the development of LTP after RFA.
Key Points
• Updated 10-year survival outcome of percutaneous radiofrequency ablation as first-line therapy for single hepatocellular carcinoma < 3 cm was higher than previously reported.
• Local tumor progression was an important prognostic factor for overall survival after percutaneous radiofrequency ablation.
• Periportal and subphrenic location of hepatocellular carcinomas and tumor size were predictors for the development of local tumor progression after percutaneous radiofrequency ablation.


Similar content being viewed by others
Abbreviations
- AFP:
-
Alpha-fetoprotein
- AIR:
-
Aggressive intrasegmental recurrence
- CI:
-
Confidence interval
- EM:
-
Extra-hepatic metastasis
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- IDR:
-
Intra-hepatic distant recurrence
- LTP:
-
Local tumor progression
- RFA:
-
Radiofrequency ablation
- US:
-
Ultrasound
References
Cucchetti A, Piscaglia F, Cescon M et al (2013) Cost-effectiveness of hepatic resection versus percutaneous radiofrequency ablation for early hepatocellular carcinoma. J Hepatol 59:300–307
Ng K, Chok K, Chan A et al (2017) Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br J Surg 104:1775–1784
Crocetti L (2018) Radiofrequency ablation versus resection for small hepatocellular carcinoma: are randomized controlled trials still needed? Radiology 287:473–475
Xu X-L, Liu X-D, Liang M, Luo B-M (2017) Radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma: systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Radiology 287:461–472
Hocquelet A, Aube C, Rode A et al (2017) Comparison of no-touch multi-bipolar vs. monopolar radiofrequency ablation for small HCC. J Hepatol 66:67–74
Choi TW, Lee JM, Lee DH et al (2017) Percutaneous dual-switching monopolar radiofrequency ablation using a separable clustered electrode: a preliminary study. Korean J Radiol 18:799–808
Song KD, Lee MW, Rhim H et al (2018) Percutaneous US/MRI fusion-guided radiofrequency ablation for recurrent subcentimeter hepatocellular carcinoma: technical feasibility and therapeutic outcomes. Radiology 288:878–886
Lee MW (2014) Fusion imaging of real-time ultrasonography with CT or MRI for hepatic intervention. Ultrasonography 33:227–239
Kim HD, Lim YS, Han S et al (2015) Evaluation of early-stage hepatocellular carcinoma by magnetic resonance imaging with gadoxetic acid detects additional lesions and increases overall survival. Gastroenterology 148:1371–1382
Korean Association for the Study of the Liver (KASL) (2018) 2017 KASL clinical practice guidelines management of hepatitis C: treatment of chronic hepatitis C. Clin Mol Hepatol 24:169–229
Forner A, Reig M, Bruix J (2018) Hepatocellular carcinoma. Lancet 391:1301–1314
Korean Association for the Study of the Liver (2016) KASL clinical practice guidelines: management of chronic hepatitis B. Clin Mol Hepatol 22:18–75
Francica G, Saviano A, De Sio I et al (2013) Long-term effectiveness of radiofrequency ablation for solitary small hepatocellular carcinoma: a retrospective analysis of 363 patients. Dig Liver Dis 45:336–341
Brunello F, Cantamessa A, Gaia S et al (2013) Radiofrequency ablation: technical and clinical long-term outcomes for single hepatocellular carcinoma up to 30 mm. Eur J Gastroenterol Hepatol 25:842–849
Bruix J, Sherman M, Practice Guidelines Committee, American Association for the Study of Liver Diseases (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
Kang TW, Lim HK, Lee MW et al (2016) Long-term therapeutic outcomes of radiofrequency ablation for subcapsular versus nonsubcapsular hepatocellular carcinoma: a propensity score matched study. Radiology 280:300–312
Ahmed M, Solbiati L, Brace CL et al (2014) Image-guided tumor ablation: standardization of terminology and reporting criteria--a 10-year update. Radiology 273:241–260
Kang TW, Lim HK, Lee MW et al (2015) Aggressive intrasegmental recurrence of hepatocellular carcinoma after radiofrequency ablation: risk factors and clinical significance. Radiology 276:274–285
Lu DS, Raman SS, Limanond P et al (2003) Influence of large peritumoral vessels on outcome of radiofrequency ablation of liver tumors. J Vasc Interv Radiol 14:1267–1274
Lee DH, Lee JM, Kang TW et al (2018) Clinical outcomes of radiofrequency ablation for early hypovascular HCC: a multicenter retrospective study. Radiology 286:338–349
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Kim YS, Lim HK, Rhim H et al (2013) Ten-year outcomes of percutaneous radiofrequency ablation as first-line therapy of early hepatocellular carcinoma: analysis of prognostic factors. J Hepatol 58:89–97
Shiina S, Tateishi R, Arano T et al (2012) Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol 107:569–577 quiz 578
Wang X, Sofocleous CT, Erinjeri JP et al (2013) Margin size is an independent predictor of local tumor progression after ablation of colon cancer liver metastases. Cardiovasc Intervent Radiol 36:166–175
Kim YS, Lee WJ, Rhim H, Lim HK, Choi D, Lee JY (2010) The minimal ablative margin of radiofrequency ablation of hepatocellular carcinoma (> 2 and < 5 cm) needed to prevent local tumor progression: 3D quantitative assessment using CT image fusion. AJR Am J Roentgenol 195:758–765
Livraghi T, Meloni F, Di Stasi M et al (2008) Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in cirrhosis: is resection still the treatment of choice? Hepatology 47:82–89
Lee MW, Raman SS, Asvadi NH et al (2017) Radiofrequency ablation of hepatocellular carcinoma as bridge therapy to liver transplantation: a 10-year intention-to-treat analysis. Hepatology 65:1979–1990
Liu W, Zheng Y, He W et al (2018) Microwave vs radiofrequency ablation for hepatocellular carcinoma within the Milan criteria: a propensity score analysis. Aliment Pharmacol Ther 48:671–681
Nault J-C, Sutter O, Nahon P, Ganne-Carrié N, Séror O (2018) Percutaneous treatment of hepatocellular carcinoma: state of the art and innovations. J Hepatol 68:783–797
Schullian P, Putzer D, Laimer G, Levy E, Bale R (2019) Feasibility, safety, and long-term efficacy of stereotactic radiofrequency ablation for tumors adjacent to the diaphragm in the hepatic dome: a case-control study. Eur Radiol. https://doi.org/10.1007/s00330-019-06399-y
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Song KD, Lim HK, Rhim H et al (2019) Hepatic resection vs percutaneous radiofrequency ablation of hepatocellular carcinoma abutting right diaphragm. World J Gastrointest Oncol 11:227–237
Lee S, Kang TW, Cha DI et al (2018) Radiofrequency ablation vs. surgery for perivascular hepatocellular carcinoma: propensity score analyses of long-term outcomes. J Hepatol 69:70–78
Angonese C, Baldan A, Cillo U et al (2006) Complications of radiofrequency thermal ablation in hepatocellular carcinoma: what about “explosive” spread? Gut 55:435–436
Marrero JA, Kulik LM, Sirlin CB et al (2018) Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 68:723–750
Funding
This study has received funding by Johnson and Johnson Medical Devices in the data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hyo Keun Lim.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Danbee Kang, one of the authors, has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval of the Samsung Medical Center was obtained.
Study subjects or cohorts overlap
Not applicable
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Lee, M.W., Kang, D., Lim, H.K. et al. Updated 10-year outcomes of percutaneous radiofrequency ablation as first-line therapy for single hepatocellular carcinoma < 3 cm: emphasis on association of local tumor progression and overall survival. Eur Radiol 30, 2391–2400 (2020). https://doi.org/10.1007/s00330-019-06575-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06575-0