Abstract
Objective
To retrospectively analyze the computed tomography (CT) features in patients with pre-invasive lesions and early-stage lung adenocarcinoma and to explore the correlation between tumor morphological changes and pathological diagnoses.
Materials and methods
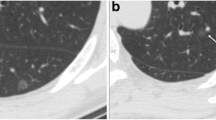
CT morphological characteristics in 2106 patients with pre-invasive (stage 0) and early-stage (stage I) lung adenocarcinoma were analyzed; lesions were confirmed by surgical pathology. Based on the morphological characteristics, the lesions were divided into eight types: I (cotton ball, ground-glass nodules), II (solid fill), III (granular), IV (dendriform), V (bubble-like lucencies), VI (alveolate or honeycomb), VII (scar-like), and VIII (notched or umbilication). The different distributions of eight morphological types in pathological types of the lesions and subtypes of invasive adenocarcinoma were analyzed by chi-squared or Fisher’s exact test. Correlation between the percentage of ground-glass opacity in the lesions and pathology types were analyzed by two-tailed Pearson’s test.
Results
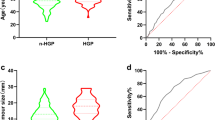
A negative correlation was observed between the pathological types and proportion of ground-glass component in the lesions (p < 0.001 and r = − 0.583). Significant differences in morphological characteristics among various pathological types of pre-invasive lesions and early lung adenocarcinomas were observed (p < 0.05). Furthermore, among the different pathological subtypes of stage I invasive adenocarcinoma, the differences in their manifestation as morphological types I, II, III, and VI were statistically significant (p < 0.05).
Conclusion
The eight types of morphological classification of pre-invasive lesions and early-stage (stage 0 or stage I) lung adenocarcinoma has different pathological bases, and morphological classification may be useful for the diagnosis and differential diagnosis of lung adenocarcinoma.
Key Points
• CT morphological classification of pre-invasive lesions and lung adenocarcinoma is intuitive.
• CT morphological classification characterizes morphological changes of the entire lesion.
• Different pathological types of lung adenocarcinoma have different morphological features.


Similar content being viewed by others
Abbreviations
- AAH:
-
Atypical adenomatous hyperplasia
- AIS:
-
Adenocarcinoma in situ
- CPR:
-
Curved planar reformation
- GGN:
-
Ground-glass nodule
- GGO:
-
Ground-glass opacity
- IAC:
-
Invasive adenocarcinoma
- LLL:
-
Left lower lobe
- LUL:
-
Left upper lobe
- mGGN:
-
Mixed ground-glass nodule
- MIA:
-
Minimal invasive adenocarcinoma
- MIP:
-
Maximum intensity projection
- MPR:
-
Multi-planar reformation
- pGGN:
-
Pure ground-glass nodule
- RLL:
-
Right lower lobe
- RML:
-
Right middle lobe
- RUL:
-
Right upper lobe
- VR:
-
Volume rendering
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65(2):87–108
Chen F, Cole P, Bina WF (2007) Time trend and geographic patterns of lung adenocarcinoma in the United States, 1973–2002. Cancer Epidemiol Biomarkers Prev 16(12):2724–2729
Zhang Y, Shen Y, Qiang JW, Ye JD, Zhang J, Zhao RY (2016) HRCT features distinguishing pre-invasive from invasive pulmonary adenocarcinomas appearing as ground-glass nodules. Eur Radiol 26(9):2921–2928
Wu F, Tian SP, Jin X et al (2017) CT and histopathologic characteristics of lung adenocarcinoma with pure ground-glass nodules 10 mm or less in diameter. Eur Radiol 27(10):4037–4043
Gao F, Sun Y, Zhang G, Zheng X, Li M, Hua Y (2018) CT characterization of different pathological types of subcentimeter pulmonary ground-glass nodular lesions. Br J Radiol:20180204
Mao H, Labh K, Han F, Jiang S, Yang Y, Sun X (2016) Diagnosis of the invasiveness of lung adenocarcinoma manifesting as ground glass opacities on high-resolution computed tomography. Thorac Cancer 7(1):129–135
Goldstraw P, Chansky K, Crowley J et al (2016) The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11(1):39–51
Travis WD, Brambilla E, Noguchi M et al (2011) International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6(2):244–285
Kim HY, Shim YM, Lee KS, Han J, Yi CA, Kim YK (2007) Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 245(1):267–275
Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS (2002) CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 178(5):1053–1057
Ko JP (2005) Lung nodule detection and characterization with multi-slice CT. J Thorac Imaging 20(3):196–209
Aoki T, Tomoda Y, Watanabe H et al (2001) Peripheral lung adenocarcinoma: correlation of thin-section CT findings with histologic prognostic factors and survival. Radiology 220(3):803–809
Madri JA, Carter D (1984) Scar cancers of the lung: origin and significance. Hum Pathol 15(7):625–631
Nambu A, Araki T, Taguchi Y et al (2005) Focal area of ground-glass opacity and ground-glass opacity predominance on thin-section CT: discrimination between neoplastic and non-neoplastic lesions. Clin Radiol 60(9):1006–1017
Winer-Muram HT (2006) The solitary pulmonary nodule. Radiology 239(1):34–49
Gao F, Li M, Ge X et al (2013) Multi-detector spiral CT study of the relationships between pulmonary ground-glass nodules and blood vessels. Eur Radiol 23(12):3271–3277
Lee HY, Lee KS, Han J et al (2009) Mucinous versus nonmucinous solitary pulmonary nodular bronchioloalveolar carcinoma: CT and FDG PET findings and pathologic comparisons. Lung Cancer 65(2):170–175
Gaeta M, Vinci S, Minutoli F et al (2002) CT and MRI findings of mucin-containing tumors and pseudotumors of the thorax: pictorial review. Eur Radiol 12(1):181–189
She Y, Zhao L, Dai C et al (2017) Preoperative nomogram for identifying invasive pulmonary adenocarcinoma in patients with pure ground-glass nodule: a multi-institutional study. Oncotarget 8(10):17229–17238
Wu F, Cai ZL, Tian SP et al (2015) Correlations between pathologic subtypes/immunohistochemical implication and CT characteristics of lung adenocarcinoma ≤ = 1 cm with ground-glass opacity. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 37(2):163–170
Saito H, Yamada K, Hamanaka N et al (2009) Initial findings and progression of lung adenocarcinoma on serial computed tomography scans. J Comput Assist Tomogr 33(1):42–48
Bobba RK, Holly JS, Loy T, Perry MC (2011) Scar carcinoma of the lung: a historical perspective. Clin Lung Cancer 12(3):148–154
Gao F, Ge X, Li M et al (2015) CT features of lung scar cancer. J Thorac Dis 7(3):273–280
Yang X, Soimakallio S (1997) Pleural signs of small peripheral pulmonary masses: pathologic correlation with chest radiographs and diagnostic value. Eur J Radiol 25(2):146–151
Yoshizawa A, Motoi N, Riely GJ et al (2011) Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 24(5):653–664
Acknowledgements
I would like to express my gratitude to all those who helped me during the writing of this paper.
Funding
This study has received funding by the Research Program of Shanghai Hospital Development Center (SHDC22015025) and the Medical Imaging Key Program of Wise Healthcare Technology 120, Health Commission of Shanghai (2018ZHYL0103).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Ming Li.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in “CT features of lung scar cancer”. J Thorac Dis 2015;7(3):273–80.
Methodology
• retrospective
• diagnostic/observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Gao, F., Li, M., Zhang, Z. et al. Morphological classification of pre-invasive lesions and early-stage lung adenocarcinoma based on CT images. Eur Radiol 29, 5423–5430 (2019). https://doi.org/10.1007/s00330-019-06149-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06149-0