Abstract
Purpose
To evaluate the appearance of mastoid and epitympanic obliteration using S53P4 bioactive glass (BG) granules in high-resolution computed tomography (HRCT) and MRI.
Materials and methods
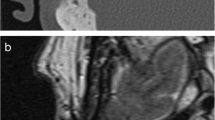
Patients undergoing mastoid and epitympanic obliteration between May 2013 and December 2015 were prospectively included in an uncontrolled clinical study. All patients underwent a temporal HRCT scan 1 year after surgery, aimed at evaluating the attenuation, homogeneity, and osseointegration of the BG granules, as well as the ventilation of the middle ear and the volume of the obliterated paratympanic spaces. If a cholesteatoma was found during surgery, additional MRI, including at least pre- and post-contrast T1-weighted, T2-weighted, and axial non-echo-planar diffusion-weighted (DW) sequences, was performed 1 year after surgery, to study the normal signal of the BG granules and the presence of residual cholesteatoma and/or other temporal bone pathologies.
Results
Seventy cases were included. On 1-year HRCT, the mean attenuation of the BG granules was 888.34 ± 166.10 HU. The obliteration was found to be mostly homogeneous with partial osseointegration. The appearance of the BG granules having a low-intensity signal in T2-weighted imaging and DW MRI was always different from the appearance of cholesteatoma. A longer follow-up has shown no attenuation or signal modification of the BG granules compared with the 1-year imaging.
Conclusion
Radiological follow-up of patients operated on with mastoid and epitympanic obliteration using BG granules is effective using both HRCT and MRI. A cholesteatoma and/or other potential complications could easily be detected due to the specific radiological appearance of the BG granules.
Key Points
• The appearance of mastoid and epitympanic obliteration by S53P4 bioactive glass (BG) granules on high-resolution computed tomography (HRCT) scans was homogeneous with an attenuation significantly higher than the attenuation of cholesteatoma and lower than mastoid bone attenuation.
• The granules have a low-intensity signal on non-echo-planar diffusion-weighted sequences and on T2-weighted images and present contrast enhancement allowing the differential diagnosis with cholesteatoma and effective for the detection of other underlying temporal bone pathologies.
• The volume and radiological appearance of the obliteration appear to be stable with time.




Similar content being viewed by others
Abbreviations
- BG:
-
Bioactive glass
- CWD:
-
Canal-wall-down
- CWU:
-
Canal-wall-up
- HRCT:
-
High-resolution computed tomography
References
Robinson JM (1997) Cholesteatoma: skin in the wrong place. J R Soc Med 90:93–96
Mosher H (1911) A method of filling the excavated mastoid with a flap from the back of the auricle. Laryngoscope 21:1158–1163
Palva T (1973) Operative technique in mastoid obliteration. Acta Otolaryngol 75:289–290
Shea MC Jr, Gardner G Jr, Simpson ME (1972) Mastoid obliteration with bone. Otolaryngol Clin North Am 5:161–172
Irving RM, Gray RF, Moffat DA (1994) Bone pâté obliteration or revision mastoidectomy: a five-symptom comparative study. Clin Otolaryngol Allied Sci 19:158–160
Decher H (1985) Reduction of radical cavities by homologous cartilage chips. Laryngol Rhinol Otol (Stuttg) 64:423–426
Montandon P, Benchaou M, Guyot JP (1995) Modified canal wall-up mastoidectomy with mastoid obliteration for severe chronic otitis media. ORL J Otorhinolaryngol Relat Spec 57:198–201
Yung MW (1996) The use of hydroxyapatite granules in mastoid obliteration. Clin Otolaryngol Allied Sci 21:480–484
Hussain A, Ram B, Hilmi OJ (2002) Reconstruction of mastoid cavity with hydroxyapatite cement and postauricular flap. Laryngoscope 112:583–585
Bagot D’Arc M, Daculsi G (2003) Micro macroporous biphasic ceramics and fibrin sealant as a moldable material for bone reconstruction in chronic otitis media surgery. A 15 years experience. J Mater Sci Mater Med 14:229–233
Bernardeschi D, Nguyen Y, Mosnier I, et al (2014) Use of granules of biphasic ceramic in rehabilitation of canal wall down mastoidectomy. Eur Arch Otorhinolaryngol 271:59–64
Zhang D, Leppäranta O, Munukka E et al (2010) Antibacterial effects and dissolution behavior of six bioactive glasses. J Biomed Mater Res A 93:475–483
van Gestel NAP, Geurts J, Hulsen DJW et al (2015) Clinical applications of S53P4 bioactive glass in bone healing and osteomyelitic treatment: a literature review. Biomed Res Int 2015:684826
Stoor P, Pulkkinen J, Grénman R (2010) Bioactive glass S53P4 in the filling of cavities in the mastoid cell area in surgery for chronic otitis media. Ann Otol Rhinol Laryngol 119:377–382
Silvola JT (2012) Mastoidectomy cavity obliteration with bioactive glass: a pilot study. Otolaryngol Head Neck Surg 147:119–126
Sarin J, Grénman R, Aitasalo K et al (2012) Bioactive glass S53P4 in mastoid obliteration surgery for chronic otitis media and cerebrospinal fluid leakage. Ann Otol Rhinol Laryngol 121:563–569
Bernardeschi D, Nguyen Y, Russo FY et al (2015) Cutaneous and labyrinthine tolerance of bioactive glass S53P4 in mastoid and epitympanic obliteration surgery: prospective clinical study. Biomed Res Int 2015:242319
Bernardeschi D, Pyatigorskaya N, Russo FY et al (2017) Anatomical, functional and quality-of-life results for mastoid and epitympanic obliteration with bioactive glass s53p4: a prospective clinical study. Clin Otolaryngol 42:387–396
de Veij Mestdagh PD, Colnot DR, Borggreven PA et al (2017) Mastoid obliteration with S53P4 bioactive glass in cholesteatoma surgery. Acta Otolaryngol 137:690–694
De Foer B, Vercruysse J-P, Pilet B et al (2006) Single-shot, turbo spin-echo, diffusion-weighted imaging versus spin-echo-planar, diffusion-weighted imaging in the detection of acquired middle ear cholesteatoma. AJNR Am J Neuroradiol 27:1480–1482
De Foer B, Vercruysse J-P, Bernaerts A et al (2010) Middle ear cholesteatoma: non-echo-planar diffusion-weighted MR imaging versus delayed gadolinium-enhanced T1-weighted MR imaging--value in detection. Radiology 255:866–872
von Elm E, Altman DG, Egger M et al (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808
Samy RN, Shoman NM, Cornelius RS, Pensak ML (2010) Radiologic comparison of density of mastoid obliteration vs. cortical bone and otic capsule. Laryngoscope 120(Suppl 4):S219
Lindfors NC, Hyvönen P, Nyyssönen M et al (2010) Bioactive glass S53P4 as bone graft substitute in treatment of osteomyelitis. Bone 47:212–218
Lindfors NC, Koski I, Heikkilä JT et al (2010) A prospective randomized 14-year follow-up study of bioactive glass and autogenous bone as bone graft substitutes in benign bone tumors. J Biomed Mater Res B Appl Biomater 94:157–164
Stoor P, Apajalahti S, Kontio R (2017) Regeneration of cystic bone cavities and bone defects with bioactive glass S53P4 in the upper and lower jaws. J Craniofac Surg 28:1197–1205
Rantakokko J, Frantzén JP, Heinänen J et al (2012) Posterolateral spondylodesis using bioactive glass S53P4 and autogenous bone in instrumented unstable lumbar spine burst fractures. A prospective 10-year follow-up study. Scand J Surg 101:66–71
Peltola M, Suonpää J, Aitasalo K et al (1998) Obliteration of the frontal sinus cavity with bioactive glass. Head Neck 20:315–319
Peltola M, Aitasalo K, Suonpää J et al (2006) Bioactive glass S53P4 in frontal sinus obliteration: a long-term clinical experience. Head Neck 28:834–841
Yung MM, Karia KR (1997) Mastoid obliteration with hydroxyapatite--the value of high resolution CT scanning in detecting recurrent cholesteatoma. Clin Otolaryngol Allied Sci 22:553–557
Vercruysse J-P, De Foer B, Somers T et al (2010) Long-term follow up after bony mastoid and epitympanic obliteration: radiological findings. J Laryngol Otol 124:37–43
Hinohira Y, Gyo K, Yanagihara N et al (1998) Effects of mastoid cavity obliteration on the growth of experimentally produced residual cholesteatoma. Acta Otolaryngol 118:101–104
Munukka E, Leppäranta O, Korkeamäki M et al (2008) Bactericidal effects of bioactive glasses on clinically important aerobic bacteria. J Mater Sci Mater Med 19:27–32
Franco-Vidal V, Daculsi G, Bagot d’Arc M et al (2014) Tolerance and osteointegration of TricOs(TM)/MBCP(®) in association with fibrin sealant in mastoid obliteration after canal wall-down technique for cholesteatoma. Acta Otolaryngol 134:358–365
Vrabec JT (2018) Imaging of labyrinthine fistula after repair with bone pate. Laryngoscope 128(7):1643–1648
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Daniele Bernardeschi.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bernardeschi, D., Law-ye, B., Bielle, F. et al. Bioactive glass granules for mastoid and epitympanic surgical obliteration: CT and MRI appearance. Eur Radiol 29, 5617–5626 (2019). https://doi.org/10.1007/s00330-019-06120-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06120-z