Abstract
Purpose
To assess the effectiveness of implementing a quality improvement project in a clinical cancer network directed at the response assessment of oncology patients according to RECIST-criteria.
Methods
Requests and reports of computed tomography (CT) studies from before (n = 103) and after (n = 112) implementation of interventions were compared. The interventions consisted of: a multidisciplinary working agreement with a clearly described workflow; subspecialisation of radiologists; adaptation of the Picture Archiving and Communication System (PACS); structured reporting.
Results
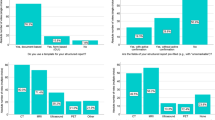
The essential information included in the requests and the reports improved significantly after implementation of the interventions. In the requests, mentioning start date increased from 2% to 49%; date of baseline CT from 7% to 64%; nadir date from 1% to 41%. In the reports, structured layout increased from 14% to 86%; mentioning target lesions from 18% to 80% and non-target lesions from 11% to 80%; measurements stored in PACS increased from 76% to 97%; labelled key images from 38% to 95%; all p values < 0.001.
Conclusion
The combination of implementation of an optimised workflow, subspecialisation and structured reporting led to significantly better quality radiology reporting for oncology patients receiving chemotherapy. The applied multifactorial approach can be used within other radiology subspeciality areas as well.
Key points
• Undeveloped subspecialisation makes adherence to RECIST guidelines difficult in general hospitals.
• A clinical cancer network provides opportunities to improve healthcare.
• Optimised workflow, subspecialisation and structured reporting substantially improve request and report quality.
• Good interdisciplinary communication between oncologists, radiologists and others contributes to quality improvement.

Similar content being viewed by others
Abbreviations
- PACS:
-
Picture Archiving and Communication System
- PDCA:
-
Plan Do Check Act
- RECIST:
-
Response Evaluation Criteria in Solid Tumours
References
Dafny LS, Lee TH (2015) The good merger. N Engl J Med 372:2077–2079
Frakt AB (2015) Hospital consolidation isn’t the key to lowering costs and raising quality. JAMA 313:345
Lindgren EA, Patel MD, Wu Q, Melikian J, Hara AK (2014) The clinical impact of subspecialized radiologist reinterpretation of abdominal imaging studies, with analysis of the types and relative frequency of interpretation discrepancies. Abdom Imaging 39:1119–1126
Bell ME, Patel MD (2014) The degree of abdominal imaging (AI) subspecialization of the reviewing radiologist significantly impacts the number of clinically relevant and incidental discrepancies identified during peer review of emergency after-hours body CT studies. Abdom Imaging 39:1114–1118
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
van Persijn van Meerten EL, Gelderblom H, Bloem JL (2010) RECIST revised: implications for the radiologist. A review article on the modified RECIST guideline. Eur Radiol 20:1456–1467
Nishino M, Jagannathan JP, Ramaiya NH, Van den Abbeele AD (2010) Revised RECIST guideline version 1.1: what oncologists want to know and what radiologists need to know. AJR Am J Roentgenol 195:281–289
Abajian AC, Levy M, Rubin DL (2012) Informatics in radiology: improving clinical work flow through an AIM database: a sample web-based lesion tracking application. Radiographics 32:1543–1552
Jorritsma W, Cnossen F, Dierckx RA, Oudkerk M, van Ooijen PMA (2015) Pattern mining of user interaction logs for a post-deployment usability evaluation of a radiology PACS client. Int J Med Inform. https://doi.org/10.1016/j.ijmedinf.2015.10.007
Folio LR, Nelson CJ, Benjamin M, Ran A, Engelhard G, Bluemke DA (2015) Quantitative radiology reporting in oncology: survey of oncologists and radiologists. AJR Am J Roentgenol 205:W233–W243
Siewert B, Hochman MG (2015) Improving safety through human factors engineering. Radiographics 35:1694–1705
Travis AR, Sevenster M, Ganesh R, Peters JF, Chang PJ (2014) Preferences for structured reporting of measurement data: an institutional survey of medical oncologists, oncology registrars, and radiologists. Acad Radiol 21:785–796
Marcal LP, Fox PS, Evans DB et al (2015) Analysis of free-form radiology dictations for completeness and clarity for pancreatic cancer staging. Abdom Imaging 40:2391–2397
Patel BN, Gupta RT, Zani S, Jeffrey RB, Paulson EK, Nelson RC (2015) How the radiologist can add value in the evaluation of the pre- and post-surgical pancreas. Abdom Imaging. https://doi.org/10.1007/s00261-015-0549-y
Narayan A, Cinelli C, Carrino JA et al (2015) Quality measurements in radiology: a systematic review of the literature and survey of radiology benefit management groups. J Am Coll Radiol 12:1173–1181.e23
Tirkes T, Hollar MA, Tann M, Kohli MD, Akisik F, Sandrasegaran K (2013) Response criteria in oncologic imaging: review of traditional and new criteria. Radiographics 33:1323–1341
Fleishon HB, Itri JN, Boland GW, Duszak R (2016) academic medical centers and community hospitals integration: trends and strategies. J Am Coll Radiol. https://doi.org/10.1016/j.jacr.2016.07.006
Muenzel D, Engels H-P, Bruegel M, Kehl V, Rummeny EJ, Metz S (2012) Intra- and inter-observer variability in measurement of target lesions: implication on response evaluation according to RECIST 1.1. Radiol Oncol 46:8–18
Donnelly LF, Merinbaum DJ, Epelman M et al (2015) Benefits of integration of radiology services across a pediatric health care system with locations in multiple states. Pediatr Radiol 45:736–742
Wilson MA (1983) Improvement in referral practices elicited by a redesigned request format. Radiology 146:677–679
Pham R, Forsberg D, Plecha D (2017) Improved screening mammogram workflow by maximizing PACS streamlining capabilities in an academic breast center. J Digit Imaging 30:133–140
Silveira PC, Dunne R, Sainani NI et al (2015) Impact of an information technology-enabled initiative on the quality of prostate multiparametric MRI reports. Acad Radiol 22:827–833
Patel BN, Lopez JM, Jiang BG, Roth CJ, Nelson RC (2016) Image-rich radiology reports: a value-based model to improve clinical workflow. J Am Coll Radiol 14:57–64
Towbin AJ, Perry LA, Larson DB (2017) Improving efficiency in the radiology department. Pediatr Radiol 47:783–792
Kadom N, Nagy P (2016) Quality improvement and leadership development. J Am Coll Radiol 13:182–183
Kelly AM, Cronin P (2015) Practical approaches to quality improvement for radiologists. Radiographics 35:1630–1642
Acknowledgements
The authors thank the administrative staff, the technicians, the PACS administrators, the radiologists and the oncologists for participating in the project.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is P.M.A. van Ooijen MSc PhD.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was not required for this study because patient data were anonymously used for the study and no interventions took place for the study.
Ethical approval
Institutional Review Board approval was not required because of the retrospective nature of the study.
Methodology
• retrospective
• observational
• performed at one institution
Rights and permissions
About this article
Cite this article
Olthof, A.W., Borstlap, J., Roeloffzen, W.W. et al. Improvement of radiology reporting in a clinical cancer network: impact of an optimised multidisciplinary workflow. Eur Radiol 28, 4274–4280 (2018). https://doi.org/10.1007/s00330-018-5427-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5427-x