Abstract
Objective
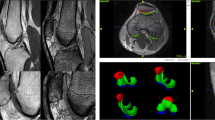
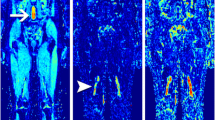
To evaluate intra-tumour and striated muscle T1 value heterogeneity and the influence of different methods of T1 estimation on the variability of quantitative perfusion parameters.
Material and methods
Eighty-two patients with a histologically confirmed musculoskeletal tumour were prospectively included in this study and, with ethics committee approval, underwent contrast-enhanced MR perfusion and T1 mapping. T1 value variations in viable tumour areas and in normal-appearing striated muscle were assessed. In 20 cases, normal muscle perfusion parameters were calculated using three different methods: signal based and gadolinium concentration based on fixed and variable T1 values.
Results
Tumour and normal muscle T1 values were significantly different (p = 0.0008). T1 value heterogeneity was higher in tumours than in normal muscle (variation of 19.8% versus 13%). The T1 estimation method had a considerable influence on the variability of perfusion parameters. Fixed T1 values yielded higher coefficients of variation than variable T1 values (mean 109.6 ± 41.8% and 58.3 ± 14.1% respectively). Area under the curve was the least variable parameter (36%).
Conclusion
T1 values in musculoskeletal tumours are significantly different and more heterogeneous than normal muscle. Patient-specific T1 estimation is needed for direct inter-patient comparison of perfusion parameters.
Key Points
• T1 value variation in musculoskeletal tumours is considerable.
• T1 values in muscle and tumours are significantly different.
• Patient-specific T1 estimation is needed for comparison of inter-patient perfusion parameters.
• Technical variation is higher in permeability than semiquantitative perfusion parameters.




Similar content being viewed by others
Abbreviations
- ROI:
-
region of interest
- T1:
-
time to 63% longitudinal magnetisation recovery
- FSE:
-
weighted fast spin-echo
- NEX:
-
number of excitations
- FOV:
-
field of view
- HPF:
-
high power field
- SPGR:
-
spoiled gradient-echo
- AIF:
-
arterial input function
- ICC:
-
intraclass correlation coefficients
- CV:
-
coefficient of variation
- EES:
-
extravascular extracellular space
- SER :
-
signal enhancement ratio
- AUC :
-
area under the curve
- Max slope:
-
maximum slope of increase
- Ktrans :
-
transfer constant from the plasma to the extravascular extracellular space
- kep :
-
backflux constant
- Vp :
-
plasma volume
- Ve :
-
extravascular extracellular space volume
- PVNS:
-
pigmented villonodular synovitis
- GCT:
-
giant cell tumour
Bibliography
Fisher SM, Joodi R, Madhuranthakam AJ et al (2016) Current utilities of imaging in grading musculoskeletal soft tissue sarcomas. Eur J Radiol 85:1336–1344
Fayad LM, Jacobs MA, Wang X et al (2012) Musculoskeletal tumours: how to use anatomic, functional, and metabolic MR techniques. Radiology 265:340–356
Griffith JF, Yeung DKW, Leung JCS et al (2011) Prediction of bone loss in elderly female subjects by MR perfusion imaging and spectroscopy. Eur Radiol 21:1160–1169
Teixeira PAG, Chanson A, Beaumont M et al (2013) Dynamic MR imaging of osteoid osteomas: correlation of semiquantitative and quantitative perfusion parameters with patient symptoms and treatment outcome. Eur Radiol 23:2602–2611
Heye T, Davenport MS, Horvath JJ et al (2013) Reproducibility of dynamic contrast-enhanced MR imaging Part I. Perfusion characteristics in the female pelvis by using multiple computer-aided diagnosis perfusion analysis solutions. Radiology 266:801–811
Beuzit L, Eliat P-A, Brun V et al (2015) Dynamic contrast-enhanced MRI: Study of inter-software accuracy and reproducibility using simulated and clinical data. J Magn Reson Imaging. doi:10.1002/jmri.25101
Cheng H-LM, Stikov N, Ghugre NR, Wright GA (2012) Practical medical applications of quantitative MR relaxometry. J Magn Reson Imaging 36:805–824
Ivanidze J, Kallas ON, Gupta A et al (2016) Application of blood–brain barrier permeability imaging in global cerebral edema. AJNR Am J Neuroradiol. doi:10.3174/ajnr.A4784
Brix G, Semmler W, Port R et al (1991) Pharmacokinetic parameters in CNS Gd-DTPA enhanced MR imaging. J Comput Assist Tomogr 15:621–628
Hittmair K, Gomiscek G, Langenberger K et al (1994) Method for the quantitative assessment of contrast agent uptake in dynamic contrast-enhanced MRI. Magn Reson Med 31:567–571
Aronhime S, Calcagno C, Jajamovich G et al (2014) DCE-MRI of the liver: effect of linear and non linear conversions on hepatic perfusion quantification and reproducibility. J Magn Reson Imaging 40:90–98
Stikov N, Boudreau M, Levesque IR et al (2015) On the accuracy of T1 mapping: searching for common ground. Magn Reson Med 73:514–522
Piechnik SK, Ferreira VM, Lewandowski AJ et al (2013) Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson 15:13
Pineda FD, Medved M, Fan X, Karczmar GS (2016) B1 and T1 mapping of the breast with a reference tissue method. Magn Reson Med 75:1565–1573
O’Connor JPB, Rose CJ, Waterton JC et al (2015) Imaging intratumor heterogeneity: role in therapy response, resistance, and clinical outcome. Clin Cancer Res 21:249–257
Trojani M, Contesso G, Coindre JM et al (1984) Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int J Cancer 33:37–42
Abdul-Karim FW, Bauer TW, Kilpatrick SE et al (2004) Recommendations for the reporting of bone tumors. Association of Directors of Anatomic and Surgical Pathology. Hum Pathol 35:1173–1178
Tofts PS, Brix G, Buckley DL et al (1999) Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: standardized quantities and symbols. J Magn Reson Imaging 10:223–232
Dyke JP, Panicek DM, Healey JH et al (2003) Osteogenic and Ewing sarcomas: estimation of necrotic fraction during induction chemotherapy with dynamic contrast-enhanced MR imaging. Radiology 228:271–278
Leach MO, Brindle KM, Evelhoch JL et al (2005) The assessment of antiangiogenic and antivascular therapies in early-stage clinical trials using magnetic resonance imaging: issues and recommendations. Br J Cancer 92:1599–1610
Schoierer O, Bloess K, Bender D et al (2014) Dynamic contrast-enhanced magnetic resonance imaging can assess vascularity within fracture non-unions and predicts good outcome. Eur Radiol 24:449–459
Gondim Teixeira PA, Gay F, Chen B et al (2016) Diffusion-weighted magnetic resonance imaging for the initial characterization of non-fatty soft tissue tumors: correlation between T2 signal intensity and ADC values. Skelet Radiol 45:263–271
Crawley AP, Henkelman RM (1988) A comparison of one-shot and recovery methods in T1 imaging. Magn Reson Med 7:23–34
Cheng H-LM, Wright GA (2006) Rapid high-resolution T(1) mapping by variable flip angles: accurate and precise measurements in the presence of radiofrequency field inhomogeneity. Magn Reson Med 55:566–574
Hawighorst H, Libicher M, Knopp MV et al (1999) Evaluation of angiogenesis and perfusion of bone marrow lesions: role of semiquantitative and quantitative dynamic MRI. J Magn Reson Imaging 10:286–294
Ganeshan B, Miles KA, Babikir S et al (2016) CT-based texture analysis potentially provides prognostic information complementary to interim FDG-PET for patients with Hodgkin’s and aggressive non-Hodgkin’s lymphomas. Eur Radiol. doi:10.1007/s00330-016-4470-8
Giganti F, Antunes S, Salerno A et al (2016) Gastric cancer: texture analysis from multidetector computed tomography as a potential preoperative prognostic biomarker. Eur Radiol. doi:10.1007/s00330-016-4540-y
Sidhu HS, Benigno S, Ganeshan B et al (2016) Textural analysis of multiparametric MRI detects transition zone prostate cancer. Eur Radiol. doi:10.1007/s00330-016-4579-9
Kim JH, Ko ES, Lim Y, et al. (2016) Breast cancer heterogeneity: MR imaging texture analysis and survival outcomes. Radiology 160261. doi: 10.1148/radiol.2016160261
Foroutan P, Kreahling JM, Morse DL et al (2013) Diffusion MRI and novel texture analysis in osteosarcoma xenotransplants predicts response to anti-checkpoint therapy. PLoS ONE 8, e82875. doi:10.1371/journal.pone.0082875
Verma RK, Slotboom J, Locher C et al (2016) Characterization of enhancing MS lesions by dynamic texture parameter analysis of dynamic susceptibility perfusion imaging. Biomed Res Int 2016:9578139
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Alain Blum.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
This study has received funding by the Société française de radiologie (SFR) and the Collège des enseignants de Radiologie de France (CERF).
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• observational
• performed at one institution
Rights and permissions
About this article
Cite this article
Gondim Teixeira, P., Leplat, C., Chen, B. et al. Contrast-enhanced 3T MR Perfusion of Musculoskeletal Tumours: T1 Value Heterogeneity Assessment and Evaluation of the Influence of T1 Estimation Methods on Quantitative Parameters. Eur Radiol 27, 4903–4912 (2017). https://doi.org/10.1007/s00330-017-4891-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4891-z