Abstract
Purpose
We assessed the burden of waiting for surveillance CT colonography (CTC) performed in patients having 6–9 mm colorectal polyps on primary screening CTC. Additionally, we compared the burden of primary and surveillance CTC.
Materials and methods
In an invitational population-based CTC screening trial, 101 persons were diagnosed with <3 polyps 6–9 mm, for which surveillance CTC after 3 years was advised. Validated questionnaires regarding expected and perceived burden (5-point Likert scales) were completed before and after index and surveillance CTC, also including items on burden of waiting for surveillance CTC. McNemar’s test was used for comparison after dichotomization.
Results
Seventy-eight (77 %) of 101 invitees underwent surveillance CTC, of which 66 (85 %) completed the expected and 62 (79 %) the perceived burden questionnaire. The majority of participants (73 %) reported the experience of waiting for surveillance CTC as ‘never’ or ‘only sometimes’ burdensome. There was almost no difference in expected and perceived burden between surveillance and index CTC. Waiting for the results after the procedure was significantly more burdensome for surveillance CTC than for index CTC (23 vs. 8 %; p = 0.012).
Conclusion
Waiting for surveillance CTC after primary CTC screening caused little or no burden for surveillance participants. In general, the burden of surveillance and index CTC were comparable.
Key points
• Waiting for surveillance CTC within a CRC screening caused little burden
• The vast majority never or only sometimes thought about their polyp(s)
• In general, the burden of index and surveillance CTC were comparable
• Awaiting results was more burdensome for surveillance than for index CTC
Similar content being viewed by others
Introduction
Debate remains regarding the management of individuals with 6–9 mm polyps at screening, and an option is surveillance CT colonography, because of the low malignancy risk and slow growing rate of these polyps [1–4]. Successful surveillance with CT colonography is amongst other factors dependent on patients’ adherence, which is likely related to previous experiences with CT colonography and expectations toward the surveillance examination. Furthermore, screening for colorectal cancer (CRC) may cause relevant side effects, such as discomfort, anxiety, and distress. In particular, waiting for a follow-up examination with the idea of having a lesion that may progress to cancer, and waiting for the results of the surveillance examination may cause considerable negative psychological consequences. The consequences of awaiting surveillance CT colonography are currently unknown and have to be weighed against CT colonography benefits [5]. Further, one can speculate about potential differences in experience between first and second CT colonography, as patients should know better what to expect the second time.
In this prospective study, we evaluated the burden of waiting 3 years for the procedure and the results of a surveillance CT colonography in patients having one or two small (6–9 mm) polyps on primary screening CT colonography. We also assessed the burden, pain, and embarrassment of surveillance CT colonography in comparison to index CT colonography in our previously performed, randomized, population-based screening trial [6].
Materials and methods
Study design and participants
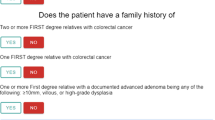
We enrolled asymptomatic 50–75 year adults with no prior or family history of CRC or adenomatous polyps, who underwent CT colonography in the context of an invitational population-based screening program (COCOS trial) [7, 8]. Eligible patients had one or two 6–9 mm polyps that were prospectively identified on screening CT colonography, and were advised to undergo surveillance CT colonography after 3 years. At that time, management after surveillance CT colonography was not clear.
Ethics approval from the Dutch Health Council (2009/03WBO, The Hague, the Netherlands) was obtained for the COCOS trial, in which the surveillance CT colonography was included. Patients had already given their written informed consent to be contacted for follow-up studies and consented to this study.
Invitation
Invitations for surveillance CT colonography were sent by mail and patients were asked to contact one of the researchers by phone. In the case of no response, a reminder letter was sent after 4 weeks and if no response to the reminder letter was received, the person was contacted by phone once after another 4 weeks. Patients who underwent a CT colonography or colonoscopy in the time between the index CT colonography and the advised surveillance CT colonography were excluded. Study information was sent to all included patients willing to participate. Non-participation reasons were summarized [9].
Procedure
CT colonography preparation, colonic distention, and scan protocol were identical to the index CT colonography examination (see for detailed description Appendix I). Briefly, patients underwent a non-cathartic preparation the day before the examination and 1.5 hours prior to the examination (total of 3x50 mL of iodinated contrast agent; Telebrix Gastro, Guerbet, Aulnaysous-Bois, France) in combination with a low-fibre diet for 1 day [10, 11]. Before colonic insufflation, 20 mg intravenous hyoscine butylbromide (Buscopan; Boehringer-Ingelheim, Ingelheim, Germany) was administered, after which colonic distention was achieved with automated pressure-controlled carbon dioxide insufflation (PROTOCO2L, Bracco, EZEM, Lake Success, NY, USA) through a thin, flexible rectal tube. When distension was considered sufficient via the scout image, a breath-hold supine and prone CT was performed using a 64 multi-detector-row CT scanner (Brilliance, Philips Healthcare, Best, the Netherlands; SOMATOM Sensation, Siemens Medical Solutions, Erlangen, Germany). Patients received no sedation or analgesics. Expert readers evaluated all CT colonographies within 2 weeks after the procedure. Patients were informed by phone about the results within 2 weeks after the surveillance CT colonography. Colonoscopy was done if a lesion ≥6 mm was reported.
Questionnaires
The expected burden questionnaire (EBQ) and perceived burden questionnaire (PBQ) were identical to those used in index CT colonography and are based on previous Dutch faecal occult blood test (FOBT) screening pilots, and on studies investigating the acceptance of CT colonography and patient perception of diagnostic tests for faecal incontinence [12–15]. For all included EBQs and PBQs we retrieved the corresponding EBQs and PBQs of index CT colonography, and the questions for index and surveillance CT colonography were compared.
Expected burden questionnaire (EBQ)
A pre-procedural questionnaire was sent to the participants to assess the expectations towards the CT colonography within 4 weeks before the procedure. They were asked to complete the questionnaire prior to the screening procedure and to return it by mail in a prepaid envelope (which was identical for index CT colonography). The EBQ contained items regarding expected embarrassment, pain, and burden of the bowel preparation and the examination itself. All but two items were scored on 5-point Likert scales (1 = not at all; 2 = slightly; 3 = some; 4 = rather; 5 = extremely) [16]. Two items regarding thoughts in the past 3 years were scored on 4-point Likert scales (1 = never; 2 = sometimes; 3 = regularly; 4 = often). Expected burden questionnaires completed after surveillance CT colonography were excluded from analysis.
Perceived burden questionnaire (PBQ)
The perceived burden, pain, and embarrassment of CT colonography and different procedural aspects were assessed using a post-procedural questionnaire, sent by mail after the participants had been informed about the CT colonography result. The PBQ contained items regarding the perceived embarrassment, pain, and burden of the bowel preparation, the examination itself, and the overall burden of the CT colonography examination (same 5-point Likert scale as pre-procedural [16]). We also collected information on the willingness to return for future screening rounds. PBQs that were completed after 12 weeks from the surveillance CT colonography were excluded from analysis, as we considered this time interval too long for an accurate representation of the perceived burden (for index CT colonography, this was 6 weeks)
Surveillance-specific questions
In addition to the EBQ for the index CT colonography, items regarding the burden and fear of waiting for (the results of) surveillance CT colonography were included. All but two items were scored on 5-point Likert scales. Two items regarding thoughts in the past 3 years were scored on 4-point Likert scales (1 = never; 2 = sometimes; 3 = regularly; 4 = often). The PBQ included additional items on the most burdensome aspect of the surveillance CT colonography (waiting for surveillance CT colonography, preparation, examination, abdominal symptoms afterward, or waiting for the results) and of the entire CT colonography screening procedure ((results of) index or surveillance CT colonography).
Impact of event scale (IES)
The level of colorectal cancer (CRC)-specific distress was assessed using the Impact of Event Scale (IES) sent together with the EBQ (IES-I) and PBQ (IES-II) [17–19]. The 15 IES items were tailored to the specific “event”: “a diagnosis of colorectal cancer”. All items were scored on 4-point Likert scales measuring whether this was present (0 = not at all; 1 = rarely; 3 = sometimes; 5 = often) during the past 7 days. The summary score of the total scale could range from 0 to 75, with a higher score indicating more cancer-specific distress (0–8: no meaningful impact; 9–25: impact event; 26–43 powerful impact event; 44–75 severe impact event). The IES was found to be sufficiently reliable (Cronbach α for IES-I and IES-II was 0.87 and 0.89, respectively) to allow these analyses to be performed.
Statistical analysis
Demographics and items specific for surveillance CT colonography were described. Corresponding questions on EBQs and PBQs were compared between index and surveillance CT colonography, and only paired data were used. Answers to questions with 4-point and 5-point ordinal scales were first dichotomized (totally agree/agree versus disagree/totally disagree and not at all/slightly versus some/rather/extremely) and differences were assessed using the McNemar test for paired proportions. One question regarding expectations towards surveillance CT colonography required a different dichotomization because of different response categories (better/slightly better/as expected versus slightly worse/worse than expected). We used Mann-Whitney U tests to test the significance of differences in the mean IES scores by sex and surveillance CT colonography results. To test for differences in IES over time, paired Wilcoxon signed-rank tests were conducted. A p-value of <0.05 was considered significant. To determine the clinical relevance of the significant difference between means, we used the minimal important difference (MID), which is defined as half of a standard deviation. SPSS V.20.0 for Windows (SPSS, Chicago, Ill) was used to perform all statistical tests.
Results
Response and respondent characteristics
Between July 2012 and May 2014, 101 patients were invited to undergo surveillance CT colonography (Fig. 1). Twenty-three (23 %) of the 101 invitees were excluded for surveillance CT colonography (four passed away; ten underwent a colonoscopy examination prior to the invitation of the surveillance CT colonography, of which five were at the patient’s own request (Appendix II); nine did not wish to participate, the most common reason mentioned was other health problems).
Overview of response to the expected and perceived burden questionnaire (EBQ and PBQ) including Impact of Event Scale (IES) among 101 surveillance CT colonography participants. aFour passed away, ten underwent a colonoscopy prior to invitation for surveillance CT colonography, and nine did not wish to participate for various reasons. bCompleted the EBQ & IES-I and PBQ & IES-II in time (prior to the surveillance CT colonography and within 12 weeks of surveillance CT colonography, respectively)
Seventy-eight patients (77 %) underwent a surveillance CT colonography (median age 63.5 IQR [60.0–72.0]; 53 % male) at a mean surveillance interval of 3.3 years (SD 0.3; range 3.0–4.6 years) (Table 1). The EBQ was completed in time by 66 (85 %) surveillance participants, the IES-I in 65 (83 %) participants. The PBQ and IES-II were returned within 12 weeks of surveillance CT colonography by 62 patients (79 %). Sixty-four EBQs and 48 PBQs of index and surveillance CT colonography were available for a head-to-head comparison.
Waiting for the surveillance CT colonography
The vast majority of the respondents never or only sometimes thought about the colonic polyp(s) (89 %; 57/64) or the recommended surveillance CT colonography (84 %; 54/64) (Fig. 2). Thoughts about the presence of the colonic polyp(s) or the waiting for surveillance CT colonography were for the majority of participants not at all or only slightly burdensome (75 %; 47/63 and 73 %; 46/63, respectively). Waiting for surveillance CT colonography did not result in anxiety or slight anxiety in 86 % (54/63). The vast majority expected the waiting for the results to be not at all or only slightly burdensome (70 %; 45/64) or expected to be not at all or only slightly anxious (72 %; 46/64) while waiting for the results of surveillance CT colonography.
Expected burden in comparison to index CT colonography
Expected burden for surveillance CT colonography was rated similarly as for index CT colonography, with the exception that the bowel preparation was expected to be not or only slightly embarrassing by a larger proportion of participants for surveillance CT than for index CT (87 %; 55/63 versus 71 %; 45/63, respectively; p = 0.031) (Fig. 3). The proportion of participants who thought that the evaluation of extracolonic structures on CT colonography was advantageous was larger in surveillance than in index CT colonography (98 %; 63/64 versus 89 %; 57/64; p = 0.031) (Appendix III).
Perceived burden in comparison to index CT colonography
Items on perceived burden of bowel preparation, CT colonography examination, abdominal complaints in the weeks of the examination, and the entire screening procedure were rated comparably for index CT colonography, with the CT colonography examination itself cited as the most burdensome part and insufflation of CO2 as the most burdensome/painful part of the CT examination (Appendix IV). Two items differed: waiting for the results was considered some, rather, or extremely burdensome by 23 % (11/47) in surveillance CT colonography versus 6 % (3/47) of participants in index CT colonography (p = 0.021) (Fig. 4). The surveillance CT colonography was experienced as expected by 31 % (15/48) and worse than expected by 6 (3/48), versus 15 % (7/48) and 23 % (11/48), respectively, in index CT colonography (p = 0.011).
Evaluation of entire screening procedure
The most burdensome part of the surveillance CT colonography procedure was considered to be the CT examination itself (33 %; 16/48) followed by bowel complaints (25 %; 12/48) and waiting for the results (25 %; 12/48). For index CT colonography, the bowel preparation was indicated as the most burdensome part (35 %; 17/48), followed by the examination itself (29 %; 14/48) and the bowel complaints (25 %; 12/48). Waiting 3 years for surveillance CT colonography was indicated as the most burdensome part by only 8 % (4/48) of invitees. There was no significant difference between surveillance and index CT colonography for the proportion of participants who would recommend CT colonography in screening (96 %; 46/48 versus 98 %; 47/48; p = 1.000) and who would participate in future screening rounds (98 %; 46/47 versus 94 %; 44/47; p = 0.625).
Psychological distress
Fifty-five paired IES scores were available for analysis. The total IES scores were significantly higher for women than for men prior to and after surveillance CT colonography (9.4 (SD 9.8) and 3.6 (SD 5.3); p = 0.006 and 11.9 (SD 11.9) and 4.3 (SD 4.7); p = 0.012, respectively) (Fig. 5a). Differences were larger than the MID and therefore considered to be clinically relevant.
CRC-specific distress score (Impact of Event Scale [IES] total) over time. a Total IES scores for the total group, separated by gender. Total IES scores in women were significantly higher than for men prior to and after surveillance CT colonography (p = 0.006 and p = 0.012, respectively). b Total IES scores for the total group, separated by result of the surveillance CT colonography. Total IES score of the group with a positive CT colonography result increased (p = 0.006). Total IES scores of the group with a negative result decreased (p = 0.655)
The total IES score of the group of patients with a positive CT colonography result significantly increased over time (from 5.2 SD (6.6) to 8.2 (SD 10.1); p = 0.006) (Fig. 5b). The difference was smaller than the MID and therefore not considered to be clinically relevant.
Discussion
This study demonstrated that the knowledge of having a 6–9 mm colonic polyp, and subsequently, being under surveillance caused little or no burden. It furthermore showed that waiting for surveillance CT colonography in screening for CRC caused little to no anxiety or burden in the vast majority of participants. In general, expectations towards and perceived burden of surveillance CT colonography were similar to index CT colonography 3 years before. Having to wait for the CT colonography results after the surveillance CT colonography was the only factor considered significantly more burdensome than for index CT colonography (23 versus 8 %). Surveillance CT colonography turned out to be worse than expected compared to index CT colonography far less often, in 6 versus 23 % of patients, respectively. Surveillance for CRC with CT colonography appeared to have no major impact on most patients; however, women did experience significantly more distress than men. The large majority of participants would recommend participating in CT colonography for CRC screening (96 %) and would participate again in the future (98 %).
To the best of our knowledge, our study is the first to evaluate the burden of waiting for surveillance CT colonography in patients with one or two 6–9 mm polyps detected at primary screening CT colonography. Our study design with identical questionnaires made a head-to-head comparison between expected and perceived burden of index and surveillance CT colonography possible. Both questionnaires had been validated in previous CRC screening pilots.
Patients did not seem to worry too much about the possible presence of colonic polyp(s), or did not find the knowledge of having this/these polyp(s) burdensome, which also can be concluded from the small fraction of patients (8 %) who considered waiting for surveillance CT colonography the most burdensome aspect of the entire screening procedure. One must realize that our study population does not represent a random selected group of persons. Individuals chose to participate in the initial CRC screening trial and, in exchange for being informed about their health, accepted certain consequences—for example, (the burden of) surveillance CT colonography. In addition, ten excluded patients underwent a preliminary colonoscopy, of which five were at their own request. In these patients, it seems likely that anxiety or worry was a barrier for waiting 3 years for surveillance CT colonography and that they were probably more prone to psychological stress.
In addition to the selection bias described noted above, a number of other potential limitations should be acknowledged. The surveillance population originated from a primary screening trial (COCOS trial), which was powered for comparing the participation rate and yield of CT colonography versus colonoscopy screening and not for evaluating burden in surveillance CT colonography, therefore leading to a relatively small surveillance population [10]. In addition, we only used paired data for solid comparison analyses, resulting in the exclusion of more questionnaires. Because of those limited number of patients, we chose a relatively wide interval (12 weeks) in which the PBQ could be returned, to retain as many questionnaires for analyses as possible. This possibly could have affected patients’ evaluations. An assessment of PBQ and cancer-specific distress (IES) before receiving the results of surveillance CT colonography might have showed higher burden scores and/or distress, as waiting for the results was reported as burdensome in 25 %. Also, an extra assessment later in time (after the results of the colonoscopy) could have provided us with information about the duration of higher distress experienced by certain patients [20]. Because of the associated questions (e.g. three questions on bowel preparation, for pain, burden, and embarrassment), there is a chance of eventually finding a significant difference on one question/outcome, as was probably the case with the expected embarrassment about bowel preparation given the comparable expectations on all other items.
Waiting for the results of a (screening) study is burdensome [5]. The significantly higher proportion of patients that consider waiting for the results of surveillance CT colonography to be somewhat, rather, or extremely burdensome in comparison to index CT colonography (23 versus 8 %) is most likely related to the knowledge of having a colonic polyp that may have grown. However, the waiting time for the results of the surveillance CT colonography in our study was unusually long (2 weeks), as the CT was evaluated by multiple observers within the framework of a different study. In daily practice, the wait will be shorter and this might decrease the burden. At colonoscopy, patients are directly informed about the results, which is very much appreciated by patients [6].
The significantly larger proportion of patients reporting surveillance CT colonography to be better than or as expected compared to index CT colonography (94 versus 77 %) was in accordance with our hypothesis that patients previously had underestimated certain elements of index CT colonography [6]. As the study information and guidance during the CT colonography was identical to index CT colonography, the more realistic expectations are most likely due to previous experience with CT colonography. This was, however, not accompanied by a higher expected or lower perceived burden in surveillance CT colonography. The CT colonography examination itself was identified as the most burdensome part of the entire screening procedure when participants were forced to choose one aspect alone, and in line with previous studies, the colonic insufflation with CO2 was considered the most burdensome and painful part of CT colonography [6, 21]. Although analgesia has shown to reduce total procedural pain and burden in CT colonography [22], this use of it remains a matter of practical hurdles, side effects, and costs.
The Impact of Event Scale (IES) has been used in the psycho-oncology literature as a measure of cancer-related anxiety, amongst other types in screening populations [5, 23, 24]. Although we noticed a significant increase in the total IES score in patients with a positive result, we did not notice any clinically relevant changes in cancer-specific distress, which was in accordance with other screening studies [5, 23]. The higher distress scores in women than in men were also reported in other studies [5, 25, 26]. This should be considered when supplying information and providing counselling for CRC screening.
In conclusion, waiting for surveillance CT colonography caused little discomfort. In general, the expected and perceived burden of surveillance and index CT colonography were comparable. Since waiting for the results for surveillance CT colonography proved to be burdensome, minimizing the waiting time for the test result is recommended. It is also reassuring that after surveillance CT colonography, almost every patient would participate again in future screening rounds.
References
Lieberman D, Moravec M, Holub J, Michaels L, Eisen G (2008) Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology 135:1100–1105
Kim DH, Pickhardt PJ, Taylor AJ et al (2007) CT colonography versus colonoscopy for the detection of advanced neoplasia. N Engl J Med 357:1403–1412
Spada C, Stoker J, Alarcon O et al (2015) Clinical indications for computed tomographic colonography: european society of gastrointestinal endoscopy (ESGE) and european society of gastrointestinal and abdominal radiology (ESGAR) guideline. Eur Radiol 25:331–345
Tutein Nolthenius CJ, Boellaard TN, de Haan MC et al (2015) Computer tomography colonography participation and yield in patients under surveillance for 6-9 mm polyps in a population-based screening trial. Eur Radiol
van den Bergh KA, Essink-Bot ML, Bunge EM et al (2008) Impact of computed tomography screening for lung cancer on participants in a randomized controlled trial (NELSON trial). Cancer 113:396–404
de Wijkerslooth TR, de Haan MC, Stoop EM et al (2012) Burden of colonoscopy compared to non-cathartic CT-colonography in a colorectal cancer screening programme: randomised controlled trial. Gut 61:1552–1559
de Haan MC, Nio CY, Thomeer M et al (2012) Comparing the diagnostic yields of technologists and radiologists in an invitational colorectal cancer screening program performed with CT colonography. Radiology 264:771–778
de Wijkerslooth TR, de Haan MC, Stoop EM et al (2010) Study protocol: population screening for colorectal cancer by colonoscopy or CT colonography: a randomized controlled trial. BMC Gastroenterol 10:47
van Rijn AF, van Rossum LG, Deutekom M et al (2008) Low priority main reason not to participate in a colorectal cancer screening program with a faecal occult blood test. J Public Health (Oxf) 30:461–465
Stoop EM, de Haan MC, de Wijkerslooth TR et al (2012) Participation and yield of colonoscopy versus non-cathartic CT colonography in population-based screening for colorectal cancer: a randomised controlled trial. Lancet Oncol 13:55–64
Liedenbaum MH, Denters MJ, Zijta FM et al (2011) Reducing the oral contrast dose in CT colonography: evaluation of faecal tagging quality and patient acceptance. Clin Radiol 66:30–37
Denters MJ, Deutekom M, Fockens P, Bossuyt PMM, Dekker E (2009) Implementation of population screening for colorectal cancer by repeated fecal occult blood test in the Netherlands. Bmc Gastroenterol 9
van Gelder RE, Birnie E, Florie J et al (2004) CT colonography and colonoscopy: assessment of patient preference in a 5-week follow-up study. Radiology 233:328–337
Deutekom M, Terra MP, Dijkgraaf MGW et al (2006) Patients’ perception of tests in the assessment of faecal incontinence. Br J Radiol 79:94–100
Hol L, van Leerdam ME, van Ballegooijen M et al (2010) Screening for colorectal cancer: randomised trial comparing guaiac-based and immunochemical faecal occult blood testing and flexible sigmoidoscopy. Gut 59:62–68
Likert R (1932) A technique for the measurement of attitudes. York, New
van der Ploeg E, Mooren TT, Kleber RJ, van der Velden PG, Brom D (2004) Construct validation of the Dutch version of the impact of event scale. Psychol Assess 16:16–26
Horowitz M, Wilner N, Alvarez W (1979) Impact of Event Scale: a measure of subjective stress. Psychosom Med 41:209–218
Brom D, Kleber RJ (1985) De Schok Verwerkings Lijst [The Dutch version of the Impact of Event Scale]. Ned Tijdschr Psychol 40:164–168
Lowe JB, Balanda KP, Del Mar C, Hawes E (1999) Psychologic distress in women with abnormal findings in mass mammography screening. Cancer 85:1114–1118
Jensch S, Bipat S, Peringa J et al (2010) CT colonography with limited bowel preparation: prospective assessment of patient experience and preference in comparison to optical colonoscopy with cathartic bowel preparation. Eur Radiol 20:146–156
Boellaard TN, van der Paardt MP, Hollmann MW et al (2013) A multi-centre randomised double-blind placebo-controlled trial to evaluate the value of a single bolus intravenous alfentanil in CT colonography. BMC Gastroenterol 13:94
Cullen J, Schwartz MD, Lawrence WF, Selby JV, Mandelblatt JS (2004) Short-term impact of cancer prevention and screening activities on quality of life. J Clin Oncol 22:943–952
Taylor KL, Shelby R, Gelmann E, McGuire C (2004) Quality of life and trial adherence among participants in the prostate, lung, colorectal, and ovarian cancer screening trial. J Natl Cancer Inst 96:1083–1094
Kruijshaar ME, Kerkhof M, Siersema PD et al (2006) The burden of upper gastrointestinal endoscopy in patients with Barrett's esophagus. Endoscopy 38:873–878
Thiis-Evensen E, Wilhelmsen I, Hoff GS, Blomhoff S, Sauar J (1999) The psychologic effect of attending a screening program for colorectal polyps. Scand J Gastroenterol 34:103–109
Acknowledgments
The scientific guarantor of this publication is J. Stoker, MD, PhD. This study was funded by the Dutch Cancer Society (KWF Kanker Bestrijding 2012–5698). Philips Healthcare (Best, the Netherlands) provided the CT colonography workstations. Neither were involved in designing or conducting this study, had access to the data, or were involved in data analysis or preparation of this manuscript. One author (J Stoker) of this manuscript declares relationships with the following companies: Robarts. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study.
Some study subjects or cohorts have been previously reported in: de Wijkerslooth et al. Gut 2012 ‘Burden of colonoscopy compared to non-cathartic CT-colonography in a colorectal cancer screening programme: randomised controlled trial. Methodology: prospective, cross sectional study, multicenter study.
We thank research nurses Isha Verkaik and Laurens Groenendijk for their research support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Appendices
Appendix I
Detailed description of CT colonography procedure
A non-cathartic preparation consisting of two 50-mL doses of iodinated contrast agent (Telebrix Gastro, Guerbet, Aulnaysous-Bois, France) was given on the day before the examination, and another 50 mL was given 1.5 hours prior to the examination (total = 150 mL) in combination with a low-fibre diet for 1 day [8, 9].
All CT colonography examinations were performed by experienced radiologic technologists. Both supine- and prone-position CT images were obtained on two 64-slice CT-scanners (Brilliance, Philips Healthcare, Best, the Netherlands; SOMATOM Sensation, Siemens Medical Solutions, Erlangen, Germany) using a low-dose protocol; with collimation 64 × 0.625 mm, slice thickness 0.9 mm, reconstruction interval 0.7 mm, tube voltage 120 kV, and 25 reference mAs (for Brilliance) and collimation 128 × 0.6 mm, slice thickness 1.0 mm, reconstruction interval 0.7 mm, tube voltage 120 kV, and 16 ref mAs (for SOMATOM Sensation). Before colonic insufflation, 20 mg intravenous hyoscine butylbromide was administered (if contraindicated, 1 mg of glucagon hydrochloride was used intravenously). Distention of the colon was obtained via a thin, flexible rectal catheter using automatic insufflation of carbon dioxide (PROTOCO2L, Bracco, EZEM, Lake Success, NY, USA).
All CT colonographies were evaluated within 2 weeks after the procedure by an experienced abdominal radiologist using primary 2D (window setting 1500, -250 HU) with 3D problem solving (Amsterdam: View Forum, Philips, Best, the Netherlands), and by two of four trained technologists (experience of all four = approximately ±1200 CT colonographies), read using primary 2D and followed by 3D [5]. All readers finished with computer-aided detection (CAD) evaluation. Patients were informed about the results within 2 weeks of the CT colonography. Colonoscopy was done if at least one of the observers reported a lesion ≥6 mm.
Appendix II
Reasons for early surveillance CT colonography or colonoscopy instead of the advised surveillance CT colonography at 3 years
Appendix III
General statements on bowel cancer screening in index and surveillance CT colonography. P-values of McNemar’s test after dichotomization are presented on top of the bars
Appendix IV
Perceived burden of bowel preparation and different aspects of surveillance CT colonography in comparison to index CT colonography. P-values of McNemar’s test after dichotomization are presented on top of the bars
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Tutein Nolthenius, C.J., Boellaard, T.N., de Haan, M.C. et al. Burden of waiting for surveillance CT colonography in patients with screen-detected 6–9 mm polyps. Eur Radiol 26, 4000–4010 (2016). https://doi.org/10.1007/s00330-016-4251-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4251-4