Abstract
Objective
To investigate pathological findings in the susceptibility weighted imaging (SWI) of patients experiencing convulsive (CSE) or non-convulsive status epilepticus (NCSE) with focal hyperperfusion in the acute setting.
Methods
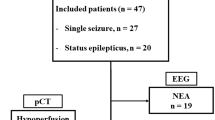
Twelve patients (six with NCSE confirmed by electroencephalogram (EEG) and six patients with CSE with seizure event clinically diagnosed) underwent MRI in this acute setting (mean time between onset of symptoms and MRI was 3 h 8 min), including SWI, dynamic susceptibility contrast MR imaging (DSC) and diffusion-weighted imaging (DWI). MRI sequences were retrospectively evaluated and compared with EEG findings (10/12 patients), and clinical symptoms.
Results
Twelve out of 12 (100 %) patients showed a focal parenchymal area with pseudo-narrowed cortical veins on SWI, associated with focal hyperperfused areas (increased cerebral blood flow (CBF) and mean transit time (MTT) shortening), and cortical DWI restriction in 6/12 patients (50 %). Additionally, these areas were associated with ictal or postical EEG patterns in 8/10 patients (80 %). Most frequent acute clinical findings were aphasia and/or hemiparesis in eight patients, and all of them showed pseudo-narrowed veins in those parenchymal areas responsible for these symptoms.
Conclusion
In this study series with CSE and NCSE patients, SWI showed focally pseudo-narrowed cortical veins in hyperperfused and ictal parenchymal areas. Therefore, SWI might have the potential to identify an ictal region in CSE/NCSE.
Key Points
• The focal ictal brain regions show hyperperfusion in DSC MR-perfusion imaging.
• SWI shows focally diminished cortical veins in hyperperfused ictal regions.
• SWI has the potential to identify a focal ictal region in CSE/NCSE.



Similar content being viewed by others
References
Meierkord H, Holtkamp M (2007) Non-convulsive status epilepticus in adults: clinical forms and treatment. Lancet Neurol 6:329–339
Leppik IE (1993) Status epilepticus in the treatment of epilepsy: principles and practice. Lee and Febiger, Philadelphia
Shneker BF, Fountain NB (2003) Assessment of acute morbidity and mortality in nonconvulsive status epilepticus. Neurology 61:1066–1073
Maganti R, Gerber P, Drees C, Chung S (2008) Nonconvulsive status epilepticus. Epilepsy Behav 12:572–586
Foreman B, Hirsch LJ (2012) Epilepsy emergencies: diagnosis and management. Neurol Clin 30:11–41, vii
El-Koussy M, Mathis J, Lovblad KO, Stepper F, Kiefer C, Schroth G (2002) Focal status epilepticus: follow-up by perfusion- and diffusion MRI. Eur Radiol 12:568–574
Toledo M, Munuera J, Sueiras M, Rovira R, Alvarez-Sabin J, Rovira A (2008) MRI findings in aphasic status epilepticus. Epilepsia 49:1465–1469
Hauf M, Slotboom J, Nirkko A, von Bredow F, Ozdoba C, Wiest R (2009) Cortical regional hyperperfusion in nonconvulsive status epilepticus measured by dynamic brain perfusion CT. AJNR Am J Neuroradiol 30:693–698
Masterson K, Vargas MI, Delavelle J (2009) Postictal deficit mimicking stroke: role of perfusion CT. J Neuroradiol 36:48–51
Szabo K, Poepel A, Pohlmann-Eden B et al (2005) Diffusion-weighted and perfusion MRI demonstrates parenchymal changes in complex partial status epilepticus. Brain 128:1369–1376
Hauf M, Wiest R, Schindler K et al (2013) Common mechanisms of auditory hallucinations-perfusion studies in epilepsy. Psychiatry Res 211:268–270
Canas N, Breia P, Soares P et al (2010) The electroclinical-imagiological spectrum and long-term outcome of transient periictal MRI abnormalities. Epilepsy Res 91:240–252
Hong KS, Cho YJ, Lee SK, Jeong SW, Kim WK, Oh EJ (2004) Diffusion changes suggesting predominant vasogenic oedema during partial status epilepticus. Seizure 13:317–321
Fahrendorf D, Schwindt W, Wolfer J et al (2013) Benefits of contrast-enhanced SWI in patients with glioblastoma multiforme. Eur Radiol 23:2868–2879
Gramsch C, Goricke SL, Behrens F et al (2013) Isolated cerebral susceptibility artefacts in patients with malignant melanoma: metastasis or not? Eur Radiol 23:2622–2627
Mittal S, Wu Z, Neelavalli J, Haacke EM (2009) Susceptibility-weighted imaging: technical aspects and clinical applications, part 2. AJNR Am J Neuroradiol 30:232–252
Santhosh K, Kesavadas C, Thomas B, Gupta AK, Thamburaj K, Kapilamoorthy TR (2009) Susceptibility weighted imaging: a new tool in magnetic resonance imaging of stroke. Clin Radiol 64:74–83
Hermier M, Nighoghossian N (2004) Contribution of susceptibility-weighted imaging to acute stroke assessment. Stroke 35:1989–1994
Saini J, Kesavadas C, Thomas B et al (2009) Susceptibility weighted imaging in the diagnostic evaluation of patients with intractable epilepsy. Epilepsia 50:1462–1473
Kao HW, Tsai FY, Hasso AN (2012) Predicting stroke evolution: comparison of susceptibility-weighted MR imaging with MR perfusion. Eur Radiol 22:1397–1403
Huang P, Chen CH, Lin WC, Lin RT, Khor GT, Liu CK (2012) Clinical applications of susceptibility weighted imaging in patients with major stroke. J Neurol 259:1426–1432
Verschuuren S, Poretti A, Buerki S, Lequin MH, Huisman TA (2012) Susceptibility-weighted imaging of the pediatric brain. AJR Am J Roentgenol 198:W440–W449
Bosemani T, Burton VJ, Felling RJ et al (2013) Pediatric hemiplegic migraine: role of multiple MRI techniques in evaluation of reversible hypoperfusion. Cephalalgia. doi:10.1177/0333102413509432
Lee YJ, Shon YM, Yoo WJ, Jung SL, Kim BS, Ahn KJ (2013) Diminished visibility of cerebral venous vasculature in subclinical status epilepticus by susceptibility-weighted imaging: a case report. Clin Neuroradiol. doi:10.1007/s00062-013-0204-3
Zhao M, Suh M, Ma H, Perry C, Geneslaw A, Schwartz TH (2007) Focal increases in perfusion and decreases in hemoglobin oxygenation precede seizure onset in spontaneous human epilepsy. Epilepsia 48:2059–2067
Wasterlain CG, Fujikawa DG, Penix L, Sankar R (1993) Pathophysiological mechanisms of brain damage from status epilepticus. Epilepsia 34:S37–S53
Unrath A, Muller HP, Ludolph AC, Kassubek J (2012) Reversible cortical diffusion restriction, hyperperfusion and T2-hyperintensity caused by two different types of epileptic seizure. Clin Neuroradiol 22:239–243
Xing W, Wang X, Xie F, Liao W (2013) Application of dynamic susceptibility contrast-enhanced perfusion in temporal lobe epilepsy. Acta Radiol 54:107–112
Ge Y, Zohrabian VM, Osa EO et al (2009) Diminished visibility of cerebral venous vasculature in multiple sclerosis by susceptibility-weighted imaging at 3.0 Tesla. J Magn Reson Imaging 29:1190–1194
Tsui YK, Tsai FY, Hasso AN, Greensite F, Nguyen BV (2009) Susceptibility-weighted imaging for differential diagnosis of cerebral vascular pathology: a pictorial review. J Neurol Sci 287:7–16
Thomas B, Somasundaram S, Thamburaj K et al (2008) Clinical applications of susceptibility weighted MR imaging of the brain - a pictorial review. Neuroradiology 50:105–116
Tong KA, Ashwal S, Obenaus A, Nickerson JP, Kido D, Haacke EM (2008) Susceptibility-weighted MR imaging: a review of clinical applications in children. AJNR Am J Neuroradiol 29:9–17
Gelfand JM, Wintermark M, Josephson SA (2010) Cerebral perfusion-CT patterns following seizure. Eur J Neurol 17:594–601
Iwasaki H, Takeda T, Ito T et al (2014) The use of susceptibility-weighted imaging for epileptic focus localization in acute-stage pediatric encephalopathy: a case report. Pediatr Neurol 50:171–176
Bosemani T, Verschuuren SI, Poretti A, Huisman TA (2013) Pitfalls in susceptibility-weighted imaging of the pediatric brain. J Neuroimaging. doi:10.1111/jon.12051
Acknowledgements
The scientific guarantor of this publication is Dr. Rajeev Kumar Verma. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was not required for this study because of the retrospective design of the study. Methodology: retrospective, cross-sectional study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aellen, J., Abela, E., Buerki, S.E. et al. Focal hemodynamic patterns of status epilepticus detected by susceptibility weighted imaging (SWI). Eur Radiol 24, 2980–2988 (2014). https://doi.org/10.1007/s00330-014-3284-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3284-9