Abstract
This cross-sectional study aims to evaluate the post-traumatic growth (PTG) level and explores its predictors among adult patients with SLE in China. From April 2020 to April 2021, 135 hospitalized adult SLE patients completed the questionnaire including sociodemographic and disease-related data, Post-traumatic Growth Inventory (PTGI), Medical Coping Modes Questionnaire (MCMQ), Social Support Rating Scale (SSRS), Pittsburgh Sleep Quality Index (PSQI), Hospital Anxiety and Depression Scale (HADS), and Self-Perceived Burden Scale (SPBS). Descriptive analysis, pearson’s correlation analysis, and forward multiple line regression analysis were used for analysis by SPSS 22.0. Results showed that, the mean PTGI score was 57.52 ± 20.82. Pearson correlation analysis showed that, complicated autoimmune hemolytic anemia (r = − 0.185), CD4 +/CD8 + (r = − 0.383), acceptance-resignation (r = − 0.185), poor PSQI (r = − 0.215), and depression (r = − 0.322) were negatively associated with total PTGI score; while the relationship with lupus nephritis (r = 0.247), confrontation (r = 0.313), avoidance (r = 0.379), and SSRS (r = 0.242) were positive (all P < 0.05). The total score of PTGI and its five sub-dimensions were not correlated with anxiety and self-perceived burden. Further, CD4 +/CD8 +, confrontation of MCMQ, and SSRS could explain 30.3% of the variance in total PTGI (F = 6.646, P < 0.01). In summary, Chinese adults with SLE experience moderate levels of PTG. Clinical nurses need pay attention to the current disease status and individual characteristics of patients, as well as their mental health, to promote their growth experience, so that they can cope with the future life in a better state and coexist well with SLE.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease of unknown etiology, characterized by the involvement of multiple organs, such as skin, joints, kidneys, lungs, central nervous system, and hematopoietic system, and linked to the production of autoantibodies leading to inflammation [1, 2]. SLE occurs commonly in women of child-bearing age (approximately 9:1 female to male) [3], with the prevalence ranging from 0 to 241/100,000 people [4]. In China, it generally affects 38.6 in every 100,000 individuals. Emerging data show that the prevalence of SLE is rising over time, and now SLE is one of the leading causes of death in young women [5]. Conventional therapies include oral glucocorticoids, antimalarial and/or immunosuppressive therapies to control inflammation [6].
While remission is an achievable outcome, it may seldom be reached or sustained with the current therapies [1]. It has been reported that the clinical response rate and complete response rate of SLE patients in China were only 3.2% and 2.8%, respectively [7]. This implies that disease burden with SLE remains high and patients often experiencing significant work disability due to the need for repeated treatment [6]. Thus, being diagnosed with SLE can be a traumatic experience for patients. It has been reported that those negative changes, such as anxiety (72%), depression (70%), and ensuing challenges in sleeping (79%), were commonly observed in SLE patients [8]. However, at the same time, a growing body of evidence has documented positive post-traumatic changes known as post-traumatic growth (PTG).
PTG refers to positive psychological change experienced as a result of the struggle with highly challenging life circumstances [9]. Previous research indicates that more perceived growth in the months or years following negative life events may be associated with long-term health outcomes, such as decreased morbidity, mortality, and psychological distress [10]. Thus, it is necessary to understand person’s PTG level. Empirical evidence has demonstrated that PTG can be observed among patients with rheumatoid arthritis and multiple sclerosis, two kinds of autoimmune disease [11]. This means that patients with autoimmune disease may experience varying levels of PTG. Given that exploring PTG is consistent with the salutogenic approach that calls for a positive orientation toward health, rather than a focus on the origins of disease, in seeking to promote and maintain physical and mental well-being [12], it is of great significance to evaluate PTG level in patients with SLE, one of the most common autoimmune disease. Nonetheless, PTG in SLE has received little attention. The only study related to PTG in lupus was conducted in 2001 by Katz et al. [13] in USA. They compared the differences of PTG between 56 cancer patients and 31 lupus patients in US, found that lupus patients were more demoralized and reported fewer benefits from their illness than cancer patients. It is important to note that this study included patients with lupus. Considering that lupus has four categories, namely SLE, cutaneous lupus, drug-induced lupus, and neonatal lupus; PTG of SLE patients cannot be accurately extracted. In addition, after 20 years of rapid development of medical technology, it is unknown whether the PTG of SLE patients in today’s era has changed, as well as its level among Chinese patients.
Therefore, this study aims to evaluate the PTG level and explore its predictors among patients with SLE. Hope this study play a key role in promoting the possibility of PTG in SLE patients.
Methods
Participants
In this cross-sectional study, patients hospitalized in Department of Rheumatology, The First Affiliated Hospital of Soochow University in China from April 2020 to April 2021, fulfilled the 1997 American College of Rheumatology revised criteria for the classification of SLE [14], and willing to participate in were selected as the research objects. Patients who were < 18 years old, diagnosed with severe mental or life-threatening disorders were excluded from this research. This survey was approved by the Medical Ethics Committee of The First Affiliated hospital of Soochow University (2021023), on March 1st, 2021, and written informed consent statement were obtained from each participant.
Demographics and clinical characteristics
Demographic variables contained the following: age, gender, body mass index (BMI), education, occupation, monthly income, place of residence, marital status, number of children, smoking, drinking, and medical insurance.
Clinical variables included comorbidity, disease duration, number of hospitalizations, and blood examination. Venous blood of 3 ml was collected from all patients in the morning under fasting condition. Centrifugation at 3000 R/min for 10 min. The upper layer of serum was stored at – 80 °C. Factor B, IgG, IgA, IgM, complement 3 and 4, Kappa- and Lambda-light chain were detected by nephelometry immunoassay. Additionally, anticoagulant whole blood was incubated with CD3-FITC, CD4-PC7, CD8-APC-Cy7 fluorescent antibodies at 4 °C for 30 min. Then, lysate red blood cells with potassium chloride buffer, wash, fix for flow cytometry.
Clinical measurements
Post-traumatic Growth (PTG) was measured by the 20-item Chinese Version of Post-traumatic Growth Inventory (C-PTGI) [15], which was adapted from the Post-traumatic Growth Inventory [16]. C-PTGI comprised of the following five subscales: relating to others (RO), new possibilities (NP), personal strength (PS), spiritual change (SC), and appreciation for life (AL). Each item was answered on a 6-point Likert scale from 0 (strongly disagree)-5 (strongly agree), with total scores ranging from 0 to 100 and high scores indicating high PTG.
Coping strategy was measured by Medical Coping Modes Questionnaire (MCMQ), which was originally invented by Feifel [17], and the Chinese version was revised by Shen et al. [18]. The MCMQ Chinese version consists of 20 items, covering three dimensions: confrontation (8 items), avoidance (7 items), and acceptance-resignation (5 items). All the items were rated on a 4-point Likert scale ranging from 1 (never) to 4 (very often). The score for each coping strategy was calculated separately, and higher scores indicate that individuals are more inclined to use that coping strategy.
Social support was determined by the Social Support Rating Scale (SSRS), which was developed for the Chinese population by Xiao in 1994 [19]. The scale includes 10 items that measure 3 dimensions: subjective support (4 items), objective support (3 items), and support utilization (3 items). The total score ranges from 12 to 66. A higher score represents more social support.
Sleep quality was evaluated by Pittsburgh Sleep Quality Index (PSQI), which is a self-rated questionnaire developed by Buysse et al. [20] in 1989. PSQI consists of 19 items in 7 dimensions: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The total score ranges from 0 to 21, and the scores > 5 were defined as poor sleep quality.
Anxiety and depression were measured by Hospital Anxiety and Depression Scale (HADS), which was developed by Zigmond et al. [21], and translated by Leung et al. [22]. This scale contains 14 items, with seven items assessing depression and seven items assessing anxiety on a 4-point Likert scale. Total score of either subscale is ranging from 0 to 21. Patients with a score ≥ 8, on either subscale, was considered to have clinically significant anxiety or depression.
Self-perceived burden (SPB) was measured by Self-Perceived Burden Scale (SPBS), which was developed by Cousineau et al. in 2003 [23], and translated by Wu et al. [24]. This scale consists of 10 items, including three dimensions of body burden, emotional burden, and economic burden. Each item is scored on a five-point Likert scale, from 1 (never) to 5 (always). Total SPBS score is defined as the sum of the individual items (the eighth item is scored in reverse), and higher scores indicate heavier burden.
Data analysis
Statistical analysis was performed using SPSS 21.0. Categorical variables will be described by frequency (percentage). For continuous variables, Kolmogorov–Smirnov test was used to conduct normality assessment, with P > 0.05 indicating normal distribution. Continuous variables with normal distribution will be described by mean ± standard deviation (SD), others will be described by median (Min–Max). The relationship between variables and PTGI, the five sub-dimensions of PTGI were first tested by pearson correlation analysis. Then, variables with a significant association with PTGI and the five sub-dimensions were entered into a forward stepwise multivariate linear regression model to test the significant predictors of PTGI, as well as the five sub-dimensions of PTGI, respectively, with the criteria that included if P < 0.05 or removed if P > 0.10. The statistically significant level was 0.05, two-tailed.
Results
Descriptive statistics
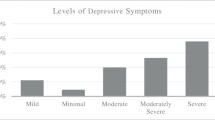
The descriptive statistics for all study variables are shown in Table 1. Of the 137 participants, the response rate was 100%, and 135 eligible patients were included in the final analysis (2 were less than 18 years old). The mean age was 39.13 ± 13.30. Female accounted for 94.1%. Lupus nephritis (LN) was present in 36.3% of 135 adult SLE patients, idiopathic thrombocytopenic purpura (ITP) in 14.8%. 59.3% of patients reported poor sleep quality. The prevalence of anxiety and depression among the 135 adult SLE patients was 41.5% and 36.3%, respectively. The SSRS score was 38.87 ± 6.70, and the SPB was 30.20 ± 7.69.
The total PTGI score was 57.52 ± 20.82, for the 5 dimensions, RO was 8.87 ± 3.75, NP was 10.27 ± 5.20, PS was 9.47 ± 3.73, SC was 9.61 ± 4.43, AL was 19.29 ± 6.93 (Fig. 1). This suggests that adult SLE patients have moderate level of PTG.
Correlation between PTGI and variables
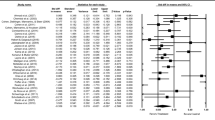
Table 1 also displayed the relationship between PTGI and variables. Pearson correlation analysis showed that, complicated AIHA (r = − 0.185, P < 0.05), CD4 + /CD8 + (r = − 0.383, P < 0.05), acceptance-resignation (r = − 0.185, P < 0.05), poor PSQI (r = − 0.215, P < 0.05), and depression (r = − 0.322, P < 0.01) were negatively associated with total PTGI score; while the relationship with complicated LN (r = 0.247, P < 0.01), confrontation (r = 0.313, P < 0.01), avoidance (r = 0.379, P < 0.01), and SSRS (r = 0.242, P < 0.01) was positive. The total score of PTGI and its five sub-dimensions were not correlated with anxiety and self-perceived burden (P > 0.05).
Predictors of PTGI
The forward multiple line regression analysis revealed that CD4 + /CD8 +, confrontation, and SSRS could explain 30.3% of the variance in total PTGI (F = 6.646, P < 0.01). For the dimensions of PTGI, BMI, Factor B level, avoidance, and SSRS could explain 22.1% of the variance in RO (F = 8.993, P < 0.01); complicated LN, marital status, confrontation, avoidance, and acceptance-resignation could explain 24.6% of the variance in NP (F = 9.733, P < 0.01); CD3 +, CD4 +/CD8 + , and PSQI could explain 27.8% of the variance in PS (F = 6.013, P < 0.01); drinking, kappa-light chain, CD4 +/CD8 + , and confrontation could explain 41.5% of the variance in SC (F = 7.920, P < 0.01); monthly income, CD4 +/CD8 + , and SSRS could explain 27.5% of the variance in AL (F = 5.815, P < 0.01) (Table 2).
Discussion
This study explored PTG among Chinese adult patients with SLE, and found that, while patients underwent negative induced emotion, such as depression (36.3%) and anxiety (41.5%), they also experienced moderate levels of PTG (57.52 ± 20.82). This was less than that of patients with inflammatory bowel disease (61.36 ± 26.91) [12], another autoimmune disease, but higher than that in Chinese coronary artery disease patients (36.8 ± 21.6) [25], a kind of chronic disease. This indicates that among patients with chronic disease, the PTG of adult SLE patients is at a moderate level. Pearson correlation analysis showed that, complicated AIHA, complicated LN, coping strategy, poor sleep quality, depression, social support, and the level of CD4 +/CD8 + were associated with PTG in adult SLE patients. Further forward multiple line regression analysis retained confrontation of coping strategy, CD4 +/CD8 + ratio, and social support. To our knowledge, this research was the first to investigate PTG and its predictors among adult SLE patients in China.
The exploration of risk and protective factors for PTG in adult patients with SLE yielded significant findings. That there is association between coping strategy and PTG among Chinese adult patients diagnosed with SLE. In details, confrontation and avoidance were positively predictive of PTG, while acceptance-resignation being the negatively predictive. The findings were consistent with earlier study focus on other chronic disease [26]. Feifel et al. [17] argue that confrontation is generally considered a positive and beneficial coping strategy, and that greater use of confrontation is characteristic of those who perceive their illness as serious. This is also reported by Du et al. [27], that positive coping strategies can relieve stress, promote communication, and have a significant effect by improving mental status and healthy behaviors. Another explanation is that confrontation can help patients adapt more effectively to changes in stress and return to stable health more quickly, and may enhance resilience by influencing feelings of self-efficacy and hope, creating a sense of peace and meaning [28], and thus promote PTG among adult patients diagnosed with SLE. It is very interesting that avoidance is the protective factor of PTG. The possible explanation is that short-term avoidance protects their spiritual world, helps them face the truth of events, facilitates psychological adjustment and increases the likelihood of promoting positive change [26]. Additionally, acceptance-resignation was found to be the negatively predictive of PTG among adult SLE patients. Patients who use accept-resignation as the coping strategy might believe that their illness cannot be resolved, and when confronting it, they are unable to take any action, with an increased feeling of helplessness [29]. Another possible explanation is that acceptance-resignation might put patients in a negative mood in the long run, affect their initiative [30], thus reduce their positive psychological changes-PTG. Therefore, it is suggested that medical staff strengthen the psychological guidance of adult SLE patients and guide them to adopt positive coping styles to enhance PTG.
And one of the things that we found in particular, the CD4 +/CD8 + ratio was the negatively predictive of SLE among adult patients with SLE in China (β = − 11.376, Standard Error = 3.733, P = 0.004). Immunologically, the main potential pathogenesis of SLE is the destruction of tolerance of T and B lymphocytes and the production of large amounts of autoantibodies by self-reactive B cells [31]. Among them, T cells play an indispensable role in promoting the occurrence and development of SLE. T cells can be divided into two subpopulations of CD4 + T cells and CD8 + T cells according to the expression levels of CD4 and CD8 surface molecules [31]. An overactive immune response in SLE induces an inverted t-lymphocyte ratio. Increased T lymphocyte activation can lead to cell depletion and show some characteristics of CD4 +/CD8 + ratio inversion [32]. Under normal physiological conditions, the CD4/CD8 ratio is higher than 1, while 0.91 ± 0.68 in this study. The possible reason is that all the adult SLE patients included in this study were hospitalized with a long course of disease (6.79 ± 7.43 years). Hospitalization means that most patients were in the active stage of disease with abnormal indicators. Long-term coexisting with SLE made them relatively adaptable to those abnormal. For them, the purpose of hospitalization is to relieve symptoms and control the disease, to achieve better survival and positive psychological experience. Therefore, when the CD4 +/CD8 + ratio increases or even reaches the normal value, patients still need to be hospitalized, which may cause negative emotions, such as “Why do I still feel uncomfortable and need to be hospitalized even when this index is normal?”, which in turn weakens the positive effect, such as PTG. This suggests that when clinical staff focus on hospitalized SLE patients with abnormal indicators, they should also pay attention to the psychological state of patients with normal indicators.
We also found social support was positively related to the level of PTG in Chinese adults with SLE (r = 0.242, P < 0.01), although not significantly in the regression analysis. Social support is affected by culture, socioeconomic factors, and policies and impacts health through health behavioral pathways or psychological pathways [33]. It has been empirically demonstrated that social support plays an important role in the transition from trauma to growth, because it activates the cognitive processes that promote PTG [34]. In the case of Chinese adults with SLE, possessing a supportive environment, having the opportunity to self-disclose and receiving help may be especially valuable. Different from western culture, which attaches great importance to individual value and forms the principle of “individual standard”, China advocates group culture and attaches great importance to human social value, forming the principle of “obligation standard”. In addition, China’s group culture has given rise to the group principle, which enforces individual obligations and responsibilities. As a result, China has formed the custom of helping each other when they meet problems, and family members, relatives and friends are relatively close to each other. Therefore, it is necessary to focus on establishing a good social support network. Given the view of positive correlation with RO and AL, two dimensions of PTG, it is necessary to pay attention to the establishment and maintenance of a good social support network, to help activate and promote the cognitive process of PTG in Chinese adult SLE patients.
The limitations of this study are as follows: (1) Single center and small sample have certain impact on the representativeness of the results. However, considering that the data were collected in the first year of COVID-19 in China, and the number of hospitalized patients was strictly controlled at that time, this study to some extent reflects the psychological status of hospitalized SLE patients under the epidemic situation. (2) Due to cross-sectional study design, causality cannot be proved. Since there are no published studies related to PTG in SLE patients in China, it is necessary to use a cross-sectional design to understand the existing status. Future longitudinal studies could be carried out to explore causal links. (3) Subjective measurement tools were used for PTG, coping style, social support, anxiety, depression, sleep quality and self-perceived burden.
Conclusion
Chinese adults with SLE experience moderate levels of PTG. Confrontation of coping strategy and CD4 + /CD8 + were the predictors of PTG. Clinical nurses are thus suggested to pay attention to the current disease status and individual characteristics of patients, as well as their mental health, to promote their growth experience, so that they can cope with the future life in a better state and coexist well with SLE.
Data availability
All data generated or analyzed during this study are available from the corresponding author upon reasonable request.
References
Gerosa M, Beretta L, Ramirez GA et al (2022) Long-Term clinical outcome in systemic lupus erythematosus patients followed for more than 20 years: the Milan systemic lupus erythematosus consortium (SMiLE) cohort. J Clin Med 11(13):3587. https://doi.org/10.3390/jcm11133587
Sang N, Gao R, Zhang M, Wu Z, Wu Z, Wu G (2022) Causal relationship between sleep traits and risk of systemic lupus erythematosus: a two-sample Mendelian randomization study. Front Immunol. https://doi.org/10.3389/fimmu.2022.918749
Hardy C, Gladman DD, Su J, Rozenbojm N, Urowitz MB (2021) Barriers to medication adherence and degree of nonadherence in a systemic lupus erythematosus (SLE) outpatient population. Rheumatol Int. https://doi.org/10.1007/s00296-021-04898-0
Rees F, Doherty M, Grainge MJ, Lanyon P, Zhang W (2017) The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies. Rheumatology 56(11):1945–1961. https://doi.org/10.1093/rheumatology/kex260
Cai M, Gui L, Huang H et al (2022) Proteomic analyses reveal higher levels of neutrophil activation in men than in women with systemic lupus erythematosus. Front Immunol. https://doi.org/10.3389/fimmu.2022.911997
van Vollenhoven RF, Kalunian KC, Dorner T et al (2022) Phase 3, multicentre, randomised, placebo-controlled study evaluating the efficacy and safety of ustekinumab in patients with systemic lupus erythematosus. Ann Rheum Dis. https://doi.org/10.1136/ard-2022-222858
National Clinical Research Center For Skin And Immune Diseases (2020) [China Systemic Lupus Erythematosus Development Report 2019]. http://news.sciencenet.cn/htmlnews/2021/5/457389.shtm
Schneider B (2020) Patient reported impact of lupus on quality of life [abstract]. Arthritis Rheumatol 72(SUPPL 10):2253–2255
Tedeschi RG, Calhoun LG (2004) Posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq 15(1):1–18
Jones DR, Johnson JA, Graham-Engeland JE, Park CL, Smyth JM (2018) Is perceived growth associated with momentary indicators of health and Well-Being in people with asthma or rheumatoid arthritis? Appl Psychol Health Well Being 10(2):254–271. https://doi.org/10.1111/aphw.12129
Barskova T, Oesterreich R (2009) Post-traumatic growth in people living with a serious medical condition and its relations to physical and mental health: a systematic review. Disabil Rehabil 31(21):1709–1733. https://doi.org/10.1080/09638280902738441
Hamama-Raz Y, Nativ S, Hamama L (2021) Post-traumatic growth in inflammatory bowel disease patients: the role of illness cognitions and physical quality of life. J Crohns Colitis 15(6):1060–1067. https://doi.org/10.1093/ecco-jcc/jjaa247
Katz RC, Flasher L, Cacciapaglia H, Nelson S (2001) The psychosocial impact of cancer and lupus: a cross validation study that extends the generality of “benefit-finding” in patients with chronic disease. J Behav Med 24(6):561–571. https://doi.org/10.1023/a:1012939310459
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725. https://doi.org/10.1002/art.1780400928
Wang J (2011) [Development of Posttraumatic Growth Inventory and its norm for accidental injury], Second Military Medical University
Tedeschi RG, Calhoun LG (1996) The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 9(3):455–471. https://doi.org/10.1007/BF02103658
Feifel H, Strack S, Nagy V (1987) Coping strategies and associated features of medically III patients. Psychosom Med 49(6):616–625
Shen X, Jiang Q (2000) Report on application of Chinese version of MCMQ in 701 patients. Chin J Behav Med Sci 9(1):18–20
Xiao S (1994) The theoretical basis and research applications of “Social Support Rating Scale.” J Clin Psychiat 4(2):98–100
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiat Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Zigmond A, Snaith R (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Leung CM, Ho S, Kan CS, Hung CH, Chen CN (1993) Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. A cross-cultural perspective. Int J Psychosom 40(1–4):29–34
Cousineau N, Mcdowell I, Hotz S, Hebert P (2003) Measuring chronic patients’ feelings of being a burden to their caregivers: development and preliminary validation of a scale. Med Care 41(1):110–118. https://doi.org/10.1097/00005650-200301000-00013
Wu Y, Jiang Y (2010) Investigation and analysis of the self-perceived burden among cancer patients. J Nurs Admin 10(06):405–407
Leung YW, Gravely-Witte S, Macpherson A, Irvine J, Stewart DE, Grace SL (2010) Post-traumatic growth among cardiac outpatients. J Health Psychol 15(7):1049–1063. https://doi.org/10.1177/1359105309360577
Zhou L, Hong J, Qin R et al (2021) Post-traumatic growth and its influencing factors among Chinese women diagnosed with gynecological cancer: a cross-sectional study. Eur J Oncol Nurs 51:101903. https://doi.org/10.1016/j.ejon.2021.101903
Du R, Wang P, Ma L, Larcher LM, Wang T, Chen C (2020) Health-related quality of life and associated factors in patients with myocardial infarction after returning to work: a cross-sectional study. Health Qual Life Out. https://doi.org/10.1186/s12955-020-01447-4
Chen S, Mei R, Tan C, Li X, Zhong C, Ye M (2020) Psychological resilience and related influencing factors in postoperative non-small cell lung cancer patients: a cross-sectional study. Psychooncology 29(11):1815–1822. https://doi.org/10.1002/pon.5485
Jurado R, Morales I, Taboada D et al (2011) Coping strategies and quality of life among liver transplantation candidates. Psicothema 23(1):74–79
Qiu X, Zhang K, Zhang Y, Sun L (2022) Benefit finding and related factors of patients with Early-Stage cancer in China. Int J Env Res Pub He 19(7):4284. https://doi.org/10.3390/ijerph19074284
Yuan S, Zeng Y, Li J et al (2022) Phenotypical changes and clinical significance of CD4+ /CD8+T cells in SLE. Lupus Sci Med 9(1):e660. https://doi.org/10.1136/lupus-2022-000660
Handono K, Putra Gofur NR, Nurdiana N et al (2020) Role of lymphocytes CD4/CD8 ratio and immunoglobulin g cytomegalovirus as potential markers for systemic lupus erythematosus patients with periodontal disease. Eur J Dent 14(04):544–550. https://doi.org/10.1055/s-0040-1715788
Aierken A, Ding X, Pan Y, Chen Y, Li Y (2022) Association between dependency on community resources and social support among elderly people living in rural areas in China: a cross-sectional study. BMC Geriatr. https://doi.org/10.1186/s12877-022-03247-5
Sörensen J, Rzeszutek M, Gasik R (2021) Social support and post-traumatic growth among a sample of arthritis patients: analysis in light of conservation of resources theory. Curr Psychol 40(4):2017–2025. https://doi.org/10.1007/s12144-019-0131-9
Acknowledgements
None.
Funding
This study was supported by the National Natural Science Foundation of China (82101893); Suzhou “Kejiaoxingwei” Youth Science and Technology project (KJXW2020004).
Author information
Authors and Affiliations
Contributions
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. RX: Methodology, Formal analysis, Writing—original draft; QY: Acquisition and analysis of data, Writing—original draft; ZX: Acquisition and analysis of data, Writing-review; XL: Interpretation of data; RY: Conceptualization, Validation, Supervision, Writing-editing. All co-authors take full responsibility for the integrity and accuracy of all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interests.
Ethical statement
This survey was approved by the Medical Ethics Committee of The First Affiliated Hospital of Soochow University (2021023).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, R., Yan, Q., Xu, Z. et al. Post-traumatic growth in adult patients with systemic lupus erythematosus: a cross-sectional study in China. Rheumatol Int 43, 1077–1085 (2023). https://doi.org/10.1007/s00296-022-05233-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05233-x