Abstract
Rheumatoid arthritis (RA) is associated with an increased risk of cardiovascular disease (CVD). Advanced measures of cardiorespiratory fitness (CRF) are associated with CVD risk factors. The present study aimed to examine whether CVD risk factors can predict clinic-based measures of CRF, using the Siconolfi step test and to determine if exercise can improve RA patients’ cardiovascular health. Sixty-five RA patients (46 females, age 58 ± 11 years) completed assessments of CRF, CVD risk factors, body composition and RA characteristics. Ten patients participated in a follow-up 8-week exercise intervention. CRF was low (22 ml kg−1 min−1) and associated with higher diastolic blood pressure (r = − 0.37, p = 0.002), higher global CVD risk (r = − 0.267, p = 0.031) and worse body composition profile (body fat, r = − 0.48, p < 0.001; waist, r = − 0.65, p < 0.001; hip, r = − 0.58, p < 0.001). Regular exercise significantly improved CRF (p = 0.021), lower body strength (p < 0.001), agility (p < 0.001), systolic blood pressure (p = 0.021), body fat (p = 0.018), waist circumference (p = 0.035), hip circumference (p = 0.016), disease activity (p = 0.002), disability (p = 0.007) and QoL (p = 0.004). Elevated diastolic blood pressure and worse body composition profile are strong predictors of clinic-based measures of CRF. CRF is an important determinant of CVD risk and warrants inclusion in the routine assessment of RA patients. Regular exercise can improve CRF and CVD risk factors without any exacerbation of disease activity and should be offered as part of routine care.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease that is associated with 50–60% increased mortality risk from cardiovascular disease (CVD) compared to the general population [1]. Excess CVD risk is believed to be dependent on both traditional and novel CVD risk factors such as inflammation [2]. Furthermore, other precipitating factors, such as persistent physical inactivity [3,4,5] and poor cardiorespiratory fitness (CRF) [6, 7] likely contribute.
Typically RA patients have a reduced CRF with reductions of 20–30% being reported by Stenstrom and Minor [8]. Average maximal oxygen consumption (VO2max) values obtained from a group of female RA patients equalled 22 ml kg−1 min−1 [9]. The same poor CRF was observed in a cohort studied by our group [10]. Compared to healthy adults of similar age, RA patients have a significantly reduced CRF [8, 11,12,13]. Unfortunately, in rheumatology clinical practice, the measurement of CRF is generally nonexistent. One reason for this is that a simple method to assess fitness in a clinical setting did not previously exist. However, our group has validated the Siconolfi step test in RA patients [10]. This simple test is a useful tool that can be used by health professionals in routine clinical practice to determine the CRF of their RA patients.
Studies examining the associations between physical activity and traditional CVD risk factors in RA patients reveal that lower physical activity levels are associated with increased systolic blood pressure (SBP), total cholesterol, and low-density lipoprotein [4]. More recently, it has been shown that CRF, as measured by a maximal treadmill test, is also associated with several CVD risk factors [14]. Further, 6 months of individualised exercise can improve CRF, individual CVD risk factors, and reduce overall CVD risk [15]. These studies used advanced measures of CRF which require expensive equipment and technical expertise thus limiting their use in clinical practice. To our knowledge, it is currently unclear if CRF, as assessed by the more simple, clinically applied Siconolfi step test can predict the development of CVD in RA.
Thus, the primary aim of the present study was to examine the association between CRF, as measured by the Siconolfi step test and classical CVD risk factors and RA disease-related factors. A secondary aim was to investigate whether improving CRF via an 8-week group exercise programme offered as part of routine care could also improve RA patients’ cardiovascular health and general wellbeing.
Methods
Participant recruitment
Upon obtaining ethical approval from the North Wales Research Ethics Committee (REC reference: 10/WNo01/11; approved: 22.02.2010), 65 consecutive adults attending rheumatology out-patient services at Betsi Cadwaladr University Health Board (West) were recruited. Patients diagnosed with RA according to the American Rheumatism Association’s 1987 Criteria for the Classification of Rheumatoid Arthritis [16] and who were deemed clinically stable were considered for participation. Exclusion criteria were: pregnancy or breastfeeding, taking beta-blockers, suffering from dementia, neurological impairment, cancer, an unstable chronic or terminal illness or any musculoskeletal impairment that prevented patients completing the step test. With ethical approval (REC reference: 11/WA/0206; approved 04.08.2011), ten RA patients were recruited for an additional longitudinal exercise study. Informed consent was obtained from all participants.
Protocol for cross-sectional study
Participants were assessed in parallel to their rheumatology appointment. On the assessment day, the following measures were assessed in this approximate order:
RA factors
To assess inflammation [erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)] patients were required to have a recent blood test (< 4 weeks). The Stanford Health Assessment Questionnaire (HAQ) [17] and the Disease Activity Score 28 (DAS 28) [18] were used to determine functional status (disability) and disease activity, respectively.
Classical CVD risk factors
Blood pressure was measured following 5 min of rest by the standard auscultatory technique and the values reported are the mean of two measurements. Fasting lipids and glucose were assessed within 4 weeks of the assessment session. Information regarding patients smoking status, family history of heart disease and current medication was obtained using a cardiovascular questionnaire. Global CVD risk was measured using the QRISK2 score [19]. The QRISK2 algorithm includes CVD risk factors such as age, gender, total cholesterol/high-density lipoprotein ratio, blood pressure, diabetes and smoking status but also accounts for the presence of RA.
Body composition
Height and body mass were measured using standard procedures and used to calculate body mass index (BMI) (kg m−2). Body fat was measured using bioelectrical impedance analysis (Tanita corp., Tokyo, Japan) and waist and hip circumference were measured to determine waist–hip ratio (waist:hip).
CRF
CRF was measured using the validated Siconolfi step test [10]. A detailed description of the protocol is provided in the literature [10, 20]. However, in summary, the test involves stepping up and down a 10-inch step in time with a metronome for 3 min per stage for one to three stages. VO2max was estimated from the exercise heart rate at the end of the test according to established equations [20].
Protocol for longitudinal study
RA factors, CVD risk factors, and CRF were measured in the same manner as per the cross-sectional study at baseline and at 8 weeks follow-up. Other assessments included:
Physical function
The 30 s sit-to-stand test requires the participant to stand up and sit down as many times as they can in 30 s and measures lower body strength. The 8-foot “Up and Go” test requires the participant to rise from seated, walk eight feet around a cone and return to a seated position and measures agility, speed and balance whilst moving [21].
Quality of life (QoL) and fatigue
QoL was assessed using the SF-36 health survey [22], a 36-item questionnaire that measures health status on eight different concepts. Health status is categorised into a physical component, a mental component and an overall QoL score. Fatigue was measured using the Multidimensional Assessment of Fatigue (MAF) questionnaire [23], a 16-item scale that measures fatigue according to four dimensions (degree, distress caused, timing, impact on daily living).
Intervention: 8-week exercise programme
In line with ACSM guidelines [24] participants exercised three times per week for 8 weeks at the physiotherapy gym, Gwynedd Hospital. Exercise sessions were supervised by an exercise physiologist. Each session lasted 60 min and consisted of 3 × 10 min aerobic exercises. Participants chose the exercise and order in which they were completed (treadmill, bike, rower, stepper, cross-trainer). Exercise intensity increased from 55 to 85% predicted heart rate max (220-age) during the programme and included both continuous and interval training patterns. Heart rate and ratings of perceived exertion (RPE) were monitored throughout. After aerobic exercise, participants completed resistance training exercises (calf raises, leg raises, knee raises, squats and abdominal curls). Participants completed 15 repetitions × 2 sets of each exercise at week 1 and progressed to 15 repetitions, 10 pulses × 3 sets by week 8.
Statistical analysis
Cross-sectional study
Data analysis was performed using the Statistical Package for Social Sciences version 19.0 (SPSS Inc. Chicago, Illinois, USA). The Kolmogorov–Smirnov test of normality was used to assess the distribution of variables. Variables not normally distributed were log transformed. Non-parametric tests were performed on data that remained not normally distributed (diastolic blood pressure, glucose, ESR, CRP, tender joints, swollen joints, disease duration, HAQ).
Pearson’s correlation coefficient (parametric), Spearman’s correlation coefficient (non-parametric), logistic regression analysis and analysis of covariance (ANCOVA) were performed to assess the association between CRF and CVD risk factors, global CVD risk scores, body composition and RA disease factors. Hierarchical multiple regression was performed to determine the factors (independent variables) which best predict CRF (dependent variable). Statistical significance was set at p < 0.05 for all analyses unless otherwise stated.
Longitudinal study
Dependent t test analysis was used to determine significant differences between pre- and post-test measures. The effect size was calculated using eta squared (t2 ÷ t2 + (N−1)). Significance level was set at p < 0.05 for all analyses.
Results
Cross-sectional study
Descriptive statistics
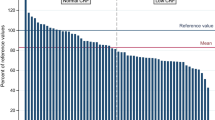
65 RA patients (71% female) successfully completed the Siconolfi step test (mean ± SD; age 58 ± 11 years; disease duration 10 ± 8 years). Predicted CRF was 22.0 ± 5.9 ml kg−1 min−1 for the entire cohort and 20.3 ± 4.8 ml kg−1 min−1 and 26.3 ± 6.2 ml kg−1 min−1 for females and males, respectively.
RA patients were categorised as overweight (BMI > 25). 65% of RA patients were overweight or obese according to their body fat percent and the prevalence of being overweight or obese was higher in female RA patients (70%) compared to males (53%).
RA patients had well-controlled disease with low levels of inflammation (ESR = 12.0 mm h−1; CRP = 4.0 mg l−1), disease activity (DAS 28 CRP = 2.2) and disability (HAQ = 0.5). See Table 1. Patients were treated with disease-modifying anti-rheumatic drugs (DMARDs) including methotrexate (66%), leflunomide (18%), sulphasalazine (14%) and hydroxychloroquine (9%) and biologic therapy (23%). 57% of patients were receiving monotherapy, 37% of patients were receiving combination therapy and 6% of patients were not being treated with DMARDs.
Global CVD risk was moderate to high (16.3%). 35% of patients were classified as having metabolic syndrome based on the clustering of risk factors (abdominal obesity, hyperglycaemia, low high-density lipoprotein cholesterol (HDL-c), high triglycerides (TG) and hypertension). According to the NCEP Adult treatment Panel (ATP III), a diagnosis of metabolic syndrome requires at least three of the five criteria [25].
Correlation/regression analysis
CRF inversely correlated with diastolic blood pressure (DBP) and global CVD risk score but not with any other CVD risk factors, see Table 2.
No significant associations were observed between CRF and family history of heart disease (OR = 1.06, 95% CI = 0.96–1.17; p = 0.275), diabetes (OR = 1.07, 95% CI = 0.93–1.24; p = 0.321), hypertension (OR = 1.08, 95% CI = 0.98–1.18; p = 0.112), dyslipidemia (OR = 1.08, 95% CI = 0.98–1.19; p = 0.105), smoking status (OR = 0.94, 95% CI = 0.86–1.04; p = 0.212), or metabolic syndrome (OR = 1.07, 95% CI = 0.97–1.18; p = 0.172).
CRF inversely correlated with all body composition measures (weight, BMI, body fat percent, waist circumference, hip circumference and waist:hip) when adjusting for age and gender (see Table 2). Waist circumference was most strongly associated with CRF.
CRF was 24% lower in obese patients compared to non-obese (19.1 ± 4.9 ml kg−1 min−1 versus 23.7 ± 5.8 ml kg−1 min−1, p = 0.002). Obesity remained a significant and independent predictor of CRF using ANCOVA, with age, gender and disease duration as covariates, (F1, 60 = 8.3; p < 0.01).
For RA disease variables, CRF correlated significantly with HAQ scores with better CRF associated with less reported disability. CRF did not correlate with any other RA disease factors (see Table 2).
Hierarchical multiple regression assessed the ability of three measures (DBP, body fat percent and HAQ) to predict level of CRF. DBP was entered at step 1, explaining 10.3% of variance in CRF (R2 change 0.103). After entry of body fat percent at step 2, the total variance explained by the model was 39% (F (2,62) = 19.81, p < 0.001). Body fat percent explained an additional 28.7% of the variance in CRF, after controlling for DBP (R2 change 0.287). After entry of HAQ at step 3, the total variance explained by the model was 40.2% (F (3,61) = 13.65, p < 0.001). In the final model, only DBP (beta − 0.29, p < 0.01) and body fat percent (beta − 0.53, p < 0.001) were significant predictors of CRF.
Longitudinal study
Of the 65 patients assessed in the cross-sectional study, 10 patients (8 females; age 64 ± 6 years; disease duration 11 ± 12 years) agreed to participate and completed 8 weeks of exercise. Compliance to training was excellent and participants completed on average 22 sessions (range 17–24). Results are displayed in Table 3.
CRF improved significantly after the exercise programme (p = 0.021). Relative to baseline, fitness improved by 13%, lower body strength improved by 54% and agility improved by 17%. SBP decreased by 7 mmHg (p = 0.021). There were no changes in fasting lipids or glucose, LDL-c increased by 0.2 mmol l−1 but remained within normal range. Body fat decreased by 9%, waist circumference by 2% and hip circumference decreased by 3% with an overall reduction in total weight (1.4 kg) and BMI (0.6 kg m−2). There was no change in inflammation, however, disease activity, pain, HAQ, fatigue and QoL improved significantly.
Discussion
The present study revealed that in patients with RA, DBP and body composition (specifically body fat, waist and hip circumference) were the strongest predictors of CRF as measured by the validated Siconolfi step test. Further, an 8-week exercise intervention revealed improvement in CRF and physical function, several classical CVD risk factors and RA factors. Collectively, these findings suggest that CRF is an important determinant of CVD risk and warrants inclusion in the routine assessment of RA patients. The present study also suggests that regular exercise can improve CVD risk, RA disease and general wellbeing and thus should be prescribed as part of routine care.
The assessment of CRF using the previously validated Siconolfi step test supports our previous findings about the low CRF of RA patients (22 ml kg−1 min−1). Importantly, poor CRF was associated with higher DBP, higher global CVD risk and worse body composition profile. Patients with low CRF tended to be heavier, fatter and had a larger waist and hip circumference. The strong association between CRF and body composition is partially explained by the inclusion of body weight in the CRF calculation. However, despite this, these results remain consistent with previous findings [14, 26, 27]. The present study shows that CRF is significantly lower (24%) in patients that are classified as obese, even after controlling for age, gender and disease duration.
Previous research suggests that physically active RA patients have lower SBP, better lipid profiles and favourable body composition when compared to physically inactive patients [4] and that these positive effects are mediated by higher CRF [14]. Interestingly, regardless of fitness level, it has also been shown that individuals with higher visceral adipose tissue also have higher blood pressure [28]. The results of the present study suggest that the association between poor CRF and high DBP may be due to individuals who are less fit also having higher levels of body fat. The exact biological mechanism for this observation is unclear, however, it is possible that the increased production of proinflammatory cytokines from visceral adipose tissue [29] directly injures the vascular endothelium, subsequently increasing blood pressure [30]. In addition, the abnormal production of proinflammatory cytokines derived from metabolically active fat may also be exacerbated by the inflammatory nature of RA disease itself [31]. Interestingly, a sub-analysis of the present study provides support for this hypothesis, patients who were classified as having a high waist circumference (≥ 88 cm for females, ≥ 102 cm for males) did have significantly higher DBP (p = 0.042). Systolic blood pressure was on average higher for individuals with a high waist circumference, but this was not statistically significant.
There is a large body of evidence that suggests regular exercise is beneficial to RA patients [32]. Regular aerobic and muscle strengthening exercise have been shown to improve CRF [15, 33, 34], muscle strength [35, 36], body composition [15, 37, 38] and CVD risk factors [15]. Importantly, these benefits are all achieved without any exacerbation of disease activity. The results of the present study show that 8 weeks of supervised exercise offered as part of routine care, not only significantly improves CRF and physical function, but also significantly improves several CVD risk factors which include SBP and body composition. These beneficial effects were all achieved without any exacerbation of disease activity. In fact, 8 weeks of supervised exercise resulted in a significant improvement in disease activity, pain, fatigue and quality of life.
The exercise programme implemented was based on current exercise guidelines [24] and the findings confirm the programme was of sufficient intensity, duration, frequency and progression to elicit positive changes. CRF improved by 13%, indicating a large effect and is consistent with findings from previous research [15, 33, 34]. Lower body strength improved by 54%, this is greater than the 30% improvement reported by Lemmey et al. [35] and the 30.5% reported by Law et al. [39] but is in line with the 59% improvement observed by Matsuda et al. [36], who investigated the beneficial effects of a 6-week home exercise programme. Similarly, Matsuda et al. [36] reported a 25% improvement in agility, whilst patients in the current investigation improved by 17%.
Importantly, 8 weeks of regular exercise resulted in a significant reduction in SBP. Average SBP at baseline was 133 mmHg, which is classified as pre-hypertension, 8 weeks of exercise reduced SBP by 7 mmHg, representing a clinical and large effect [40]. DBP was within normal range at baseline and thus is not surprising that no significant change was observed. Similarly, RA patients had an acceptable lipid profile at baseline and no changes were observed post intervention.
Obesity is a significant contributor to CVD [41], so results of the present cross-sectional study highlights that the level of obesity in the RA population is a cause for concern. However, findings from the longitudinal investigation provide support for an effective strategy for managing this issue. 8 weeks of regular exercise, offered as part of routine care, can significantly improve RA patients’ body composition. The present study suggests that excess adiposity is linked with higher DBP and poor CRF. It could therefore be argued that reducing adiposity is an essential target for treatment. It must be acknowledged that improvements in body composition were achieved without any change in diet. These findings are similar to those reported by previous investigations [15, 37, 38].
Limitations of the present study include the cross-sectional design of the study, meaning no conclusions can be made on the cause and effect of CRF, CVD risk and future cardiovascular health of RA patients. Additionally, patients unable to complete the step test were excluded which suggests the cohort investigated are likely the fittest patients. Despite this, the present study has revealed low CRF and a high prevalence of obesity. A major strength of the current investigation is the addition of the longitudinal investigation. To our knowledge, this is the second study to investigate the beneficial effects of exercise on CVD risk in RA. Our investigation highlights that RA patients can participate in regular exercise and benefit from improvements in cardiovascular health and general wellbeing. However, the longitudinal study is not without limitations. Compared to the cross-sectional study, RA patients’ CVD risk factors, inflammation and disease activity were not markedly elevated at baseline. Thus, the beneficial effects of exercise in patients with more active disease and a worse CVD risk profile remains to be determined. Second, the sample size was small, with no control group, randomisation or blinding. Lastly, the short duration of the longitudinal study means that no conclusions can be made on CRF as measured by the Siconolfi step test and hard outcomes like the future development of CVD in RA. Future research is needed to determine if results from the Siconolfi step test can be used to predict future CVD. Despite these limitations, this study has identified important CVD risk factor targets for treatment and has designed an effective exercise programme that could be offered as part of routine care.
Conclusion
RA patients have poor CRF as assessed by the Siconolfi step test and this is associated with higher DBP, higher global CVD risk and obesity. This investigation highlights the importance of including CRF, as measured by the step test, as an indicator of CVD risk. The present study also shows that regular exercise offered as part of routine care can help improve RA patients overall cardiovascular health, wellbeing and QoL. Future research is required to establish how these improvements can be sustained in patients with a wide range of disease activity and finally, to determine whether or not such a treatment, offered as part of routine care, is financially viable for the national health service.
References
Avina-Zubieta JA, Choi HK, Sadatsafavi M, Etminan M, Esdaile JM, Lacaille D (2008) Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum 59:1690–1697
Kitas GD, Gabriel SE (2011) Cardiovascular disease in rheumatoid arthritis: state of the art and future perspectives. Ann Rheum Dis 70(1):8–14
Lee IM, Sesso HD, Paffenbarger RS Jr (2000) Physical activity and coronary heart disease risk in men: does the duration of exercise episodes predict risk? Circulation 102:981–986
Metsios GS, Stavropoulos-Kalinoglou A, Panoulas VF, Wilson M, Nevill AM, Koutedakis Y, Kitas GD (2009) Association of physical activity with increased cardiovascular risk in patients with rheumatoid arthritis. Eur J Cardiovasc Prev Rehabil 16:188–194
Warren TY, Barry V, Hooker SP, Sui X, Church TS, Blair SN (2010) Sedentary behaviours increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc 42:879–885
Blair SN, Kohl HW 3rd, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW (1989) Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 262:2395–2401
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE (2002) Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346:793–801
Stenstrom CH, Minor MA (2003) Evidence for the benefit of aerobic and strengthening exercise in rheumatoid arthritis. Arthritis Rheum 49:428–434
Minor MA, Hewett JE (1995) Physical fitness and work capacity in women with rheumatoid arthritis. Arthritis Care Res 8:146–154
Cooney JK, Moore JP, Ahmad YA, Jones JG, Lemmey AB, Casanova F, Maddison PJ, Thom JM (2013) A simple step test to estimate cardio-respiratory fitness levels of rheumatoid arthritis patients in a clinical setting. Int J Rheumatol 1:1. https://doi.org/10.1155/2013/174541
McKenzie JA, Witkowski S, Ludlow AT, Roth SM, Hagberg JM (2011) AKT1 G205T genotype influences obesity-related metabolic phenotypes and their responses to aerobic exercise training in older Caucasians. Exp Physiol 96:338–347
Mitros M, Gabriel KP, Ainsworth B, Lee C, Herrmann S, Campbell K, Swan P (2011) Comprehensive evaluation of a single-stage submaximal treadmill walking protocol in healthy, middle-aged women. Eur J Appl Physiol 111:47–56
Schulman SP, Fleg JL, Goldberg AP, Busby-Whitehead J, Hagberg JM, O’Connor FC, Gerstenblith G, Becker LC, Katzel LI, Lakatta LE, Lakatta EG (1996) Continuum of cardiovascular performance across a broad range of fitness levels in healthy older men. Circulation 94:359–367
Metsios GS, Koutedakis Y, Veldhuijzen van Zanten JJCS, Stavropoulos-Kalinoglou A, Vitalis P, Duda JL, Ntoumanis N, Rouse PC, Kitas GD (2015) Cardio-respiratory fitness levels and their association with cardiovascular profile in patients with rheumatoid arthritis: a cross-sectional study. Rheum 54(12):2215–2220
Stavropoulos-Kalinoglou A, Metsios GS, Veldhuijzen van Zanten JJJCS, Nightingale P, Kitas GD, Koutedakis Y (2013) Individualised aerobic and resistance exercise training improves CRF and reduces cardiovascular risk in patients with rheumatoid arthritis. Ann Rheum Dis 72(11):1819–1825
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Fries JF, Spitz P, Kraines RG, Holman HR (1980) Measurement of patient outcome in arthritis. Arthritis Rheum 23(2):137–145
Fransen J, Welsing P, De Keijzer RM, Riel PL (2004) Disease Activity Scores using C-reactive protein: CRP may replace ESR in the assessment of RA disease activity. Ann Rheum Dis 62:151
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, Brindle P (2008) Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 336:1475–1482
Siconolfi SF, Garber CE, Lasater TM, Carleton RA (1985) A simple, valid step test for estimating maximal oxygen uptake in epidemiologic studies. Am J Epidemiol 121:382–390
Jones CJ, Rikli RE (2002) Measuring functional fitness of older adults. J Activ Aging 1:24–30
Ware JE Jr (2000) SF-36 health survey update. Spine 25:3130–3139
Belza BL (1995) Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol 22:639–643
American College of Sports Medicine (2009) ACSM’s guidelines for exercise testing and prescription (8th ed). Lippincott Williams & Wilkins, Philadelphia
National Cholesterol Education Program (NCEP) (2002) Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
Fogelholm M, Malmberg J, Suni J, Santtila M, Kyrolainen H, Mantysaari M (2006) Waist circumference and BMI are independently associated with the variation of cardio-respiratory and neuromuscular fitness in young adult men. Int J Obes 30:962–969
Wong SL, Katzmarzyk P, Nichaman MZ, Church TS, Blair SN, Ross R (2004) CRF is associated with lower abdominal fat independent of body mass index. Med Sci Sports Exerc 36:286–291
Rheaume C, Arsenault BJ, Belanger S, Perusse L, Tremblay A, Bouchard C, Poirier P, Despres JP (2009) Low CRF levels and elevated blood pressure: what is the contribution of visceral adiposity? Hypertension 54:91–97
Bray GA, Bellanger T (2006) Epidemiology, trends, and morbidities of obesity and the metabolic syndrome. Endocrine 29:109–117
Despres JP (2001) Health consequences of visceral obesity. Ann Med 33:534–541
Sattar N, McCarey DW, Capell H, McInnes IB (2003) Explaining how “high-grade” systemic inflammation accelerates vascular risk in rheumatoid arthritis. Circulation 108:2957–2963
Cooney JK, Law RJ, Matschke V, Lemmey AB, Moore JP, Ahmad Y, Jones JG, Maddison P, Thom J (2011) Benefits of exercise in rheumatoid arthritis. J Aging Res 1:1. https://doi.org/10.4061/2011/681640
Breedland I, van Scheppingen C, Leijsma M, Verheij-Jansen NP, van Weert E (2011) Effects of a group-based exercise and educational program on physical performance and disease self-management in rheumatoid arthritis: a randomized controlled study. Phys Ther 91:879–893
Neuberger GB, Aaronson LS, Gajewski B, Embretson SE, Cagle PE, Loudon JK, Miller PA (2007) Predictors of exercise and effects of exercise on symptoms, function, aerobic fitness, and disease outcomes of rheumatoid arthritis. Arthritis Rheum 57:943–952
Lemmey AB, Marcora SM, Chester K, Wilson S, Casanova F, Maddison PJ (2009) Effects of high-intensity resistance training in patients with rheumatoid arthritis: a randomized controlled trial. Arthritis Rheum 61:1726–1734
Matsuda PN, Shumway-Cook A, Ciol MA (2010) The effects of a home-based exercise program on physical function in frail older adults. J Geriatr Phys Ther 33:78–84
Dekker MJ, Lee S, Hudson R, Kilpatrick K, Graham TE, Ross R, Robinson LE (2007) An exercise intervention without weight loss decreases circulating interleukin-6 in lean and obese men with and without type 2 diabetes mellitus. Metabolism 56:332–338
Lim JY, Tchai E, Jang SN (2010) Effectiveness of aquatic exercise for obese patients with knee osteoarthritis: a randomized controlled trial. PMR 2:723–731
Law R-J, Saynor ZL, Gabbitas J, Jones J, Kraus A, Breslin A, Maddison PJ, Thom JM (2015) The effects of aerobic and resistance exercise on markers of large joint health in stable rheumatoid arthritis patients: a pilot study. Musculoskelet Care 13:222–235
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Erlbaum, Hillsdale
Ritchie SA, Connell JM (2007) The link between abdominal obesity, metabolic syndrome and cardiovascular disease. Nutr Metab Cadiovasc Dis 17(4):319–326
Acknowledgements
This investigation was funded by the Welsh Assembly Government (HST08-004). The authors would like to thank the patients and staff of the Rheumatology Service at Betsi Cadwaladr University Health Board (West) for their assistance in conducting this study.
Author information
Authors and Affiliations
Contributions
JC, JT YA and JM secured funding for the project. JT, YA and JM supervised the project. JC led the project, assessed participants and analysed the data. JC and AS interpreted the data and drafted the manuscript. All authors read and approved the final manuscript and take full responsibility for the integrity of the study and the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Cooney, J.K., Ahmad, Y.A., Moore, J.P., Sandoo, A., Thom, J.M. declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work formed part of a PhD Thesis and the related publication can be found using the following link: http://e.bangor.ac.uk/5150/1/PhD%20Thesis%202012%20-%20Jennifer%20Cooney.pdf.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Cooney, J.K., Ahmad, Y.A., Moore, J.P. et al. The impact of cardiorespiratory fitness on classical cardiovascular disease risk factors in rheumatoid arthritis: a cross-sectional and longitudinal study. Rheumatol Int 39, 1759–1766 (2019). https://doi.org/10.1007/s00296-019-04431-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-019-04431-4