Abstract
Assessment of disease activity in Takayasu arteritis (TA) is challenging. We aimed to study utility of serum amyloid A (SAA) to assess disease activity and its association with SAA gene polymorphisms, if any, in our TA patients. Serum of 99 consecutive adult TA patients and 40 healthy controls were assayed for SAA. Depending on the ITAS2010 and ITAS-CRP score, patients were designated as having active disease if ITAS2010 ≥ 2 or ITAS-CRP ≥ 3 and stable disease if ITAS2010 = 0 or ITAS-CRP is ≤1. Clinical ITAS of 0 with raised inflammatory markers scoring a ITAS-CRP of 2 was considered as indeterminate for disease activity assessment. Repeat SAA levels for active group was measured after 6 months from baseline. SAA levels between active and stable disease as well as serial levels were compared. DNA of 40 patients and controls were genotyped for SAA polymorphisms (rs12218, rs2468844) and the allele frequencies were compared. At baseline, SAA levels were higher in patients as compared to controls (137.4 vs 100.8 ng/ml, p = 0.001) and higher in patients with active disease (166.4 ng/ml) than those with stable disease (98.2 ng/ml), p = 0.001. SAA decreased during follow-up in treatment responders (189.9 ng/ml at baseline vs 119.0 ng/ml at follow-up, p = 0.008); in contrast, there was no significant change among non-responders during follow-up. Allelic frequencies of SAA gene polymorphisms did not differ between cases and controls. SAA may be a reliable biomarker to assess disease activity and treatment response in TA.




Similar content being viewed by others
References
Kerr GS, Hallahan CW, Giordano J, Leavitt RY, Fauci AS, Rottem M et al (1994) Takayasu arteritis. Ann Intern Med 120(11):919–929
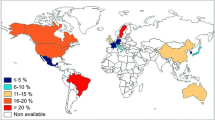
Sharma BK, Sagar S, Singh AP, Suri S. Takayasu arteritis in India. Heart Vessels 7(1):37–43
Direskeneli H, Aydin SZ, Merkel PA (2011) Assessment of disease activity and progression in Takayasu’s arteritis. Clin Exp Rheumatol 29(1 Suppl 64):S86–S91
Direskeneli H, Aydın SZ, Merkel PA (2013) Disease assessment in Takayasu’s arteritis. Rheumatology 16(ket27):4
Keser G, Direskeneli H, Aksu K (2013) Management of Takayasu arteritis: a systematic review. Rheumatology ket320
Ishihara T, Haraguchi G, Tezuka D, Kamiishi T, Inagaki H, Isobe M (2013) Diagnosis and assessment of Takayasu arteritis by multiple biomarkers. Circ J 77(2):477–483
O’Connor TE, Carpenter HE, Bidari S, Waters MF, Hedna VS (2014) Role of inflammatory markers in Takayasu arteritis disease monitoring. BMC Neurol 28(14):62
Salvarani C, Cantini F, Boiardi L, Hunder GG (2003) Laboratory investigations useful in giant cell arteritis and Takayasu’s arteritis. Clin Exp Rheumatol 21(6; SUPP/32):S23–S28
Matsuyama A, Sakai N, Ishigami M, Hiraoka H, Kashine S, Hirata A et al (2003) Matrix metalloproteinases as novel disease markers in Takayasu arteritis. Circulation 108(12):1469–1473
Urieli-Shoval S, Linke RP, Matzner Y (2000) Expression and function of serum amyloid A, a major acute-phase protein, in normal and disease states. Curr Opin Hematol 7(1):64–69
Ma J, Luo X, Wu Q, Chen Z, Kou L, Wang H (2010) Circulation levels of acute phase proteins in patients with Takayasu arteritis. J Vasc Surg 51(3):700–706
O’Neill L, Rooney P, Molloy D, Connolly M, McCormick J, McCarthy G et al (2015) Regulation of inflammation and angiogenesis in giant cell arteritis by acute-phase serum amyloid A. Arthritis Rheumatol Hoboken NJ 67(9):2447–2456
Vitale A, Rigante D, Lopalco G, Brizi MG, Caso F, Franceschini R et al (2014) Serum amyloid-A in Behçet’s disease. Clin Rheumatol 33(8):1165–1167
Bargagli E, Magi B, Olivieri C, Bianchi N, Landi C, Rottoli P (2011) Analysis of serum amyloid A in sarcoidosis patients. Respir Med 105(5):775–780
Chen ES, Song Z, Willett MH, Heine S, Yung RC, Liu MC et al (2010) Serum amyloid A regulates granulomatous inflammation in sarcoidosis through toll-like receptor-2. Am J Respir Crit Care Med 181(4):360–373
Eklund KK, Niemi K, Kovanen PT (2012) Immune functions of serum amyloid A. Crit Rev Immunol 32(4):335–348
Betts JC, Edbrooke MR, Thakker RV, Woo P (1991) The human acute-phase serum amyloid A gene family: structure, evolution and expression in hepatoma cells. Scand J Immunol 34(4):471–482
Xie X, Ma Y-T, Yang Y-N, Fu Z-Y, Li X-M, Huang D et al (2010) Polymorphisms in the SAA1/2 gene are associated with carotid intima media thickness in healthy Han Chinese subjects: the cardiovascular risk survey. Bochdanovits Z, editor. PLoS One 5(11):e13997
Carty CL, Heagerty P, Heckbert SR, Enquobahrie DA, Jarvik GP, Davis S et al (2009) Association of genetic variation in serum amyloid-A with cardiovascular disease and interactions with the IL6, IL1RN, IL1β and TNF genes in the Cardiovascular Health Study. J Atheroscler Thromb 16(4):419–430
Koga T, Nishino Y, Makiyama J, Hayashida T, Miyashita T, Izumi Y et al (2009) Serum amyloid A is a useful marker to evaluate the disease activity of Takayasu’s arteritis. Rheumatol Int 30(4):561–563
Acknowledgements
This project has been funded by the institutional intramural Grant obtained from Christian Medical College, Vellore. The authors would like to thank Mr. Bijesh Yadav for his contribution to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nair, A.M., Goel, R., Hindhumati, M. et al. Serum amyloid A as a marker of disease activity and treatment response in Takayasu arteritis. Rheumatol Int 37, 1643–1649 (2017). https://doi.org/10.1007/s00296-017-3786-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-017-3786-2